Abstract
Introduction
This study investigates the relationship between gender, the likelihood of discharge from institutional long-term care (LTC) facilities, and post-discharge living arrangements, highlighting sociodemographic, health, socioeconomic, and family characteristics.
Methods
We use the Health and Retirement Study to examine individuals age 65 and older admitted to LTC facilities between 2000 and 2010 (N=3,351). We examine discharge patterns using survival analyses that account for the competing risk of death and estimate the probabilities of post-discharge living arrangements using multinomial logistic regression models.
Results
Women are more likely than men to be discharged from LTC facilities during the first year of stay. Women are more likely to live alone or with kin after discharge, whereas men are more likely to live with a spouse or transfer to another institution. Gender differences in the availability and use of family support may partly account for the gender disparity of LTC discharge and post-discharge living arrangements.
Conclusion
Our findings suggest that women and men follow distinct pathways after LTC discharge. As local and federal efforts begin to place more emphasis on the transition from LTC facilities to prior communities (e.g., transitional care initiatives under the Patient Protection and Affordable Care Act), policymakers should take these gender differences into account in the design of community-transition programs.
Introduction
As more individuals live longer with chronic illness and disabilities (Freedman et al., 2013), the need for acute and long-term care (LTC) will inevitably increase. Researchers project that by 2040 the number of frail Americans age 65 and older will more than double and related LTC expenditures almost triple from their 2000 level (Johnson, Toohey, & Wiener, 2007; Zeng, Land, Gu, & Wang, 2014), while almost 70 percent of the population 65 and older is expected to need LTC at some point over the rest of their lives (Feder & Komisar, 2012). This need will likely differ by gender, as women are more likely than men to require LTC and for longer durations (Feder & Komisar, 2012). Supporting this projection, a recent study examining the expectations of Baby Boomers regarding their future need for long-term supports and services found that one-fourth of them consider it likely that they will move into a nursing home and almost half of them expect to live in an assisted living facility, with women markedly more likely than men to expect to live in these LTC facilities (Robison, Shugrue, Fortinsky, & Gruman, 2014). Despite such expectations, research shows that older individuals whose health conditions require LTC prefer living in the community (Chapin, Baca, Macmillan, Rachlin, & Zimmerman, 2009; Reinhard, 2010). Further, institutional care is expensive, and as such the government has become increasingly engaged with efforts to contain the growth of spending for LTC (James, Wiley, & Fries, 2007; Lakdawalla et al., 2003; Thomas, Gassoumis, & Wilber, 2010). Helping older adults transition from an LTC facility to the community is a potentially effective strategy in controlling this spending and supporting individual preferences (Arling, Kane, Cooke, & Lewis, 2010).
Given this context, it is important to understand older individuals' community transitions and patterns of discharge from LTC (Thomas et al., 2010). There is a particular need to identify characteristics of patients who transition from an LTC facility to the community, specifically whether they are likely to live alone. Living alone is a leading factor for frequent changes in informal care (Allen, Lima, Goldscheider, & Roy, 2012) and readmission into formal care (Strunin, Stone, & Jack, 2007), which both are associated with high financial costs for individuals, their families, and the healthcare system. Since a growing body of literature suggests that gender may be an important determinant of LTC use (Akamigbo & Wolinsky, 2007; Wallace, Levy-Storms, Kington, & Andersen, 1998; Wattmo, Wallin, Londos, & Minthon, 2011), it is especially useful to examine the relationship of gender with discharge from LTC facilities and post-discharge living arrangements. Understanding how gender and related factors may be associated with longer LTC stays and higher likelihoods of living alone following an LTC facility discharge is critical for crafting effective health policy.
In this study, we analyze the Health and Retirement Study (HRS) to identify the ways in which gender influences likelihood of discharge from LTC facilities, length of stay in LTC facilities, and post-discharge living arrangements. We consider the importance of health factors, sociodemographic characteristics, socioeconomic resources, and family-support network characteristics in shaping each of these outcomes. We distinguish between short-term stays (e.g., post-acute or rehabilitative) and long-term stays (e.g., custodial care), a distinction especially important in light of the changing profile of LTC patients who are increasingly requiring skilled post-acute and rehabilitative care instead of custodial care (Gassoumis, Fike, Rahman, Enguidanos, & Wilber, 2013).
Conceptual Model
To explore gender differences in discharge from LTC facilities and post-discharge living arrangements, we use Andersen's behavioral model of health care use (Andersen, 1995; Andersen, McCutcheon, Aday, Chiu, & Bell, 1983), which links health care seeking to predisposing characteristics, enabling resources, and need factors. This organizing framework has guided the study of various aspects of long-term care, including nursing home use (Thomeer, Mudrazija, & Angel, 2014), discharge to community (Thomas et al., 2010), readmission (Howell, Silberberg, Quinn, & Lucas, 2007), and LTC planning (Robison et al., 2014). Thus, in the context of transitional care, it is particularly important to explore whether various sociodemographic (i.e., predisposing) factors, socioeconomic and family (i.e., enabling) factors, and health and functioning (i.e., need) factors operate differently for women and men in shaping their likelihood of discharge and post-discharge living patterns, taking into account the duration of their institutional stay.
Previous research shows that nursing home discharge is largely a function of health needs (Mehr, Williams, & Fries, 1997; Murtaugh, 1994; Thomas et al., 2010), and women tend to have greater health needs than men (Case & Paxson, 2005). In addition to need factors, however, several predisposing and enabling characteristics of nursing home residents are also found to be importantly related to discharge and post-discharge living arrangements. For example, younger age and higher use of rehabilitation services are positively associated with nursing home discharge (Mehr et al., 1997). The family is also important, and studies have established that family ties are positively associated with discharge from the formal care system to prior communities (Arling et al., 2010; Penrod, Kane, & Kane, 2000). Family availability varies importantly by gender. Among the population age 85 and older, around 29 percent of men and 56 percent of women live alone (Crescioni, Gorina, Bilheimer, & Gillum, 2010), and 54 percent of men and 17 percent of women are married (U.S. Census Bureau, 2011). This suggests that women are less likely than men to have partners able to provide them with informal care. On the other hand, studies of intergenerational family relationships suggest that the relationships between mothers and their children, daughters in particular, are stronger (e.g., more social and financial support) than the relationships between fathers and children (Bengtson, 2001; Fritzell & Lennartsson, 2005; Ingersoll-Dayton, Starrels, & Dowler, 1996; Suitor & Pillemer, 2006). Thus, studies find that grown children decrease the need for nursing home care use more so for mothers than for fathers (Freedman, Berkman, Rapp, & Ostfeld, 1994; Noël-Miller, 2010). However, studies have neither considered how gender is linked to likelihood of LTC facility discharge, length of stay, and post-discharge living arrangements, nor how these associations between gender and discharge and post-discharge living arrangements are related to predisposing, need-based, and enabling factors, especially the family. The goal of the current study is to address these research gaps.
Data and Methods
Data come from the Health and Retirement Study (HRS), a nationally representative biennial longitudinal survey of over 26,000 Americans age 51 and above and their spouses. The HRS offers detailed information on respondents' health, health insurance coverage, socioeconomic status, family ties, household composition, LTC use, and post-LTC living arrangements. The analytic sample consists of 3,351 respondents age 65 and older first admitted to LTC facilities between 2000 and 2010. Approximately 10 percent of the sample has missing values on at least one predictor that are imputed in a multiple-imputation procedure. Respondents with missing information are on average two years older than the rest of the sample and therefore somewhat more likely to die in an LTC facility, but they do not significantly differ from other respondents otherwise.
Variables
Dependent Variables
In the HRS, LTC facilities primarily refer to nursing homes, but they also include convalescent homes and other long-term health care facilities that provide continuing nursing care such as skilled nursing facilities, but excluding hospices.1
Our outcomes of interest are: (1) the probability of discharge from a long-term health care facility and (2) post-discharge living arrangements for the subset of discharged individuals. The first outcome measure is ascertained by subtracting the respondent's birth year and month from the year and month of nursing home admission to define the age at the onset of the period when discharge may occur, and subtracting the respondent's birth year and month from the year and month of LTC facility discharge to define the age at the time of discharge. The analysis focuses on first discharge because the initial stay in a facility such as a nursing home marks the onset of reliance on the formal LTC system (Freedman, 1996). For the second outcome of interest, post-discharge living arrangement, we distinguish between non-community and community discharge. Options in discharge placement are coded as: (1) non-community living (e.g., retirement center, another nursing home, hospital, or rehab center), (2) living alone, (3) living with spouse only, and (4) living with others, such as child and child's family, or other relatives.
Independent Variables
Predisposing factors (sociodemographics)
The main predictor variable is gender (man or woman). In addition to gender, other important predisposing factors in the model include race/ethnicity (non-Hispanic white, non-Hispanic black, or Hispanic), age, and education (less than a high school education or more than a high school education).
Enabling factors (family support network and socioeconomic resources)
Family support network control variables include marital status (currently partnered/married or currently unpartnered/unmarried), household size, any living children, and any living siblings. Household size is a count variable of all household members including the respondent. In the models of post-discharge living arrangements, we exclude the measures of household size and marital status given that the models are used to define the outcome categories of living alone, living with spouse/partner, and living with others. Socioeconomic resource variables include homeownership (respondent owns home or respondent does not own home), log value of total annual income, and an indicator of Medicaid coverage (respondent covered by Medicaid or respondent not covered by Medicaid).
Need factors (health and health services)
Health services include use of home health services, special facilities/services, and hospitals. All health services variables are indicator variables with the value of 1 assigned if a service has been used at any time in the two years prior to the interview. Home health services refer to any help received at home by professionally trained medical personnel. The use of special facilities/services refers to the use of adult care centers, social workers, outpatient rehabilitation programs, physical therapy or transportation for elderly and/or disabled while the use of hospitals is limited to overnight stays only. Health controls include chronic conditions, activities of daily living (ADL) difficulties, cognition, and depressive symptoms. Chronic condition variables are indicators of having been diagnosed with cancer, heart condition, stroke, and memory-related problems like dementia or Alzheimer's disease (in each case, “yes” is coded as 1 and “no” as 0).2 The ADL index includes difficulties in respondents' ability to bathe, eat, dress, walk across a room, get out of bed without assistance, and use the toilet, each defined with a “yes” (=1) or “no” (=0) indicator, resulting in a summary score ranging from 0 (i.e., no difficulties with ADLs) to 6 (i.e., difficulties with all ADLs). Cognitive impairment is measured with a total cognition score that ranges from 0 to 35 where higher number indicates better cognition. The overall score is composed of two main subscores: 1) total word recall score, which is derived as a sum of immediate and delayed word recall, each with a 0-10 range, resulting in a 0-20 range for the total word recall, and 2) mental status score that includes the number of correct subtractions in the Serial Sevens Test (ranging from 0 to 5), correct date naming (with 0-4 range), and backward counting, object naming, and President/Vice-President naming, respectively, each with a 0-2 range.3 Finally, the measure of depressive symptoms is defined as a score ranging from 0 to 8, with higher score indicating more reported depressive symptoms. The score summarizes responses to the following eight Center for Epidemiological Studies Depression Scale (CES-D) items asked of respondents about the period in the week prior to the interview, each assigned a value of 1 for a “yes” response and 0 for a “no” response: feeling depressed, everything an effort, sleep was restless, felt happy, felt lonely, felt sad, could not get going, and enjoyed life.4
Analysis
The analysis begins with a gendered overview of sample characteristics of nursing home residents. Next, we fit a competing-risk regression of LTC facility discharge. As death is a competing event that can impede the occurrence of a discharge, competing-risk regression takes this information into account and produces appropriate estimates. The model is partitioned by the duration of institutional stay to short- and long-term stays using two alternative cutoff points, namely, one month and three months, to examine whether and how the variation in the definition of short- and long-term stay affects the findings. While the existing LTC financing policies are mostly consistent with the use of a three-month cutoff point, certain administrative rules (Centers for Medicare and Medicaid Services, 2012) and previous research (e.g., Howell et al., 2007) suggest a one-month cutoff point may be more appropriate. We stratify models of LTC facility discharge by gender in order to test whether the underlying processes explaining discharge significantly differ between women and men. Supplementary analyses (not shown), using multiple interaction terms of gender with other covariates, confirm that these stratified gender differences are statistically significant. For the analysis of post-discharge living arrangements, we specify a multinomial logistic regression distinguishing between individuals who transfer to another formal LTC institution, live alone or live with family. The model is stratified by the duration of stay.
Results and Discussion
Almost two thirds of nursing home residents in our sample are women (2066 women compared to 1285 men), as shown in Table 1. They are more likely to be discharged from an LTC facility despite being on average older than men, less likely to have a living spouse or siblings, and less economically advantaged (i.e., lower incomes and homeownership rates) than their male counterparts. Moreover, women and men exhibit similar health outcomes, although men report a somewhat higher prevalence of cancer, stroke, and heart conditions while women experience more depressive symptoms and ADL difficulties.
Table 1. Sample means, by gender a,b.
| Men | Women | |
|---|---|---|
| Discharged from LTC facility | 0.58 | 0.65 *** |
| Predisposing factors | ||
| Race | ||
| Non-Hispanic white | 0.90 | 0.90 |
| Non-Hispanic black | 0.07 | 0.07 |
| Hispanic | 0.03 | 0.03 |
| Age | 81.09 | 82.42 *** |
| Less than high school | 0.32 | 0.34 |
| Enabling factors | ||
| Married/partnered | 0.59 | 0.24 *** |
| Household size (1-11) c | 1.91 | 1.69 *** |
| Any living children | 0.91 | 0.90 + |
| Any living siblings | 0.71 | 0.66 ** |
| Homeownership | 0.70 | 0.55 *** |
| Annual income (in $) | 37072 | 28774 *** |
| Any Medicaid | 0.12 | 0.19 *** |
| Need factors | ||
| Home health services | 0.39 | 0.47 *** |
| Special facility or service | 0.27 | 0.30 + |
| Hospital overnight | 0.73 | 0.77 * |
| Cancer | 0.27 | 0.22 ** |
| Heart condition | 0.53 | 0.46 *** |
| Stroke | 0.26 | 0.24 * |
| Memory problems | 0.17 | 0.18 |
| ADL disability (0-6) d | 1.68 | 1.90 ** |
| Cognitive impairment (0-35) e | 18.52 | 18.37 |
| Depression (0-8) f | 2.14 | 2.32 *** |
|
| ||
| N | 1285 | 2066 |
p<0.001,
p<0.01,
p<0.05,
p<0.01
The information used in the calculation of sample means reflects the values of variables recorded at the survey wave of first entry into the LTC facility.
All variables are dichotomous (0=no, 1=yes) unless indicated otherwise.
Includes the respondent, that is, the person entering the LTC facility.
Score measuring difficulties in respondents' ability to perform bathing, eating, dressing, walking across a room, getting out of bed without assistance, and using the toilet, and ranging from 0 (i.e., no difficulties with ADLs) to 6 (i.e., difficulties with all ADLs).
Score ranging from 0 to 35 (where higher number indicates better cognition) and includes total word recall score (which is derived as a sum of immediate and delayed word recall, each with a 0-10 range, resulting in a 0-20 range for the total word recall) and mental status score (with a 0-15 range, that consists of the number of correct subtractions in the Serial Sevens Test with scores ranging from 0 to 5, correct naming of date including the day of month, month, year, and day of week (0-4 range), and backward counting, object naming, and President/Vice-President naming, each with a 0-2 range).
Score based on the following Center for Epidemiological Studies Depression Scale (CES-D) items asked of respondents about the period in the week prior to the interview: feeling depressed, everything an effort, sleep was restless, felt happy, felt lonely, felt sad, could not get going, and enjoyed life.
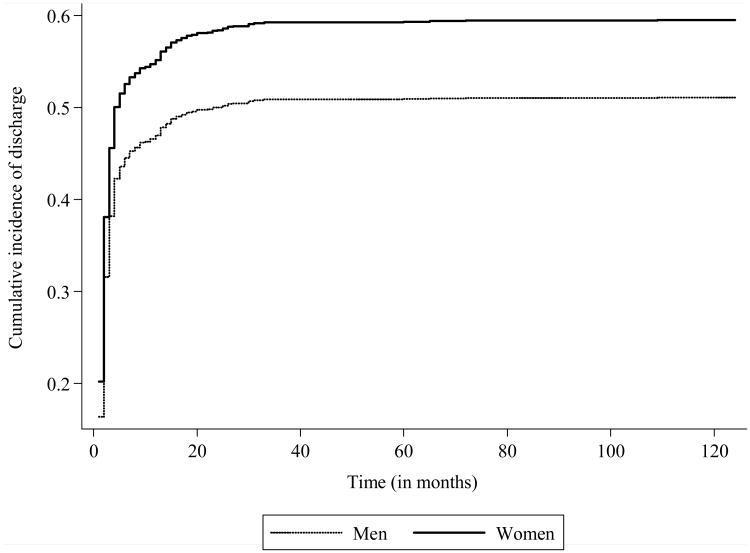
Figure 1 presents cumulative incidence of discharge from an LTC facility for women and men. This suggests that the difference in discharge rates between the two groups emerges mostly within the first two months of LTC facility stay, and in particular within the first month of stay. Past three months, the difference in the cumulative incidence of discharge between women and men appears to remain largely unchanged.
Figure 1. Cumulative incidence of discharge from an LTC facility by gender.
The results of competing-risk survival analysis (Table 2) reveal that, controlling for the risk of death, women are more likely than men to be discharged from an LTC facility for both short- and long-term stays. Subhazard ratio (SHR), that is, the effect that being a woman has on the cumulative incidence of discharge, suggests that women are approximately 17 to 22 percent more likely to be discharged from an LTC facility than men, and the results are fairly constant regardless of the duration of stay.
Table 2. Competing-risk regressions of LTC facility discharge.
| Total sample | Men only | Women only | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <= 1 month | > 1 month | <= 3 months | > 3 months | <= 1 month | > 1 month | <= 3 months | > 3 months | <= 1 month | > 1 month | <= 3 months | > 3 months | |
| Predisposing factors | ||||||||||||
| Women (ref. Men) | 1.17 *** | 1.19 ** | 1.22 *** | 1.19 | ||||||||
| Race (ref. non-Hispanic white) | ||||||||||||
| Non-Hispanic black | 1.06 | 1.10 | 1.03 | 1.21 | 0.96 | 0.91 | 1.00 | 0.89 | 1.12 * | 1.20 + | 1.05 | 1.32 |
| Hispanic | 1.14 * | 0.99 | 1.23 * | 0.95 | 1.41 ** | 0.91 | 1.14 | 1.03 | 1.09 | 1.03 | 1.30 * | 0.90 |
| Age | 1.00 | 0.98 *** | 0.99 * | 0.96 *** | 1.00 | 0.97 *** | 1.00 | 0.95 *** | 0.99 * | 0.98 *** | 0.99 ** | 0.96 *** |
| Less than high school | 0.95 | 0.87 * | 0.97 | 0.68 ** | 0.94 | 0.96 | 0.96 | 0.80 | 0.95 | 0.82 * | 0.97 | 0.62 *** |
| Enabling factors | ||||||||||||
| Married/partnered | 0.96 | 1.01 | 0.98 | 1.02 | 1.00 | 1.20 | 1.04 | 0.92 | 0.95 | 0.91 | 0.92 | 1.08 |
| Household size | 1.03 * | 1.06 + | 1.03 | 1.11 + | 1.06 * | 1.05 | 1.07 + | 1.03 | 1.02 | 1.06 + | 1.02 | 1.14 * |
| Any living children | 1.00 | 1.16 | 1.13 | 1.04 | 1.07 | 1.11 | 1.13 | 1.23 | 0.97 | 1.18 | 1.11 | 0.94 |
| Any living siblings | 1.05 | 1.06 | 1.06 | 1.17 | 1.04 | 1.03 | 1.08 | 1.02 | 1.04 | 1.07 | 1.03 | 1.27 |
| Homeownership | 1.03 | 1.11 + | 1.04 | 0.86 | 1.10 | 1.10 | 1.14 | 0.92 | 1.01 | 1.10 | 0.99 | 0.85 |
| Annual income | 1.02 | 1.04 * | 1.02 | 1.05 + | 1.03 | 1.03 | 1.02 | 1.08 | 1.01 | 1.05 * | 1.03 | 1.04 |
| Any Medicaid | 1.01 | 0.69 *** | 0.96 | 0.64 *** | 1.01 | 0.72 * | 1.06 | 0.64 + | 1.00 | 0.66 *** | 0.91 | 0.63 * |
| Need factors | ||||||||||||
| Home health services | 1.07 + | 1.42 *** | 1.13 ** | 1.66 *** | 1.17 * | 1.47 *** | 1.19 * | 1.72 ** | 1.03 | 1.40 *** | 1.08 + | 1.72 ** |
| Special facility or service | 1.07 * | 1.13 * | 1.10 * | 1.24 + | 1.04 | 1.09 | 1.10 | 1.11 | 1.07 * | 1.14 + | 1.10 * | 1.36 * |
| Hospital overnight | 1.52 *** | 2.81 *** | 2.04 *** | 2.36 *** | 1.36 ** | 2.34 *** | 1.70 *** | 2.14 ** | 1.67 *** | 3.20 *** | 2.38 *** | 2.54 *** |
| Cancer | 0.93 | 1.00 | 0.92 + | 1.04 | 0.91 | 1.12 | 0.93 | 1.34 | 0.94 | 0.94 | 0.91 | 0.91 |
| Heart condition | 1.03 | 0.92 | 0.99 | 0.93 | 0.96 | 0.90 | 0.93 | 0.93 | 1.07 + | 0.93 | 1.02 | 0.93 |
| Stroke | 1.00 | 1.04 | 0.99 | 1.14 | 1.01 | 0.97 | 1.01 | 0.90 | 0.98 | 1.08 | 0.97 | 1.28 + |
| Memory problems | 0.95 | 0.82 ** | 0.99 | 0.84 | 0.84 | 0.73 * | 0.93 | 0.70 | 1.01 | 0.86 | 1.02 | 0.88 |
| ADL disability | 1.01 | 0.91 *** | 1.00 | 0.92 *** | 1.02 | 0.95 * | 1.01 | 0.99 | 1.00 | 0.89 *** | 0.99 | 0.88 *** |
| Cognitive impairment | 1.00 | 1.01 | 1.01 + | 1.01 | 1.00 | 1.00 | 1.01 | 0.99 | 1.00 | 1.01 + | 1.01 | 1.01 |
| Depression | 1.00 | 1.00 | 0.99 | 1.01 | 1.00 | 1.01 | 0.99 | 1.04 | 0.99 | 0.99 | 0.99 | 0.99 |
|
| ||||||||||||
| N | 1096 | 2255 | 2222 | 1129 | 440 | 845 | 879 | 406 | 656 | 1410 | 1343 | 723 |
| Failed | 838 | 1177 | 1681 | 334 | 299 | 433 | 610 | 122 | 539 | 744 | 1071 | 212 |
| Competing risk | 250 | 972 | 522 | 700 | 140 | 369 | 261 | 248 | 110 | 603 | 261 | 452 |
| F-value | 4.59 | 24.3 | 9.47 | 9.48 | 1.89 | 6.88 | 3.34 | 3.39 | 3.04 | 19.21 | 6.56 | 7.76 |
p<0.001,
p<0.01,
p<0.05,
p<0.1
Gender interactions as well as models stratified by gender reveal that the majority of discharge predictors operate similarly for women and men, but the relative importance of some predictors varies by gender. Hispanic origin is strongly predictive of discharge within a month of admission for men only (SHR=1.41), whereas among women non-Hispanic black identity is positively related to discharge for short-term LTC residents. Low education is only predictive of discharge for women with longer duration of stay. Household size is positively associated with short-term LTC facility stays for men and long-term stays for women, particularly if over three months (SHR=1.14). A living spouse or partner is positively associated with discharge for men with a stay over a month (SHR=1.20), although this estimate is just short of being statistically significant. For residents staying longer than a month, ADL difficulties are positively associated with lower chance of discharge for women than men, whereas memory-related problems, including Alzheimer's disease and dementia, are comparatively more significant for men. The use of special facilities or services is positively associated with discharge for women only, and overnight hospital stays are more strongly associated with discharge for women. Except for residents staying over three months, the opposite is true for home health services use.
Once discharged from an LTC facility, former residents either transfer to non-community settings such as retirement centers or nursing homes, or return to the community where they either live alone, with their spouse, or with children, children's families, or other relatives (Table 3). An overwhelming majority (around 80%) of all discharged LTC residents returns to the community, yet among the individuals discharged after stays longer than three months, about 41 percent transfer to non-community settings. The lower proportion of discharged men living with spouses and the lower proportion of women living alone following long-term stay can fully explain the difference of proportion of former LTC residents living in non-community settings following short- and long-term LTC stays. Overall, over one-third of women and almost one-fifth of men live alone after discharge. However, the proportion of women living alone sharply decreases as length of duration of stay in LTC facilities increases (15 percent of long-term residents compared to 38 percent of residents spending less than a month in an LTC facility). Conversely, the proportion of men living alone remains roughly constant regardless of time spent in an LTC facility. This is an important observation in the context of previous findings that living alone is associated with insufficient care, elevated possibility of health deterioration, and increased probability of readmission to the formal-care system (Strunin et al., 2007), especially for individuals discharged from long-term nursing home stays (Howell et al., 2007). Finally, the proportion of women living with children, their families, or other relatives is more than double compared to men regardless of the duration of LTC facility stay, but, conversely, a substantially smaller proportion of women live with their spouses following discharge.
Table 3. Post-discharge living arrangements, by gender and duration of LTC facility stay a.
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Less than a month | 1-3 months | Over 3 months | Total | Less than a month | 1-3 months | Over 3 months | Total | |
|
|
||||||||
| Non-community | 20.4% (58) | 17.6% (54) | 40.7% (46) | 22.4% (158) | 15.9% (81) | 13.5% (69) | 40.8% (78) | 18.8% (228) |
| Alone | 16.8% (48) | 21.2% (65) | 17.7% (20) | 18.9% (133) | 37.8% (192) | 36.5% (187) | 15.2% (29) | 33.7% (408) |
| With spouse | 53.0% (151) | 49.7% (152) | 31.0% (35) | 48.0% (338) | 23.8% (121) | 24.4% (125) | 19.9% (38) | 23.5% (284) |
| With others | 9.8% (28) | 11.4% (35) | 10.6% (12) | 10.7% (75) | 22.4% (114) | 25.6% (131) | 24.1% (46) | 24.0% (291) |
Results expressed as column percentages with the number of observations for each category shown in the brackets.
The results in Table 4 describe the determinants of post-discharge living arrangements based on our multinomial logistic regression. The results reveal that women are more likely than men to live with children and others as opposed to non-community settings, and this finding holds for both short- and long-term former LTC facility residents. They are also substantially more likely to live alone and less likely to live with a spouse following discharge, though only for shorter term LTC stays.
Table 4. Multinomial logistic regression of post-discharge living arrangements.
| Post-discharge living arrangements (ref. non-community location) | <= 1 month | > 1 month | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Alone | With spouse/partner | With others | Alone | With spouse/partner | With others | |
| Predisposing factors | ||||||
| Women (ref. Men) | 2.37 *** | 0.58 * | 2.45 ** | 1.95 *** | 0.86 | 2.84 *** |
| Race (ref. non-Hispanic white) | ||||||
| Non-Hispanic black | 1.89 | 0.80 | 2.71 * | 2.47 ** | 1.57 | 3.95 *** |
| Hispanic | 0.87 | 0.73 | 2.03 | 5.78 * | 8.29 ** | 9.40 ** |
| Age | 1.00 | 0.95 ** | 1.00 | 0.97 * | 0.92 *** | 0.98 |
| Less than high school | 0.71 | 0.88 | 0.72 | 1.37 | 1.63 + | 1.65 * |
| Enabling factors | ||||||
| Any living children | 0.42 + | 1.85 | 1.32 | 0.77 | 1.68 | 1.93 + |
| Any living siblings | 1.50 | 1.54 | 1.05 | 1.06 | 1.02 | 1.00 |
| Homeownership | 1.12 | 3.55 *** | 0.80 | 1.38 | 3.81 *** | 0.90 |
| Log (annual income) | 1.05 | 2.59 + | 1.02 | 1.03 | 1.94 + | 1.00 |
| Any Medicaid | 1.13 | 1.88 | 1.54 | 0.91 | 0.49 * | 1.05 |
| Need factors | ||||||
| Home health services | 2.52 *** | 2.18 ** | 1.94 * | 1.92 ** | 2.28 ** | 1.78 * |
| Special facility or service | 2.48 ** | 2.12 * | 1.80 + | 1.35 | 0.86 | 1.10 |
| Hospital overnight | 3.31 *** | 3.75 *** | 1.41 | 3.97 *** | 3.67 *** | 2.03 * |
| Cancer | 0.72 | 0.60 + | 0.77 | 0.82 | 0.94 | 0.90 |
| Heart condition | 0.45 ** | 0.57 * | 0.58 * | 1.05 | 0.85 | 1.23 |
| Stroke | 1.08 | 1.09 | 1.05 | 0.95 | 1.38 | 1.38 |
| Memory problems | 0.54 | 1.10 | 1.70 | 0.27 *** | 0.40 *** | 0.45 ** |
| ADL disability | 0.81 * | 0.89 | 0.90 | 0.77 *** | 0.93 | 0.93 |
| Cognitive impairment | 1.02 | 0.99 | 1.03 | 1.06 * | 1.02 | 1.03 |
| Depression | 1.05 | 0.98 | 1.02 | 1.02 | 0.94 | 1.02 |
|
| ||||||
| N | 793 | 1122 | ||||
| F-value | 3.63 | 5.33 | ||||
|
| ||||||
| Post-discharge living arrangements (ref. non-community location) | <= 3 months | > 3 months | ||||
|
| ||||||
| Alone | With spouse/partner | With others | Alone | With spouse/partner | With others | |
|
| ||||||
| Predisposing factors | ||||||
| Women (ref. Men) | 2.13 *** | 0.67 * | 2.48 *** | 1.23 | 1.03 | 3.34 ** |
| Race (ref. non-Hispanic white) | ||||||
| Non-Hispanic black | 1.85 * | 0.91 | 2.41 ** | 2.66 | 5.26 * | 16.15 *** |
| Hispanic | 1.67 | 1.56 | 2.79 * | 4.82 | 25.71 * | 24.42 * |
| Age | 1.00 | 0.95 *** | 1.00 | 0.92 ** | 0.90 *** | 0.95 + |
| Less than high school | 0.86 | 1.11 | 0.96 | 1.81 | 1.75 | 1.58 |
| Enabling factors | ||||||
| Any living children | 0.53 + | 1.57 | 1.20 | 0.51 | 1.65 | 4.89 + |
| Any living siblings | 1.26 | 1.21 | 1.07 | 1.35 | 1.45 | 0.89 |
| Homeownership | 1.19 | 3.86 *** | 0.84 | 1.38 | 2.78 * | 0.71 |
| Log (annual income) | 1.01 | 2.43 ** | 0.97 | 1.06 | 1.36 | 1.05 |
| Any Medicaid | 1.06 | 1.10 | 1.25 | 0.80 | 0.22 * | 0.81 |
| Need factors | ||||||
| Home health services | 2.41 *** | 2.26 *** | 2.00 *** | 1.38 | 2.99 * | 1.85 |
| Special facility or service | 1.65 ** | 1.18 | 1.23 | 1.28 | 1.11 | 1.58 |
| Hospital overnight | 3.77 *** | 3.92 *** | 1.69 * | 1.98 | 1.54 | 1.80 |
| Cancer | 0.57 ** | 0.61 * | 0.64 * | 2.78 + | 1.41 | 1.67 |
| Heart condition | 0.74 + | 0.74 + | 0.82 | 0.66 | 0.80 | 2.04 |
| Stroke | 0.98 | 1.21 | 1.16 | 1.01 | 1.37 | 1.67 |
| Memory problems | 0.47 ** | 0.75 | 0.87 | 0.10 *** | 0.25 ** | 0.47 |
| ADL disability | 0.83 *** | 0.94 | 0.96 | 0.78 * | 0.99 | 0.89 |
| Cognitive impairment | 1.04 + | 1.00 | 1.03 | 1.05 | 1.05 | 1.06 |
| Depression | 1.04 | 0.98 | 1.05 | 1.12 | 0.94 | 0.92 |
|
| ||||||
| N | 1611 | 304 | ||||
| F-value | 7.5 | 1.82 | ||||
p<0.001,
p<0.01,
p<0.05,
p<0.1
Relative risk ratio (RRR), or the probability of being in the “living with others” category over the probability of being in the “living in non-community settings” category, varies between 2.45 for women who stayed in a nursing home less than one month and 3.34 among women who stayed in a nursing home for over three months. Conversely, the probability of living alone following discharge is larger for women who spent shorter time in an LTC facility (RRR=2.37 among those with less than a month long stay) than among those long-term stayers for whom the estimated coefficient is not statistically significant. Finally, women staying for less than three months in an LTC facility have at least one-third lower probability than men to live with a spouse (RRR=0.58 for stays shorter than a month, and RRR=0.67 for less than three-month stays).
Homeownership and higher income are associated with a higher probability of living with a spouse, whereas memory-related diseases and ADL difficulties are associated with a lower probability of living in various community settings compared to a non-community location. The presence of children, however, is predictive of living with others for individuals who are discharged after longer LTC stay (RRR=4.89). The observed racial and ethnic differences in post-discharge living arrangements appear to be consistent with differences in marital patterns for non-Hispanic blacks and a lower use of formal (including long-term) care institutions for Hispanics as established in previous research (Baxter, Bryant, Scarbro, & Shetterly, 2001; Elliott, Krivickas, Brault, & Kreider, 2012; Scharlach, Giunta, Chow, & Lehning, 2008).
In summary, the analysis reveals that women are more likely than men to be discharged from LTC facilities even after controlling for various predisposing, enabling, and need characteristics of nursing home residents. Following discharge, the majority of former nursing home residents return to their community and lives with spouses, children, or other relatives, but a substantial minority live alone, and women, particularly if unmarried, are overrepresented in this group.
This study contributes to the literature on transitional care by exploring both LTC facility discharge and post-discharge living arrangements using a nationally representative sample of older Americans. It extends previous findings based on state-level (Arling et al., 2010), county-level (Thomas et al., 2010), and city-level (Engle & Graney, 1993) analyses, and provides new, nationally representative evidence that women in the United States are more likely than men to be discharged from an LTC facility even after controlling for various predisposing, enabling, and need factors as well as accounting for the competing risk of dying. Following discharge, women are more likely than men to live alone, although the difference disappears among those individuals with the longest duration of stay in an LTC facility. This points to the importance of considering length of stay when investigating who may be particularly vulnerable after discharge from LTC facilities. While further study is needed to fully explain the sources of these systematic gender differences in institutional long-term care, the results presented in this paper suggest that some components of Andersen's behavioral model, including family support networks, function differently according to gender in relation to LTC facility discharge, length of stay, and post-discharge living arrangements.
This study also contributes to a better distinction between short- and long-term institutional residents and their unique transition pathways. Our study mirrors prior research of nursing home use (Thomeer et al., 2014; Wallace et al., 1998) and Andersen's behavioral model (Andersen, 1995), and finds need factors to be major determinants of LTC facility discharge and especially post-discharge living arrangements. However, the findings also suggest that predisposing and enabling factors are relatively more important predictors of LTC facility discharge and post-discharge living arrangements for individuals with a longer duration of institutional stay. It appears, therefore, that transitional care is a complex process, possibly because of the spectrum of options in formal and informal care arrangements following discharge and the multitude of factors affecting the ultimate outcome.
While analysis of the HRS data provides nationally relevant information, it also results in several analytical limitations. Previous research suggests that various types of long-term care (e.g., assisted living facilities, skilled nursing homes) are functionally very different (Zimmerman et al., 2003). However, the HRS employs a broad definition of LTC facilities that precludes us from examining possible differences in discharge patterns by type of LTC facilities. Similarly, due to HRS questionnaire limitations and small sample sizes, the “non-community location” category of post-discharge living arrangements variable subsumes various types of formal-care institutions like retirement centers or nursing homes, limiting us from a more nuanced treatment of post-discharge placement. Examining different types of post-discharge living arrangement in the community would likely reveal important gender differences that would be relevant to post-discharge policies. Finally, our HRS sample may not necessarily be fully representative of the population in LTC facilities since it was not specifically created as an LTC facility survey, but rather as a survey representative of the general U.S. population.
Implications for Policy and/or Practice
As the nation ages and healthcare costs increase, using available resources in the most efficient and effective way becomes imperative. Among the most prominent proposals to stem the rising cost of institutional long-term care is one that would transfer individuals with low care needs to their respective communities, where their families and larger support networks could provide them with a level of care suitable for successful living (Mor et al., 2007). About half of all long-term nursing home residents indicate a preference for transition to the community (Nishita, Wilber, Matsumoto, & Schnelle, 2008), and many more would doubtless benefit in many ways from returning to an informal living environment. Implementing such a strategy is difficult, however, and organizing and financing transitional care is a weakness in the current U.S. health care system. Medicare made overpayments of approximately $5.1 billion in 2009 for inferior care at skilled-nursing facilities due to inadequate discharge planning (Department of Health and Human Services, 2013). Moreover, transition between formal and community care carries a risk of receiving insufficient care (Coleman, 2003). The social and economic dimensions of this issue are complex, and they will become increasingly critical over time.
Despite these challenges, state and federal governments are expanding their efforts to promote deinstitutionalized living arrangements and aging in place, including the transition of nursing home residents back to their respective communities (Gassoumis et al., 2013). Increasingly, states are implementing programs like Home and Community-Based Services despite occasional difficulties regarding program costs, lack of qualified staff and appropriate infrastructure, and resistance from various stakeholders (Doty, Mahoney, & Sciegaj, 2010). Furthermore, states are also implementing Money Follows the Person demonstration programs, first established by Congress in 2005 and designed to facilitate transition of Medicaid beneficiaries with longer (over 90 days) duration of stay in long-term care facilities back to the community. The Patient Protection and Affordable Care Act (ACA) focuses on improving transparency and accountability of LTC facilities as well as protection of care recipients (Hawes, Moudouni, Edwards, & Phillips, 2012), and ACA's Community First Choice Option expands support to beneficiaries to continue living in the community rather than moving to an LTC facility. Transitional care also features prominently in the ACA through the Community-Based Care Transitions Program (Section 3026) and other Medicare and Medicaid initiatives that are aimed at improving care coordination and transitional care as well as decreasing the risk of readmission into formal care (Burton, 2012; Naylor, Aiken, Kurtzman, Olds, & Hirschman, 2011). Women at the tail end of the life course in particular will benefit from these programs because they tend to turn to community-based formal care organizations in the event of poor health and infirmity (Herrera, George, Angel, Markides, & Torres-Gil, 2013).
Given this context, the present study provides nationally relevant information about the characteristics of the older population transitioning out of formal LTC facilities. This information can be used to improve the way policy makers and program planners approach the design and delivery of care services for this population. The findings suggest, for example, that women and men differ in their health profile and related needs, material resources, and in particular access to family support. Older women are more likely than older men to be widowed or divorced, and they seem to rely on a larger social network for informal care support (Brandt, Haberkern, & Szydlik, 2009; Kalmijn, 2007), so the critical aspect for their successful community transition is careful advance planning and coordination between various potential informal caregivers to minimize the disruption of multiple transitions among caregivers.
In contrast, men tend to rely primarily on their spouses for informal care, so they are at higher risk than women of receiving no care (due to loss of a spouse) or insufficient care (due to spouse's illness), which is often related to increased risk of readmission into the formal care system (Woz et al., 2012). Since men's social networks tend to be less developed than those of women, identifying and engaging friends and family members other than spouses who could participate in care provision after LTC facility discharge should be an essential part of discharge planning for older men (Allen et al., 2012).
The role that family members, especially grown children, play in informal caregiving is among the key differences in the long-term care provided to older women and men. As noted earlier, older mothers tend to be closer to their grown children, especially daughters, than older fathers are (Bengtson, 2001; Silverstein & Bengtson, 1997; Suitor & Pillemer, 2006), and they are therefore more likely to depend on their children for support. Therefore, in the absence of a living spouse, women are in a better position than men to transition to home care from a hospital or nursing home.
However, as the population ages and family size decreases for subsequent cohorts of older adults, subsequent populations may be less able to rely on grown children for care. Projections suggest that the ratio of potential caregivers aged 45–64 to persons aged 80 and older will decrease from more than 7:1 in 2010 to 4:1 by 2030, falling even further to 3:1 by 2050 (Redfoot, Feinberg, & Houser, 2013). Consequently, family caregivers and particularly adult children will likely face a larger burden of care for older individuals while simultaneously having to work and/or provide financial and time support to their children or other family members. Since older women on average rely on family for support more than men do, this development could disproportionately affect them. Moreover, it may further exacerbate negative health implications of informal care provision for family caregivers, too (Donelan, Falik, & DesRoches, 2001). Policymakers should anticipate the possibility that the need for a combination of formal and informal care rather than completely and permanently transition from formal to informal care settings among older women will increase. In this context, improving the coordination between all caregivers, both formal and informal, is essential (Miles & Washington, 2011). Further research is needed to explore this issue as well as strategies leading to policy developments designed to improve the viability of implementing cost-effective community-transition programs.
Acknowledgments
Funding: The research was supported by the NIH National Institute of Minority Health and Health Disparities grant (1 R01 MD005894-01). The funding agency had no involvement in study design, in the collection, analysis and interpretation of data, in the writing of the article, and in the decision to submit the article for publication.
Biographies
Stipica Mudrazija is a postdoctoral scholar at the University of Southern California. His research examines population aging, health, social stratification, and comparative social policy, with a particular focus on the nexus of public and private intergenerational support.
Mieke Beth Thomeer is a sociologist who studies family, health, gender, and aging. Her work focuses on how social relationships interact with gender to influence physical and mental health and how changing family structures influence end-of-life outcomes among older adults.
Jacqueline L. Angel is a Professor of Public Affairs and Sociology at The University of Texas at Austin. Her research addresses the relationships linking gender, inequality, and health across the life course, including a special focus on minority aging and Latinos.
Footnotes
In fact, because of the wording of the relevant HRS questions, many authors who use the HRS data on long-term care simply refer in their work to “nursing homes” (e.g., Muramatsu et al., 2007; Thomeer et al., 2014). However, we consider the definition to be somewhat broader and opt for a more inclusive term “long-term care (LTC) facilities,” but with the understanding that they refer to nursing homes and other similar health care facilities excluding hospices for the terminally ill.
Until 2010, the HRS questionnaire included only a general question asking whether a doctor diagnosed a memory-related disease, whereas from the 2010 Wave it specifies that memory-related diseases of interest are Alzheimer's disease and dementia.
In the cases where the cognitive performance tests could not be conducted with respondents, a different set of measures, based on IQCODE scale developed by Jorm and colleagues (Jorm, 1994; Jorm and Jacomb, 1989) was used to ascertain the respondents' cognitive status. HRS provides imputed data on cognitive functioning that account for proxy interviews. More information is available in the Documentation of Cognitive Functioning Measures in the Health and Retirement Study report (Ofstedal, Fisher, & Herzog, 2005).
Detailed information about the health scores used as predictors in this analysis can be found in RAND HRS Data Documentation (Chien et al., 2014).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stipica Mudrazija, Email: mthomeer@uab.edu.
Jacqueline L. Angel, Email: jangel@austin.utexas.edu.
References
- Akamigbo AB, Wolinsky FD. New evidence of racial differences in access and their effects on the use of nursing homes among older adults. Medical Care. 2007;45(7):672–679. doi: 10.1097/MLR.0b013e3180455677. [DOI] [PubMed] [Google Scholar]
- Allen SM, Lima JC, Goldscheider FK, Roy J. Primary caregiver characteristics and transitions in community-based care. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2012;67(3):362–371. doi: 10.1093/geronb/gbs032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Services Research. 1983;18(1):49. [PMC free article] [PubMed] [Google Scholar]
- Arling G, Kane RL, Cooke V, Lewis T. Targeting residents for transitions from nursing home to community. Health Services Research. 2010;45(3):691–711. doi: 10.1111/j.1475-6773.2010.01105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter J, Bryant LL, Scarbro S, Shetterly SM. Patterns of rural Hispanic and non-Hispanic white health care use: The San Luis Valley Health and Aging Study. Research on Aging. 2001;23(1):37–60. [Google Scholar]
- Bengtson VL. Beyond the nuclear family: The increasing importance of multigenerational bonds. Journal of Marriage and Family. 2001;63(1):1–16. [Google Scholar]
- Brandt M, Haberkern K, Szydlik M. Intergenerational help and care in Europe. European Sociological Review. 2009;25(5):585–601. [Google Scholar]
- Burton RA. Health policy brief: improving care transitions. Health Affairs. 2012 Sep 13; 2012. [Google Scholar]
- Case A, Paxson C. Sex differences in morbidity and mortality. Demography. 2005;42(2):189–214. doi: 10.1353/dem.2005.0011. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Long term care hospital prospective payment system: Short-stay outliers. 2012 Retrieved from http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/LTCH-ShortStay.pdf.
- Chapin R, Baca B, Macmillan K, Rachlin R, Zimmerman M. Residential outcomes for nursing facility applicants who have been diverted: Where are they 5 years later? The Gerontologist. 2009;49(1):46–56. doi: 10.1093/geront/gnp009. [DOI] [PubMed] [Google Scholar]
- Chien S, Campbell N, Hayden O, Hurd M, Main R, Mallett J, et al. St Clair P. RAND HRS data documentation, version N. 2014 Retrieved from http://hrsonline.isr.umich.edu/modules/meta/rand/randhrsn/randhrsN.pdf.
- Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. Journal of the American Geriatrics Society. 2003;51(4):549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- Crescioni M, Gorina Y, Bilheimer L, Gillum RF. National Health Statistics Reports, no. 24. Hyattsville, MD: National Center for Health Statistics; 2010. Trends in health status and health care use among older men. [PubMed] [Google Scholar]
- Department of Health and Human Services. Skilled nursing facilities often fail to meet care planning and discharge planning requirements (OEI-02-09-00201) 2013 doi: 10.1016/j.gerinurse.2013.04.005. from https://oig.hhs.gov/oei/reports/oei-02-09-00201.pdf. [DOI] [PubMed]
- Donelan K, Falik M, DesRoches CM. Caregiving: Challenges and implications for women's health. Women's Health Issues. 2001;11(3):185–200. doi: 10.1016/s1049-3867(01)00080-9. [DOI] [PubMed] [Google Scholar]
- Doty P, Mahoney KJ, Sciegaj M. New state strategies to meet long-term care needs. Health Affairs. 2010;29(1):49–56. doi: 10.1377/hlthaff.2009.0521. [DOI] [PubMed] [Google Scholar]
- Elliott DB, Krivickas K, Brault MW, Kreider RM. Historical marriage trends from 1890-2010: A focus on race differences. Washington, DC: United States Census Bureau; 2012. [Google Scholar]
- Engle VF, Graney MJ. Predicting outcomes of nursing home residents: Death and discharge home. Journal of Gerontology. 1993;48(5):S269–S275. doi: 10.1093/geronj/48.5.s269. [DOI] [PubMed] [Google Scholar]
- Feder J, Komisar HL. The importance of federal financing to the nation's long-term care safety net. The SCAN Foundation; 2012. [Google Scholar]
- Freedman VA. Family structure and the risk of nursing home admission. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1996;51(2):S61–S69. doi: 10.1093/geronb/51b.2.s61. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Berkman LF, Rapp SR, Ostfeld AM. Family networks: Predictors of nursing home entry. American Journal of Public Health. 1994;84(5):843–845. doi: 10.2105/ajph.84.5.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Spillman BC, Andreski PM, Cornman JC, Crimmins EM, Kramarow E, et al. Schoeni RF. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50(2):661–671. doi: 10.1007/s13524-012-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritzell J, Lennartsson C. Financial transfers between generations in Sweden. Ageing and Society. 2005;25(3):397–414. [Google Scholar]
- Gassoumis ZD, Fike KT, Rahman AN, Enguidanos SM, Wilber KH. Who transitions to the community from nursing homes? Comparing patterns and predictors for short-stay and long-stay residents. Home Health Care Services Quarterly. 2013;32(2):75–91. doi: 10.1080/01621424.2013.779353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes C, Moudouni DM, Edwards RB, Phillips CD. Nursing homes and the affordable care act: a cease fire in the ongoing struggle over quality reform. Journal of Aging & Social Policy. 2012;24(2):206–220. doi: 10.1080/08959420.2012.660046. [DOI] [PubMed] [Google Scholar]
- Herrera AP, George R, Angel JL, Markides K, Torres-Gil F. Variation in Older Americans Act caregiver service use, unmet hours of care, and independence among Hispanics, African Americans, and Whites. Home Health Care Services Quarterly. 2013;32(1):35–56. doi: 10.1080/01621424.2012.755143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell S, Silberberg M, Quinn WV, Lucas JA. Determinants of remaining in the community after discharge: Results from New Jersey's Nursing Home Transition Program. The Gerontologist. 2007;47(4):535–547. doi: 10.1093/geront/47.4.535. [DOI] [PubMed] [Google Scholar]
- Ingersoll-Dayton B, Starrels ME, Dowler D. Caregiving for parents and parents-in-law: Is gender important? The Gerontologist. 1996;36(4):483–491. doi: 10.1093/geront/36.4.483. [DOI] [PubMed] [Google Scholar]
- James ML, Wiley E, Fries BE. Predicting nursing facility transition candidates using AID: A case study. The Gerontologist. 2007;47(5):625–632. doi: 10.1093/geront/47.5.625. [DOI] [PubMed] [Google Scholar]
- Johnson RW, Toohey D, Wiener JM. Meeting the long-term care needs of the baby boomers. Washington, DC: Urban Institute; 2007. [Google Scholar]
- Jorm AF. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Development and cross-validation. Psychological Medicine. 1994;24(1):145–153. doi: 10.1017/s003329170002691x. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Jacomb PA. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Socio-demographic correlates, reliability, validity and some norms. Psychological Medicine. 1989;19(4):1015–1022. doi: 10.1017/s0033291700005742. [DOI] [PubMed] [Google Scholar]
- Kalmijn M. Gender differences in the effects of divorce, widowhood and remarriage on intergenerational support: Does marriage protect fathers? Social Forces. 2007;85(3):1079–1104. [Google Scholar]
- Lakdawalla D, Goldman DP, Bhattacharya J, Hurd MD, Joyce GF, Panis CW. Forecasting the nursing home population. Medical Care. 2003;41(1):8–20. doi: 10.1097/00005650-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Mehr DR, Williams BC, Fries B. Predicting discharge outcomes of VA nursing home residents. Journal of Aging and Health. 1997;9(2):244–265. doi: 10.1177/089826439700900206. [DOI] [PubMed] [Google Scholar]
- Miles TP, Washington KT. Physical health problems: Shaping transitions of care. Annual Review of Gerontology and Geriatrics. 2011;31(1):65–91. [Google Scholar]
- Mor V, Zinn J, Gozalo P, Feng Z, Intrator O, Grabowski DC. Prospects for transferring nursing home residents to the community. Health Affairs. 2007;26(6):1762–1771. doi: 10.1377/hlthaff.26.6.1762. [DOI] [PubMed] [Google Scholar]
- Muramatsu N, Yin H, Campbell RT, Hoyem RL, Jacob MA, Ross CO. Risk of nursing home admission among older americans: does states' spending on home-and community-based services matter? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62(3):S169–S178. doi: 10.1093/geronb/62.3.s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murtaugh CM. Discharge planning in nursing homes. Health Services Research. 1994;28(6):751. [PMC free article] [PubMed] [Google Scholar]
- Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Affairs. 2011;30(4):746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- Nishita CM, Wilber KH, Matsumoto S, Schnelle JF. Transitioning residents from nursing facilities to community living: Who wants to leave? Journal of the American Geriatrics Society. 2008;56(1):1–7. doi: 10.1111/j.1532-5415.2007.01566.x. [DOI] [PubMed] [Google Scholar]
- Noël-Miller C. Spousal loss, children, and the risk of nursing home admission. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2010;65(3):370–380. doi: 10.1093/geronb/gbq020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ofstedal MB, Fisher GG, Herzog AR. Documentation of Cognitive Functioning Measures in the Health and Retirement Study (HRS Documentation Report DR-006) 2005 Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-006.pdf.
- Penrod JD, Kane RA, Kane RL. Effects of posthospital informal care on nursing home discharge. Research on Aging. 2000;22(1):66–82. [Google Scholar]
- Redfoot D, Feinberg L, Houser A. The aging of the baby boom and the growing care gap: A look at future declines in the availability of family caregivers. AARP Public Policy Institute; 2013. [Google Scholar]
- Reinhard SC. Diversion, transition programs target nursing homes' status quo. Health Affairs. 2010;29(1):44–48. doi: 10.1377/hlthaff.2009.0877. [DOI] [PubMed] [Google Scholar]
- Robison J, Shugrue N, Fortinsky RH, Gruman C. Long-term supports and services planning for the future: Implications from a statewide survey of baby boomers and older adults. The Gerontologist. 2014;54(2):297–313. doi: 10.1093/geront/gnt094. [DOI] [PubMed] [Google Scholar]
- Scharlach AE, Giunta N, Chow JCC, Lehning A. Racial and ethnic variations in caregiver service use. Journal of Aging and Health. 2008;20(3):326–346. doi: 10.1177/0898264308315426. [DOI] [PubMed] [Google Scholar]
- Silverstein M, Bengtson VL. Intergenerational solidarity and the structure of adult child-parent relationships in American families. American Journal of Sociology. 1997;103(2):429–460. [Google Scholar]
- Strunin L, Stone M, Jack B. Understanding rehospitalization risk: Can hospital discharge be modified to reduce recurrent hospitalization? Journal of Hospital Medicine. 2007;2(5):297–304. doi: 10.1002/jhm.206. [DOI] [PubMed] [Google Scholar]
- Suitor JJ, Pillemer K. Choosing daughters: Exploring why mothers favor adult daughters over sons. Sociological Perspectives. 2006;49(2):139–161. [Google Scholar]
- Thomas KE, Gassoumis ZD, Wilber KH. Conversion diversion: Participation in a social HMO reduces the likelihood of converting from short-stay to long-stay nursing facility placement. Journal of the American Medical Directors Association. 2010;11(5):333–337. doi: 10.1016/j.jamda.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer MB, Mudrazija S, Angel JL. How do race and Hispanic ethnicity affect nursing home admission? Evidence from the Health and Retirement Study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;70(4):628–638. doi: 10.1093/geronb/gbu114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. America's families and living arrangements: 2011. 2011 Retrieved from https://www.census.gov/population/www/socdemo/hh-fam/cps2011.html.
- Wallace SP, Levy-Storms L, Kington RS, Andersen RM. The persistence of race and ethnicity in the use of long-term care. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1998;53(2):S104–S112. doi: 10.1093/geronb/53b.2.s104. [DOI] [PubMed] [Google Scholar]
- Wattmo C, Wallin ÅK, Londos E, Minthon L. Risk factors for nursing home placement in Alzheimer's disease: A longitudinal study of cognition, ADL, service utilization, and cholinesterase inhibitor treatment. The Gerontologist. 2011;51(1):17–27. doi: 10.1093/geront/gnq050. [DOI] [PubMed] [Google Scholar]
- Woz S, Mitchell S, Hesko C, Paasche-Orlow M, Greenwald J, Chetty V, et al. Jack B. Gender as risk factor for 30 days post-discharge hospital utilisation: a secondary data analysis. BMJ Open. 2012;2(2) doi: 10.1136/bmjopen-2011-000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y, Land KC, Gu D, Wang Z. Household and living arrangement projections: The extended cohort-component method and applications to the U.S. and China. Springer; Netherlands: 2014. [Google Scholar]
- Zimmerman S, Gruber-Baldini AL, Sloane PD, Eckert JK, Hebel JR, Morgan LA, et al. Chen C. Assisted living and nursing homes: Apples and oranges? The Gerontologist. 2003;43(suppl 2):107–117. doi: 10.1093/geront/43.suppl_2.107. [DOI] [PubMed] [Google Scholar]