Abstract
We report a case of “can ventilate but can’t intubate” situation which was successfully managed in the Emergency Department and Intensive Care Unit by the use of ProSeal laryngeal mask airway and Frova Intubating Introducer as bridging rescue devices. Use of appropriate technique while strictly following the difficult airway algorithm is the mainstay of airway management in unanticipated difficult airway situations. Although the multiple airway devices were used but each step took not more than 2 min and “don’t struggle, skip to the next step principle” was followed. With the availability of many advanced airway management tools, the intensivists should have a training and experience along with preparedness in order to perform such lifesaving airway managements.
Keywords: C-MAC video laryngoscope, difficult airway, Emergency Department, Frova Intubating Introducer, ProSeal laryngeal mask airway
Introduction
The prime target of airway management in Emergency Department (ED) and Intensive Care Unit (ICU) should be optimal ventilation and oxygenation followed by securing a definitive airway while maintaining hemodynamic stability. At times, in spite of the availability of expertise and sophisticated equipment intubation may become a challenge to the intensivist due to many other contributory factors.[1] Here we report the step wise use of ProSeal laryngeal mask airway (PLMA), C-MAC, and Cook Frova Intubating Introducer (FII) in managing a case of unanticipated difficult airway in ED and ICU sequentially under strict adherence to difficult airway algorithm.
Case Report
A 69-year-old patient was brought by a neighbor to the ED of our institute after found unconscious in the cowshed. In the ED, the patient was having Glasgow coma scale of E1V1M4 and was rapidly desaturating on facemask with tachypnea and tachycardia with blood pressure (BP) of 130/70 mm of Hg. Modified rapid sequence intubation was planned and after two failed laryngoscopy attempts, PLMA was inserted through which the ventilation and oxygenation improved. Following gastric decompression patient was shifted to ICU for the definitive airway management. After an uneventful shifting to the ICU, a Cook FII was inserted blindly through the PLMA. The first attempt failed, and the catheter went into the esophagus. While fiberoptic cart being readied, an attempt at video laryngoscopy by using C-MAC (Karl Storz, Tuttlingen, Germany) was carried out. However we were unable to differentiate the structures in and around epiglottis, so an attempt at insertion under C-MAC visualization was made. The following resistance in the first attempt, catheter went inside trachea successfully, which was confirmed by capnography as well as clinically. Oxygenation was adequate with stable hemodynamics. Finally, under C-MAC visualization, a 7.5 mm endotracheal tube (ETT) was railroaded and definitive airway was successfully established.
Discussion
For each arm of the algorithm [Figure 1], the physician followed a step-by-step approach to secure the airway and maintain the oxygenation while following the principle “Do not struggle against the patient, just skip to next step with advanced technique.” Unfortunately, we could not avail the advanced techniques in the ED for which we had to proceed with initial airway management with a PLMA followed by the definite airway management with the surgical airway back up in the critical care unit.
Figure 1.
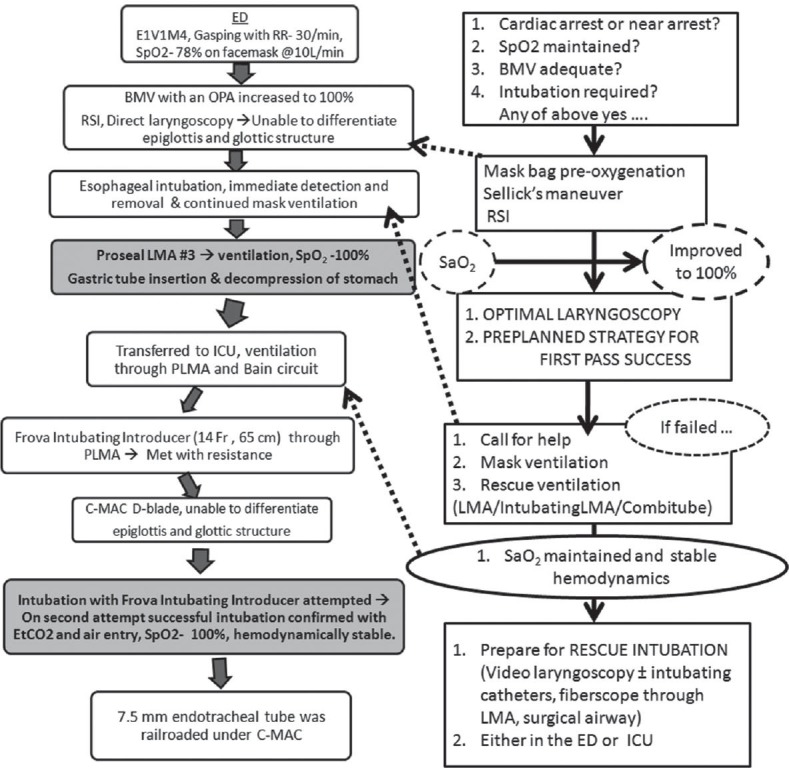
The step wise management of the case in parallel with difficult airway algorithm
Our observation confirms the view that the failure of conventional airway management mandates the accessory rescue airway devices rapidly being deployed in a predefined algorithmic fashion assisting the clinician in airway management. In the present paper, four airway devices were used: The Macintosh laryngoscope, the PLMA, FII, and C-MAC video laryngoscope (VLS) with a D blade with the flexible fiberscope and Melker Emergency Cricothyrotomy Catheter Sets (Cuffed) as back up. Although several airway devices were used, overall airway management duration was relatively short, because for each scenario, failed primary and secondary backup devices were quickly abandoned after two failed attempts, with <2 min duration limit for each attempt, to rapidly use the next rescue device. Because of intrinsic failure rate several airway devices were being used instead of limiting to single device.
VLS allow better imaging of larynx when conventional laryngoscopes fail. The C-MAC® VLS features standard Macintosh blade designs with an external light source and a small digital camera at the distal third of the blade that extend to a video display monitor.[2] With VLS having acute angulated blades such as D-blade of C-MAC, it is possible to have an indirect view of the glottis in the monitor with the help of a miniature camera at the tip of the blades. Studies have shown that the limited laryngeal view improved with the use of C-MAC following direct laryngoscopy.[2,3]
Though successful applications of a C-MAC in expected difficult laryngoscopy settings have been reported but there is insufficient knowledge on the efficacy and potential complications of C-MAC use in emergencies such as unpredicted failed intubation. This case is an example of the use of C-MAC as a tertiary emergency airway device in the event of an unexpected “failed intubation.” A prospective study conducted in the ED showed a higher success rate in second-attempt-intubation using C-MAC compared to second direct laryngoscopy (82.3% vs. 61.7%). This suggests C-MAC use as a rescue device after initial failed intubation attempt in ED.[4]
Use of a flexible stylet improves the negotiation of the ETT and appears to decrease the time to intubation and increases the success rate.[5,6] The clinical cases previously reported prove that GlideScope combined with FII allowed successful intubation of the patients with potential or unexpected difficult airway.[7] The FII is a gum elastic bougie which in combination with C-MAC VLS overcomes some of the limitations of VLS while offering multiple advantages; its 30° anteriorly angulated atraumatic distal tip enhances the endotracheal insertion of the device.[8] Moreover, RapiFit adaptor provided with FII allows oxygenation. Finally, the FII may overcome a common limitation of the available VLS, viz., the limited room available for the manipulation and insertion of the ETT.[9] Additional considerations are derived from the analysis of the hemodynamic parameters: Our pharmacological management could adequately control the values of BP and heart rate after the repeated intubation attempts; the rate-pressure product, indeed, never exceeded the 22,000 threshold value (for myocardial ischemia).[10]
Conclusion
FII along with C-MAC VLS helped us successfully to manage an unpredicted difficult intubation. Specific knowledge of each device, expertise in their use and adherence to difficult airway algorithm are very essential for the successful procedure. Our observations reinforce the need for predefined difficult airway algorithms and physician training with advanced airway devices for the safe management of unanticipated difficult airway cases in ED and ICUs. Struggling with the patient's airway is known to lead to a poor outcome.
Difficult airway management simulations inculcating following requirements should be a part of training programs.
Precise, strict, and acceptable definition of device related failure,
Proposing an acceptable 2-min duration limit of each airway device attempt,
Setting lower limits for a relevant physiological parameter such as SpO2 (e.g., <85%) for the activation of a rescue infraglottic (surgical) oxygenation procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Walz JM, Kaur S, Heard SO. Airway management and endotracheal intubation. In: Irwin RS, Rippe JM, editors. Intensive Care Medicine. 7th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2012. p. 1. [Google Scholar]
- 2.Cavus E, Kieckhaefer J, Doerges V, Moeller T, Thee C, Wagner K. The C-MAC videolaryngoscope: First experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110:473–7. doi: 10.1213/ANE.0b013e3181c5bce5. [DOI] [PubMed] [Google Scholar]
- 3.Piepho T, Fortmueller K, Heid FM, Schmidtmann I, Werner C, Noppens RR. Performance of the C-MAC video laryngoscope in patients after a limited glottic view using Macintosh laryngoscopy. Anaesthesia. 2011;66:1101–5. doi: 10.1111/j.1365-2044.2011.06872.x. [DOI] [PubMed] [Google Scholar]
- 4.Sakles JC, Mosier JM, Patanwala AE, Dicken JM, Kalin L, Javedani PP. The C-MAC ® video laryngoscope is superior to the direct laryngoscope for the rescue of failed first-attempt intubations in the emergency department. J Emerg Med. 2015;48:280–6. doi: 10.1016/j.jemermed.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Rai MR, Dering A, Verghese C. The GlideScope system: A clinical assessment of performance. Anaesthesia. 2005;60:60–4. doi: 10.1111/j.1365-2044.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- 6.Falcó-Molmeneu E, Ramírez-Montero F, Carreguí-Tusón R, Santamaría-Arribas N, Gallén-Jaime T, Vila-Sánchez M. The modified Eschmann guide to facilitate tracheal intubation using the GlideScope. Can J Anaesth. 2006;53:633–4. doi: 10.1007/BF03021859. [DOI] [PubMed] [Google Scholar]
- 7.Heitz JW, Mastrando D. The use of a gum elastic bougie in combination with a videolaryngoscope. J Clin Anesth. 2005;17:408–9. doi: 10.1016/j.jclinane.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Sharma R. A new maneuver for endotracheal tube insertion during difficult GlideScope® intubation: A suggestion. J Emerg Med. 2011;40:443. doi: 10.1016/j.jemermed.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Xue FS, Cheng Y, Li RP, Liao X. Comparative performance of direct and indirect laryngoscopes for emergency intubation under cervical stabilization. Resuscitation. 2012;83:e169. doi: 10.1016/j.resuscitation.2012.02.034. [DOI] [PubMed] [Google Scholar]
- 10.Robinson BF. Relation of heart rate and systolic blood pressure to the onset of pain in angina pectoris. Circulation. 1967;35:1073–83. doi: 10.1161/01.cir.35.6.1073. [DOI] [PubMed] [Google Scholar]


