Abstract
Waveform capnography was recommended as the most reliable method to confirm correct endotracheal tube or laryngeal mask airway placements. However, capnography may be unreliable during cardiopulmonary resuscitation and during low flow states. It may lead to an unnecessary removal of a well-placed endotracheal tube, re-intubation and interruption of chest compressions. Real-time upper airway (laryngo-tracheal) ultrasonography to confirm correct endotracheal tube placement was shown to be very useful in cadaveric models and during emergency intubation. Tracheal ultrasonography does not interrupt chest compressions and is not affected by low pulmonary flow or airway obstruction, but is limited by ultrasonography scattering and acoustic artifacts generated in air – mucosa interfaces. Sonographic upper airway assessment emerges as a rapid and easily available method to predict difficult intubation, to assess the laryngeal and hypopharyngeal size and visualize the position of the laryngeal mask airway in situ. This study demonstrates that the replacement of air with saline in endotracheal tube or laryngeal mask airway cuffs and the use of the contrast agents enables detection of cuffs in the airway. It also allows visualization of the surrounding structures or tissues as the ultrasound beam can be transmitted through the fluid – filled cuffs without being reflected from air – mucosal interfaces.
Keywords: endotracheal intubation, laryngeal mask airway, upper airway sonography
Abstract
Kapnografia jest uznawana za najbardziej wiarygodną metodę potwierdzenia prawidłowego umiejscowienia rurki intubacyjnej lub maski krtaniowej. W trakcie resuscytacji krążeniowo-oddechowej oraz w stanach niskiego przepływu nie zawsze jednak daje ona wiarygodne wyniki, co może spowodować niepotrzebne usunięcie prawidłowo założonej rurki intubacyjnej, powtórną intubację oraz zakłócenie masażu serca. Przeprowadzane w czasie rzeczywistym badanie ultrasonograficzne górnych dróg oddechowych (krtani i tchawicy), wykonywane w celu potwierdzenia prawidłowego umiejscowienia rurki intubacyjnej, okazało się niezwykle skuteczne w badaniach przeprowadzanych na zwłokach, a także w przypadkach intubacji w stanach nagłych. Ultrasonografia tchawicy nie zakłóca masażu serca i nie zależy od przepływu płucnego i niedrożności dróg oddechowych. Ograniczeniem dla tego badania jest rozproszenie ultradźwięków i generacja artefaktów akustycznych na granicy powietrze – błona śluzowa. Ultrasonografia górnych dróg oddechowych jest szybką, łatwo dostępną i nieinwazyjną metodą umożliwiającą ocenę ich rozmiarów i funkcji, a także wizualizację umiejscowienia maski krtaniowej. Niniejsza praca wykazuje, iż zastąpienie powietrza solą fizjologiczną w przypadku wypełnienia mankietów rurki intubacyjnej i maski krtaniowej oraz zastosowanie środków kontrastowych uwidacznia mankiety w górnych drogach oddechowych. Pozwala również zobaczyć otaczające struktury oraz tkanki, ponieważ wiązka fal ultradźwiękowych może przenikać przez wypełnione płynem mankiety, nie ulegając odbiciu przez granicę powietrze – błony śluzowe.
Introduction
Establishing a secure airway is one of the primary steps during cardiopulmonary resuscitation(1). An endotracheal tube (ETT) usually provides definitive airway control. However, in case of difficult or failed intubation, rapid placement of a laryngeal mask airway (LMA) allows adequate oxygenation and ventilation.
Many methods can be employed to confirm a correct ETT or LMA placement but some may not be reliable in the emergency setting(2). For example quantitative waveform capnography that was recommended in the 2010 ACLS guidelines(1) as the most reliable method of detection may fail in low flow states(3). Recently real-time laryngo-tracheal ultrasonography (US) to confirm correct endotracheal tube placement was shown to be very useful in cadaveric models(4) and during emergency intubation(5). The usefulness of laryngeal mask airway US imaging in an emergency setting and in critically ill patients has not been studied. Due to the variety of different designs, choosing the optimal LMA for any given patient is often challenging. The quality of a seal depends on how accurately the cuff matches dimensions of the laryngeal inlet(6). New methods are needed to assess both the laryngeal size and visualize the LMA in situ. Sonographic upper airway assessment emerges as a practical and easily available noninvasive tool(7) which could be used both for pre-insertion and post-insertion assessments. Sonographic imaging of ETTs or LMAs may be sometimes difficult as their air-containing cuffs generate multiple echoes and US artifacts(2). The primary objective of this study was to develop methods that can enhance echogenicity of ETTs and LMAs and improve detection during emergency US.
Methods
Sheridan # 8 ETT, size 4 LMA Unique (uLMA) and LMA Supreme (sLMA) (LMA North America, Inc.) were:
immersed in a water bath or embedded in gelatin;
placed in the trachea or supraglottic space of pig laryngotracheal specimens;
inserted into the trachea and the upper airway of nonembalmed cadavers.
The BK Medical Flex Focus 400 ultrasound system with 5 MHz curved and 18 MHz linear probes was used for scanning. Pneumatic cuffs of ETTs and LMAs were filled with:
air;
saline;
saline with contrast agents such as sonicated albumin or Optison™ (GE Healthcare).
Results
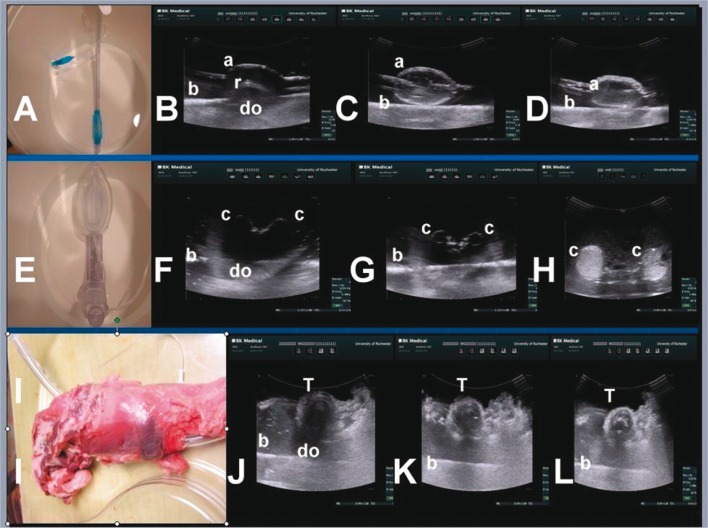
Fig. 1 (upper panel) shows the Sheridan ETT placed in the water bath (A) with the cuff inflated with air (B), saline (C) or saline with Optison™ (D). Air interfaces (a) attenuated US beam (B) causing shadowing artifacts and an image dropout (do), and a reverberation (r). Inflation of the cuff with saline (C) eliminated the shadowing artifact and enabled visualization of the whole cuff and the bottom of the plastic container (b). The image was further improved when saline was mixed with Optison™ (D).
Fig. 1.
Upper panel – Sheridan ETT placed in the water bath (A) with the cuff inflated with air (B), saline (C) or saline with Optison™ (D). Middle panel – similar sequence of images/artifacts when the pneumatic cuff (c) of the LMA Supreme (E) was filled with air (F) saline (G) or saline with Optison™ (H). Lower panel – Sheridan ETT placed in the pig tracheal specimen (I). ETT cuffs were inflated with air (J), saline (K) and saline with Optison™ (L). The saline-filled cuff (K, L) allowed visualization of the tracheal (T) ring; a – air interface, b – bottom of the plastic container, c – cuff, r – reverberation, do – Image dropout, T – tracheal ring
Fig. 1 (middle panel) shows a similar sequence of images/artifacts when the pneumatic cuff (c) of the LMA Supreme (E) was filled with air (F) saline (G) or saline with Optison™ (H).
Fig. 1 (lower panel) shows the Sheridan ETT placed in the pig tracheal specimen (I). ETT cuffs were inflated with air (J), saline (K) and saline with Optison™ (L). The saline-filled cuff (K, L) allowed visualization of the entire tracheal (T) ring.
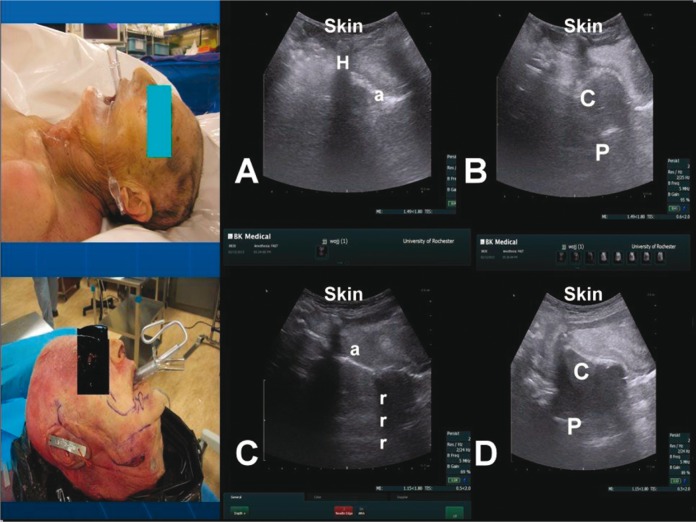
Fig. 2 shows that the ETT (upper panel) and the LMA (lower panel) placed in the cadaveric airway were not visualized when cuffs were inflated with air (A, C). Airmucosa (a) interface of the LMA (C) caused the shadowing artifact. After inflation with saline (B, D) cuffs were visualized as hypoechoic spheres.
Fig. 2.
The endotracheal tube (upper panel) and the laryngeal mask airway (lower panel) placed in the cadaveric airway; H – hyoid bone, r – reverberation, C – cuff, P – posterior wall of the pharynx
Discussion
Capnography is the standard method to confirm correct ETT or LMA placements(3). However, it may be unreliable during cardiopulmonary resuscitation and low flow states which may lead to an unnecessary removal of a well-placed ETT, re-intubation and interruption of chest compressions. Tracheal US does not interrupt chest compressions and is not affected by low pulmonary flow or airway obstruction, but is limited by US scattering and artifacts generated in air-tissue interfaces. This study demonstrates that the replacement of air with saline in ETT or LMA cuffs enables their detection and the visualization of the surrounding structures or tissues and markedly limits US artifacts.
Similar improvement in visualization was obtained in cadavers after filling of the cuffs with saline. Therefore, it is likely that saline-filled cuffs may be detected in patients after endotracheal intubation or placement of the supraglottic airway.
Conflict of interests
The authors do not report any financial or personal links with other persons or organizations, which might negatively affect the content of this publication and claim authorship rights to this publication.
References
- 1.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Part 8. Circulation. 2010;122:729–767. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 2.Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, Huang PC, et al. Tracheal rapid ultrasound exam for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–1284. doi: 10.1016/j.resuscitation.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 3.Adi O, Chuan TW, Rishya M. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J. 2013;5:7. doi: 10.1186/2036-7902-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma G, Davis DP, Schmitt J. The sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007;32:405–407. doi: 10.1016/j.jemermed.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Raphael DT, Conard FU., 3rd Ultrasound confirmation of endotracheal tube placement. J Clin Ultrasound. 1987;15:459–462. doi: 10.1002/jcu.1870150706. [DOI] [PubMed] [Google Scholar]
- 6.Cattano D, Wojtczak J, Seitan C, Aijazi H, Vale H, Altamirano A, et al. Models for predicting laryngeal anatomy and a standardized sizing system for supraglottic airway devices. Anesthesiology. 2012:A784. [Google Scholar]
- 7.Wojtczak J. Submandibular sonography – assessment of hyomental distances and ratio, tongue size, and floor of the mouth musculature using portable ultrasound. J Ultrasound Med. 2012;31:523–528. doi: 10.7863/jum.2012.31.4.523. [DOI] [PubMed] [Google Scholar]