ABSTRACT
The aim of this study was to determine the clinical safety and efficacy of preoperative embolization of meningiomas with low-concentration n-butyl cyanoacrylate (NBCA). Nineteen cases of hypervascular intracranial meningiomas were treated by preoperative embolization with 14% NBCA, using a wedged superselective catheterization of feeding arteries and reflux-hold-reinjection technique. Clinical data of the patients and radiological and intra-surgical findings were reviewed. All tumors were successfully devascularized without any neurological complications. Marked reduction of tumor staining with extensive NBCA penetration was achieved in 13 cases. Perioperative blood transfusion was only required in two cases. These results indicate that preoperative embolization of meningiomas with low-concentration NBCA is both safe and effective.
Key Words: embolization, meningiomas, n-butyl cyanoacrylate, preoperative
INTRODUCTION
Preoperative embolization of meningiomas is widely performed to reduce intraoperative blood loss, operative time, and the degree of surgical difficulty.1-3) The procedure most often utilizes polyvinyl alcohol (PVA) particles or Gelfoam powder.1-4) A limited number of recent reports have described the use of liquid adhesive agents such as n-butyl cyanoacrylate (NBCA) (Histoacryl; B. Braun, Melsungen, Germany).2, 5) To the best of our knowledge, using NBCA for preoperative embolization of meningiomas at a concentration of 14% or less has not been previously reported. Therefore, we investigated the safety and efficacy of preoperative embolization of meningiomas with low-concentration NBCA.
MATERIAL AND METHODS
Patients
Between March 2012 and February 2015, we performed preoperative surgical embolization of 19 consecutive cases of hypervascular intracranial meningiomas with low-concentration NBCA. Indications for preoperative embolization depended on the personal preference of the neurosurgeon. Clinical data, radiological, and intra-surgical findings of each case were obtained and retrospectively reviewed from hospital records and operation reports. Four lesions were convex, four parasagittal, four cerebellopontine angle, three falx lesions, and four others. Each tumor was mainly supplied by branches of the external carotid artery.
Embolization Technique
All endovascular embolizations were performed under local anesthesia 1 or 2 days before surgery. Access was achieved by a percutaneous transfemoral technique. Heparinized saline was administered via pressure bags to continuously flush the catheters (3000 U/0.5 l); however, no systemic heparinization was performed. Six French guiding catheters were placed in the proximal external carotid artery. A Marathon microcatheter (1.65 m; Micro Therapeutics, Inc., Irvine, CA, USA) was commonly navigated distally with an ASAHI CHIKAI 10 microguidewire (Asahi Intecc, Aichi, Japan) as far as possible into the target arteries. Occasionally, an Echelon 10 (eV3 Covidien; Irvine, CA, USA) or Headway microcatheter (Terumo, Tokyo, Japan) was used for coil embolization before injecting NBCA. After superselective angiography, a provocative test with 1% lidocaine was performed in cases where dangerous anastomoses were suspected. Fourteen percent NBCA was prepared with pure NBCA and lipiodol (Lipiodol Ultra-Fluide®, Guerbet, Roissy, France) in a 1:6 ratio. The liquid agent was drawn into a 1-ml Medallion® syringe (Merit Medical, UT, USA) and warmed with steam for approximately 10 sec to reduce viscosity. Using a digital subtraction angiography for guidance, 14% NBCA was injected using the reflux-hold-reinjection technique. The syringe was handled by the operator in a similar fashion as coil delivery to achieve fine control (Fig. 1). The microcatheter was slowly withdrawn once the reflux had covered its tip.
Fig. 1.
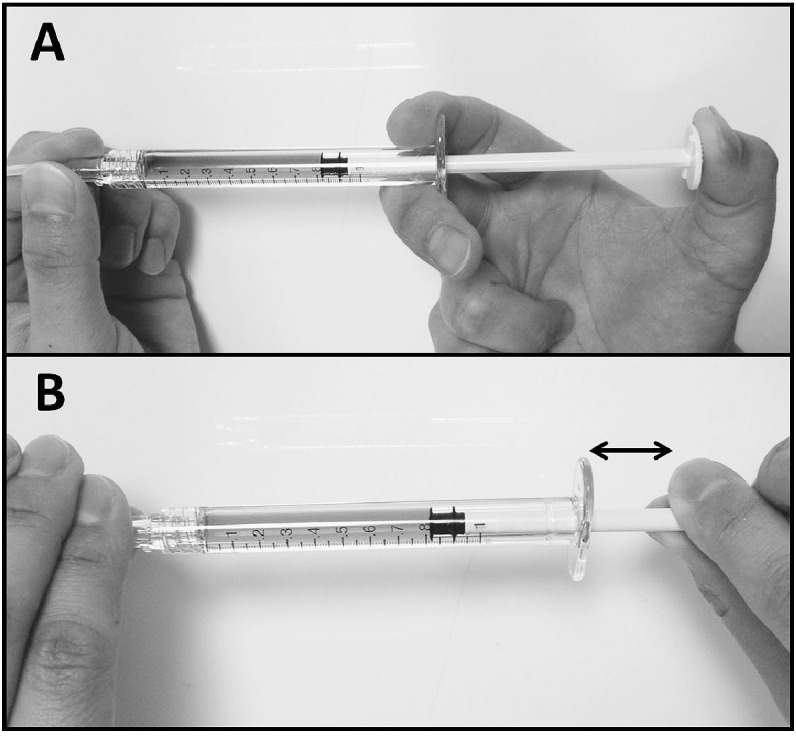
Photographs of injection handling showing A: conventional style, B: a novel technique similar to coil insertion; ↔ indicates that shorter strokes are better.
Data Evaluation
Effectiveness of preoperative embolization was retrospectively evaluated by each neurosurgeon based on the intraoperative blood loss and solidity of the tumor as excellent, good, and poor.
RESULTS
Embolization Outcome
Among 19 patients treated, a total of 31 arteries were embolized with 14% NBCA. Details of the patient characteristics and embolization procedure are summarized in Table 1. Almost all cases achieved marked reduction of tumor staining with extensive NBCA penetration. The average length of the endovascular procedure was 80 min (50–190 min). Five cases were embolized using detachable coils to enable flow control and avoid NBCA migration to important vessels. A representative case, Case 3, is shown in Fig. 2-4.
Table 1.
Characteristics of patients and summary of preoperative TAE
| Case | Age/Sex | Location of tumor |
Size of tumor (cm) |
Target feeding artery |
Microcatheter | Amount of 14% NBCA (ml) |
Complication of TAE | Interval to surgery (days) |
Effectiveness of TAE |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 80/F | Lt convexity | 5.5×3.3×3.5 | MMA, STA | Echlon 10 | 0.4 | None | 1 | Excellent |
| 2 | 79/M | Rt parasagittal | 5.3×4.1×4.6 | MMA | Marathon | 0.55 | None | 1 | Excellent |
| 3 | 52/F | Lt falx | 3.4×3.4×3.6 | MMA | Marathon | 0.6 | None | 2 | Excellent |
| 4 | 71/F | Lt parasagittal | 3.6×3.4×2.6 | MMA | Marathon | 0.5 | None | 2 | Excellent |
| 5 | 78/M | Rt parasagittal | 2.1×1.9×1.7 | MMA | Marathon | 0.3 | None | 2 | Excellent |
| 6 | 49/F | Lt falx | 2.8×2.8×3.4 | MMA | Marathon | 0.25 | None | 2 | Excellent |
| 7 | 65/F | Lt CPA | 2.9×2.8×2.6 | MMA | Echlon 10 | 0.4 | None | 1 | Good |
| 8 | 56/F | Lt olfactory | 5.2×5.5×4.8 | MMA, STA | Marathon | 1.1 | None | 2 | Good |
| 9 | 66/F | Lt parasellar | 2.5×2.1×2.2 | MMA, AMA | Marathon | 0.4 | None | 2 | Poor |
| 10 | 73/F | Lt convexity | 4.3×3.6×2.9 | MMA | Marathon | 0.35 | None | 2 | Excellent |
| 11 | 51/M | Falx | 2.1×3.0×1.9 | MMA | Marathon | 0.3 | None | 1 | Excellent |
| 12 | 46/M | Rt CPA | 3.3×1.9×3.4 | APA | Headway | 0.4 | None | 1 | Good |
| 13 | 40/F | Lt CPA | 4.9×4.6×4.9 | OA | Marathon | 0.5 | None | 2 | Excellent |
| 14 | 63/M | Lt convexity | 1.8×2.3×1.4 | MMA | Marathon | 0.4 | None | 2 | Excellent |
| 15 | 45/F | Rt CPA | 3.9×3.9×3.7 | OA, PA, MMA | Marathon | 0.6 | None | 1 | Excellent |
| 16 | 50/M | Rt sphenoid | 4.0×3.6×3.8 | MMA | Headway | 0.5 | None | 2 | Excellent |
| 17 | 66/F | Rt petroclival | 3.9×3.2×2.9 | MMA | Headway | 0.35 | None | 2 | Poor |
| 18 | 59/F | Rt parasagittal | 3.5×3.4×3.4 | MMA, STA | Marathon | 0.4 | None | 1 | Good |
| 19 | 69/F | Rt convexity | 3.2×4.0×4.0 | MMA | Marathon | 0.15 | None | 1 | Excellent |
APA: ascending pharyngeal artery, CPA: cerebellopontine angle, 4.9F: female, Lt: left, M: male, MMA: middle meningeal artery, NBCA: n-butyl cyanoacrylate, OA: occipital artery,
PA: posteror auricular artery, Rt: right, STA: superficial temporal artery, TAE: trans-arterial embolization
Fig. 2.
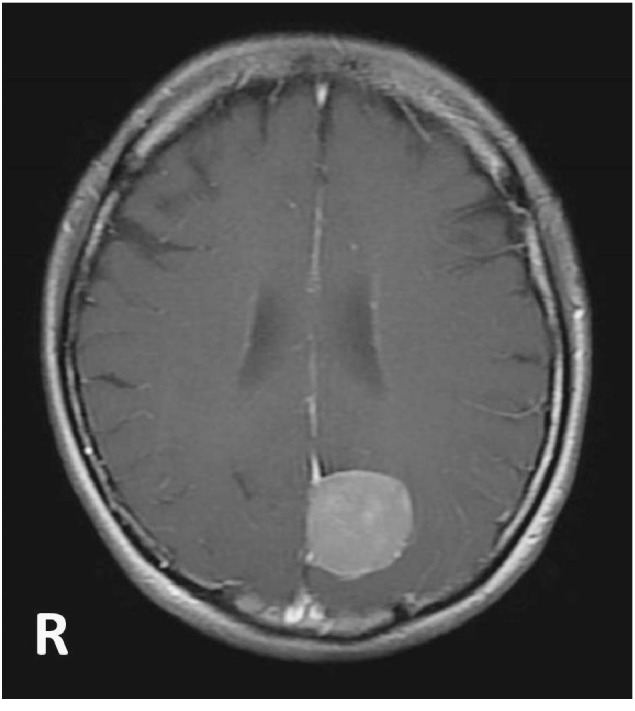
Initial gadolinium-enhanced axial magnetic resonance image of Case 3, showing a homogeneously enhanced tumor.
Fig. 4.
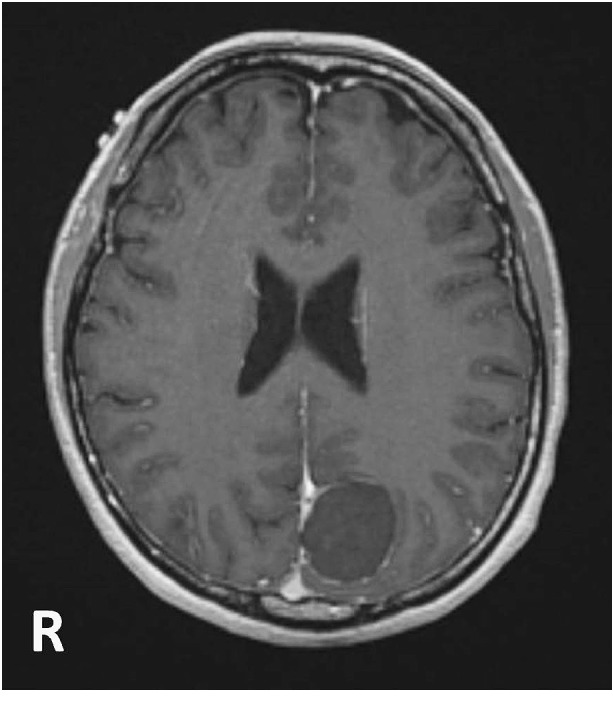
Gadolinium-enhanced axial magnetic resonance image 1 day after embolization shows no enhancement in the tumor.
Once the microcatheter was properly wedged, injection of 14% NBCA took approximately 3 min per vessel for deep penetration into the tumor vascular bed. NBCA cast was slowly and consecutively plugged in a retrograde fashion into the other feeding vessels. Fourteen of 19 cases could be embolized with an appropriately wedged catheterization. However, if wedging could not be achieved, embolization tended to cause occlusion of the proximal feeding artery.
Fig. 3.
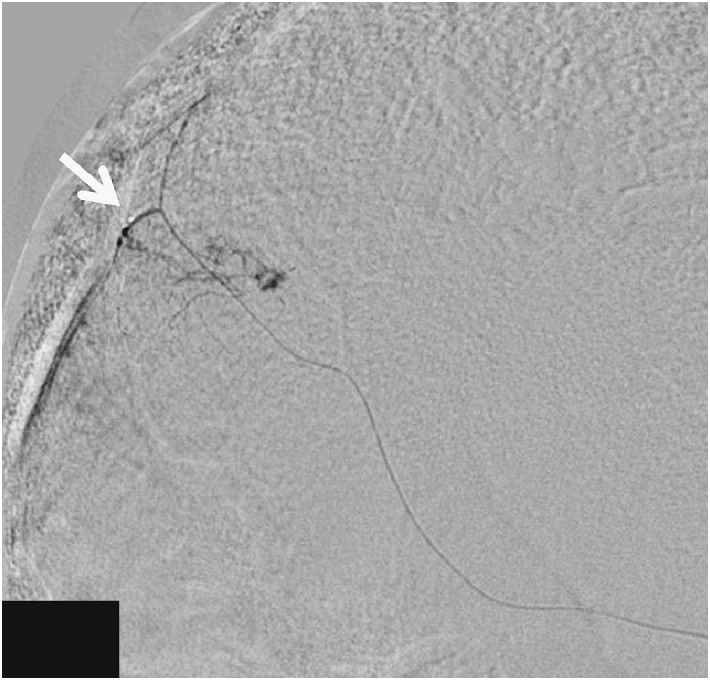
Superselective right middle meningeal artery angiogram, during 14% n-butyl cyanoacrylate injection, showing the cast plugged in a consecutive and retrograde manner into the feeders (white arrow indicate the tip of the Marathon microcatheter).
Complications
There were no procedure-related complications in any of the 19 cases. Withdrawal of all microcatheters was easy, if done in a slow and controlled manner, and there was no adhesion to vessels during the process. However, some patients complained of a temporary headache immediately after NBCA was injected.
Surgical Treatment
Surgical resection was performed in all cases, 1 or 2 days after embolization. Twelve patients underwent gross total resection, and seven underwent subtotal resection. Only two patients required perioperative blood transfusion, a parasellar case (Case 9) and petroclival case (Case 17).
DISCUSSION
Preoperative embolization of hypervascular intracranial tumors is widely used to facilitate surgical resection and reduce intraoperative blood loss.1-3) Particle embolic materials, such as PVA, have been used for many years;1-4) however, particle embolization has some clinical limitations. First, while larger particles carry a lower risk of inattentive embolization, they cannot deeply occlude the tumor tissue. In contrast, smaller particles provide better penetration but carry a higher risk of inadvertent embolization and migration into the pulmonary tissue. Furthermore, poor visualization of suspended particles promotes leakage into normal tissues. Finally, particle embolization is not permanent. Even if complete occlusion is achieved, recanalization is possible during tumor resection.
Conversely, liquid adhesive agents, such as NBCA, provide highly penetrative and permanent embolization and thus, avoid some of the pitfalls of particle embolization. Low-concentration NBCA is well visualized under fluoroscopy as a unique glue cast. Furthermore, Kim et al.5) reported low morbidity with the use of 29% NBCA for preoperative embolization of brain tumors, and Kominami et al.6) reported presurgical embolization with 17%–25% NBCA for meningiomas, as being safe and effective. Recently, two studies have reported the effectiveness of low-concentration NBCA embolization in cases of dural arteriovenous fistulas.7-8) Li et al.7) used 10%–17% NBCA by wedging the microcatheter into the main feeding artery. However, to the best of our knowledge, using NBCA at a concentration of 14% or less to treat intracranial tumors has not been described.
In this report, we used low-concentration NBCA for tumor embolization. NBCA at low concentration as compared with that at high concentration penetrates more deeply into the tumor and carries a lower risk of catheter adhesion. Because adhesion of NBCA cast depends on the balance of its concentration and blood flow velocity, it is important to control the local blood flow. Because the wedged microcatheter provides a stable local flow control, it must be advanced as distally far as possible. The reflux-hold-reinjection technique is also available for ideal NBCA penetration under a true local flow-arrest state. This technique is commonly used in the treatment of cerebral arteriovenous malformations with Onyx (Micro Therapeutics, Inc., Irvin, CA, USA). Although Shi et al.9) have reported the effectiveness of preoperative embolization of meningiomas with Onyx, it is not available for tumor embolization in Japan. Conversely, our technique of handling the 1 ml syringe in a similar fashion as coil delivery has been strongly recommended (Fig. 1). We believe that this enables finer control of the amount of NBCA injected, particularly in surgeons not familiar with the technique, compared with conventional injection by pushing the syringe with the right thumb. Shorter strokes of the right index finger and thumb are preferred to avoid over-injection of NBCA.
As a suitable substitute, we recommend the use of the 1.65-m Marathon microcatheter to allow wedging into the farthest distal feeding arteries. A standard 1.5-m microcatheter is occasionally too short to wedge into the target vessels. When the microcatheter cannot be suitably wedged, NBCA venous migration in high-flow conditions and proximal feeder occlusion in low-flow conditions can occur. In such cases, we replaced the microcatheter with a thicker one or added detachable coils prior to NBCA injection for better flow control. ED Coil Extrasoft (Kaneka, Kanagawa, Japan) can be used with the Marathon microcatheter, regardless of a one-marker and 1.65-m long catheter. The importance of wedged catheterization for this procedure cannot be emphasized enough.
During tumor removal in our 13 of the 19 cases, there was almost no intratumor bleeding. Only one parasellar case and one petroclival case (Cases 9 and 17) required perioperative blood transfusion. These tumors were well-supplied from the internal carotid artery–tentorial artery. Surgeons reported that it was easier to suction the tumor after low-concentration NBCA embolization compared with conventional particle embolization because tumor consistency changed to very soft and cream-like, rather than sponge-like.
Finally, low-concentration NBCA embolization facilitated improved surgical performance and did not cause any serious clinical complications.
CONCLUSIONS
In 19 cases, we reported high safety and efficacy of preoperative embolization of meningiomas with low-concentration NBCA. However, several important technicalities should be kept in mind during the procedure; namely, the microcatheter must be advanced as distally far as possible and a true flow-arrest condition must be established.
ACKNOWLEDGEMENTS
The authors declare that there is no conflict of interest.
REFERENCES
- 1).Dean BL, Flom RA, Wallace RC, Khayata MH, Obuchowski NA, Hodak JA, Zabramski JM, Spetzler RF. Efficacy of endovascular treatment of meningiomas: evaluation with matched samples. AJNR Am J Neuroradiol, 1994; 15: 1675–1680. [PMC free article] [PubMed]
- 2).Gruber A, Bavinzski G, Killer M, Richling B. Preoperative embolization of hypervascular skull base tumors. Minim Invasive Neurosurg, 2000; 43: 62–71. [DOI] [PubMed]
- 3).Hekster REM, Matricali B, Luyendijk W. Presurgical transfemoral catheter embolization to reduce operative blood loss. Technical note. J Neurosurg, 1974; 41: 396–398. [DOI] [PubMed]
- 4).Carli DF, Sluzewski M, Beute GN, van Rooij WJ. Complications of particle embolization of meningiomas: frequency, risk factors, and outcome. AJNR Am J Neuroradiol, 2010; 31: 152–154. [DOI] [PMC free article] [PubMed]
- 5).Kim LJ, Albuquerque FC, Aziz-Sultan A, Spetzler RF, McDougall CG. Low morbidity associated with the use of NBCA liquid adhesive for preoperative transarterial embolization of central nervous system tumors. Neurosurgery, 2006; 59: 98–104. [DOI] [PubMed]
- 6).Kominami S, Watanabe A, Suzuki M, Mizunari T, Kobayashi S, Teramoto A. Preoperative embolization of meningiomas with n-butyl cyanoacrylate. Interv Neuroradiol, 2012; 18: 133–139. [DOI] [PMC free article] [PubMed]
- 7).Li MH, Tan HQ, Fang C, Zhu YQ, Wang W, Wang J, Cheng YS. Trans-arterial embolization therapy of dural carotid-cavernous fistulae using low concentration n-butyl-cyanoacrylate. Acta Neurochir (Wien), 2008; 150: 1149–1156. [DOI] [PubMed]
- 8).Liu HM, Huang YC, Wang YH, Tu YK. Transarterial embolization of complex cavernous sinus dural arteriovenous fistulae with low-concentration cyanoacrylate. Neuroradiology, 2000; 42: 766–770. [DOI] [PubMed]
- 9).Shi ZS, Feng L, Jiang XB, Huang Q, Yang Z, Huang ZS. Therapeutic embolization of meningiomas with Onyx for delayed surgical resection. Surgical Neurol, 2008; 70: 478–481. [DOI] [PubMed]


