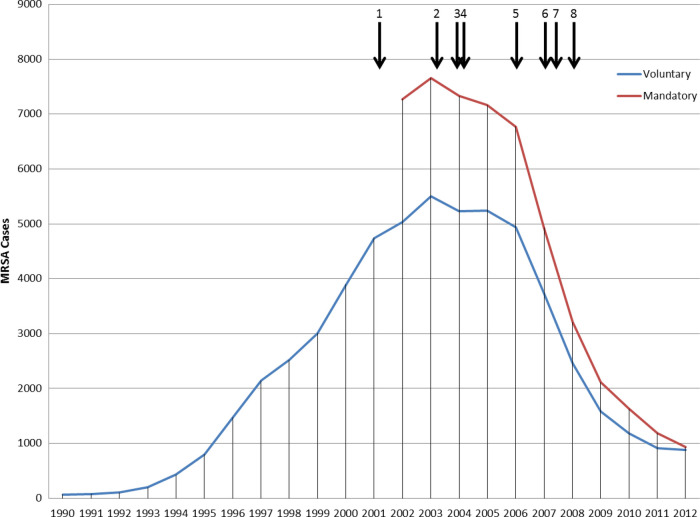
Figure 1.
Numbers of methicillin-resistant Staphylococcus aureus (MRSA) blood stream infections (BSIs) reported in England, 1990–2012. Vertical arrows indicate notable interventions aimed at reducing MRSA BSIs: 1, introduction of mandatory reporting of MRSA BSIs; 2, launch of national report targeting 7 key areas for improvement (active surveillance and investigation, infection risks associated with medical devices, reservoirs of infection, standards of hygiene in clinical practice, prudent use of antimicrobials, management and organization, and research and development; 3, launch of the cleanyourhands campaign to improve the standard of hand hygiene, which required alcohol hand gel to be available, as a minimum, at all points of patient contact; 4, launch of MRSA/Cleaner Hospitals Improvement Programme and, in November 2004, announcement of mandatory target to halve the number of MRSA BSIs in hospitals in England by 2008; 5, legislation was introduced in 2006, which implemented a statutory Code of Practice on healthcare-associated infection (HCAI) that applied to all National Health Service (NHS) healthcare providers; 6, in late 2007 a series of additional measures was added, including a requirement for quarterly reporting on HCAIs to hospital Boards, an extension of the cleanyourhands campaign, and a legal requirement for hospital Chief Executives to report MRSA BSIs (and Clostridium difficile infections) centrally more frequently (within 2 weeks of each following month); 7, start of significant reductions in cephalosporin and fluoroquinolone prescribing in hospitals; 8, MRSA screening implementation guidance was issued during 2008, stating that screening of elective and emergency admissions should be occurring by March 2009 and December 2010, respectively.