Figure 1.
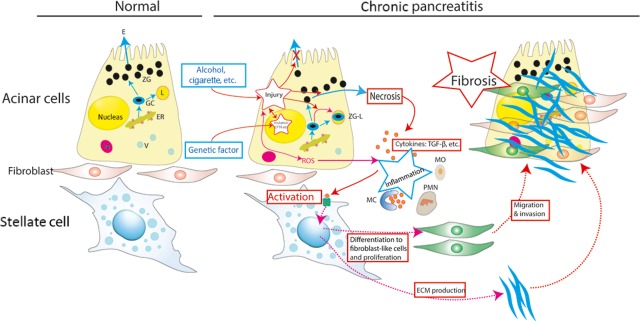
Current concept of the pathogenesis of chronic pancreatitis. An acinar cell is susceptible to autodigestive injury for both genetic and environmental causes. In the presence of an appropriate trigger factor, overt acinar cell injury is initiated. These events result in inflammation. A pancreatic stellate cell (PSC) is activated by cytokines released during pancreatic inflammation, leading to excessive ECM production. The PSCs then proliferate, migrate, invade, and differentiate to fibroblast-like cells. Activation of stellate cells is increased by cytokines from infiltrating leucocytes and the injured acinar cell; thus, fibrosis is shown. The end stage of chronic pancreatitis is identified by loss of all secretory tissues, disappearance of inflammatory cells, and severe fibrosis. ER, endoplasmic reticulum; ZG, zymogen granules; GC, Golgi complex; E, trypsinogen, and other precursor proteases; ROS, reactive oxygen species, L, lysosomes; ZG-L, miniscule fraction of zymogens activated by co-localization with lysosomal enzymes; MC, mast cell; PMN, polymorphonuclear cell; MO, monocyte; V, Vesicle; and ECM, extracellular matrix protein.
