Dear Editor,
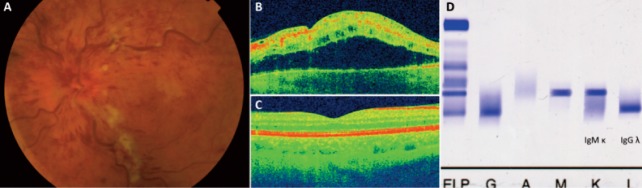
A 70-year-old male presented two weeks following sudden painless loss of left eye vision. His medical history included monoclonal gammopathy of undetermined significance (MGUS) under surveillance, and hypertension on amlodipine. At presentation, visual acuities were 0.16 in the right eye improving with pinhole to 0.33, and perception of hand movements in the left eye (no change with pinhole). Blood pressure was 140/89 mm Hg. Anterior segment examination was unremarkable with normal intraocular pressures of 18 mm Hg in both eyes. Left fundus examination revealed left optic disc swelling, engorged tortuous retinal veins, blot and flame-shaped retinal hemorrhages, and scattered cotton wool spots (Figure 1A) consistent with a diagnosis of ischemic central retinal vein occlusion (CRVO), which could explain the markedly reduced visual acuity and the additional presence of a left afferent pupillary defect (RAPD). Interestingly, low visual acuity and a RAPD are superior to fundus fluorescein angiography in reliably differentiating ischemic from non-ischemic CRVO during the acute phase1. Optical coherence tomography (OCT) verified the presence of cystoid macular edema in the left eye (Figure 1B), and was normal in the right eye (Figure 1C). Laboratory investigations verified the presence of two paraproteins previously identified by immunofixation as IgM kappa and IgG lambda (Figure 1D). Hyperviscosity associated with abnormal serum monoclonal immunoglobulins is an important risk factor for CRVO2 and may lower the blood pressure threshold above which unwanted cardiovascular complications may occur. Patient was treated with intravitreal ranibizumab (anti-Vascular Endothelial Growth Factor antibody) injection3 without significant response. Although management of patients with MGUS does not involve active treatment but mainly watchful waiting, it is essential to optimize hypertension and additional cardiovascular risk factors4 in order to prevent adverse vascular events which can lead to significant compromise of patient’s daily activities.
Figure 1. (A) Left fundus photo showing optic disc swelling, engorged retinal veins, retinal hemorrhages and cotton wool spots. (B) Optical coherence tomography (OCT) scan of left macula showing cystoid macu- lar edema. (C) Normal OCT scan of right macula. (D) Immunofixation gel of patient�s serum demonstrating the presence of abnor- mal monoclonal IgM kappa and IgG lambda paraprotein bands.
Conflict of interest
The authors have no conflicts of interest.
References
- 1.Hayreh SS, Klugman MR, Beri M, Kimura AE, Podhajsky P. Differentiation of ischemic from non-ischemic central retinal vein occlusion during the early acute phase. GraefesArch ClinExpOphthalmol. 1990;228:201–217. doi: 10.1007/BF00920022. [DOI] [PubMed] [Google Scholar]
- 2.Hayasaka S, Ugomori S, Kodama T, Noda S, Setogawa T. Central retinal vein occlusion in two patients with immunoglobulin G multiple myeloma associated with blood hyperviscosity. Ann Ophthalmol. 1993;25:191–194. [PubMed] [Google Scholar]
- 3.Haller JA. Current anti-vascular endothelial growth factor dosing regimens: benefits and burden. Ophthalmology. 2013;120:S3–S7. doi: 10.1016/j.ophtha.2013.01.057. [DOI] [PubMed] [Google Scholar]
- 4.Querques G, Triolo G, Casalino G, Garca-Arum J, Badal J, Zapata M, et al. Retinal vein occlusions: Diagnosis and choice of treatments. Ophthalmic Res. 2013;49:215–222. doi: 10.1159/000346734. [DOI] [PubMed] [Google Scholar]


