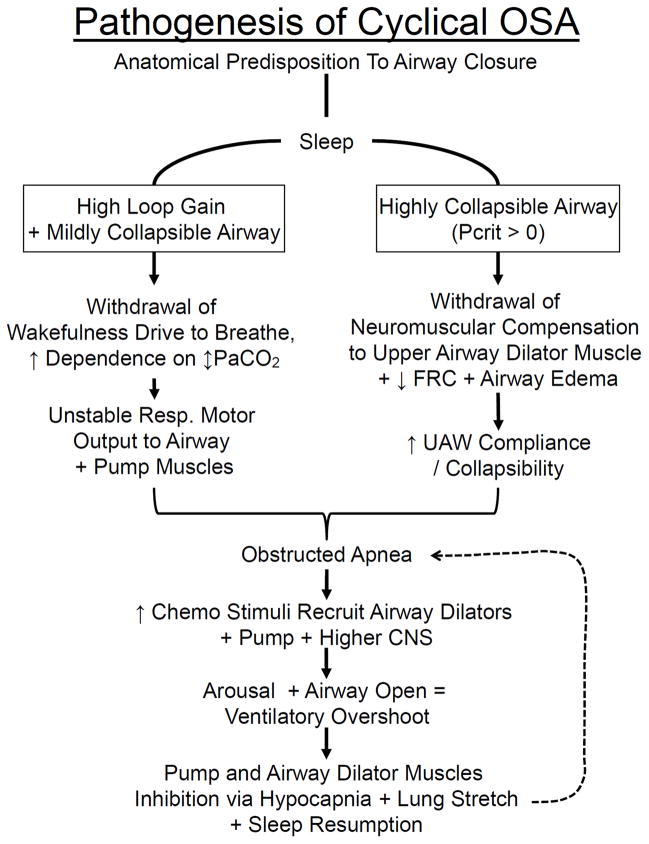
Figure 6.
A. Schematic illustrating the interactive effects of airway anatomy with neurochemical control on the magnitude and stability of central respiratory motor output, airway muscle dilator recruitment, and arousability in the pathogenesis of cyclical OSA. Patients with an anatomical predisposition to pharyngeal collapse may experience two types of overlapping scenarios leading to cyclical OSA in sleep. Right: progression initiated by an airway obstruction at sleep onset in a patient with a severely collapsible upper airway; left: progression to airway obstruction (at the nadir of the respiratory cycle) initiated by an unstable central respiratory motor output in a patient with elevated loop gain and a mildly collapsible airway. Bottom: factors that determine the consequences of airway obstruction and accumulating chemoreceptor stimuli on subsequent, postapneic ventilation, airway patency and EEG arousal. These control system characteristics include the responsiveness of both the upper airway and chest wall pump muscles and of central nervous system (CNS) arousability to the rising chemoreceptor stimuli (also see text and Fig. 5:A). UAW, upper airway; FRC, functional residual capacity. Used with permission from Dempsey et al. [29].
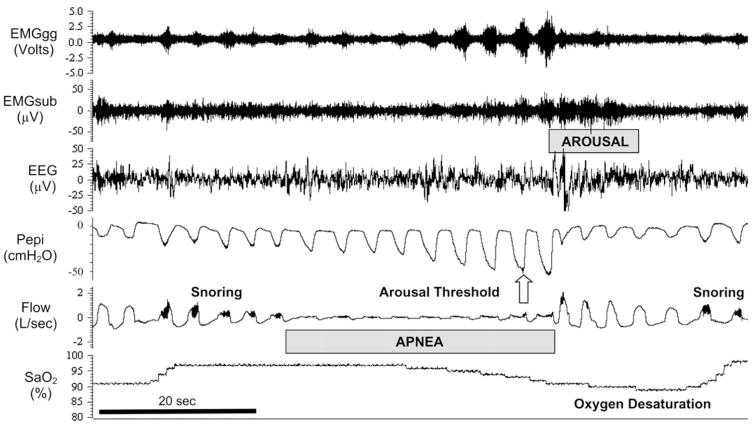
Figure 6. B. Polysomnographic tracing of an obstructed apneic event (between the dotted vertical lines in A) to illustrate the compensatory events occurring during and following the obstruction (apnea/hypopnea index = 56/hour). The cessation and resumption of flow defines the apneic event. Note the progressive increase in inspiratory effort (Pepi) and dilator muscle EMG (EMGgg) during the apnea, the transient arousal coincident with airway opening, and ventilatory overshoot at apnea termination. As the patient returns to sleep, note the gradual reduction in breathing frequency and flow rate, and increased pharyngeal pressure (signifying increased airway resistance) leading to the next obstruction. Evidence of snoring is shown on the flow tracing. Progressive increases in EMGgg activity occurred throughout the obstructive event, although in this instance they were not sufficient to restore flow, which occurred only upon arousal. Pharyngeal pressure serves as a measure of the inspiratory effort made against the obstructed airway, thereby reflecting the magnitude of central respiratory motor output in response to chemoreceptor stimuli accumulated during the obstructed apnea. Arousal threshold is determined by the pharyngeal pressure achieved through respiratory pump muscle contractions during an airway obstruction at the point of EEG arousal. EMGgg, electromyogram of the genioglossus muscle (intramuscular); EMGsub, EMG of the submental muscle (surface); EEG, electroencephalogram (C3-A2); Pepi, pressure at the level of the epiglottis; Flow, airflow measured via nasal mask and pneumotachograph; SaO2, arterial blood oxygen saturation measured via pulse oximetry at the finger. Reprinted with permission of the American Thoracic Society. Copyright © 2013 American Thoracic Society. Eckert DJ and Malhotra A. 2008. Pathophysiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5: 144–153.