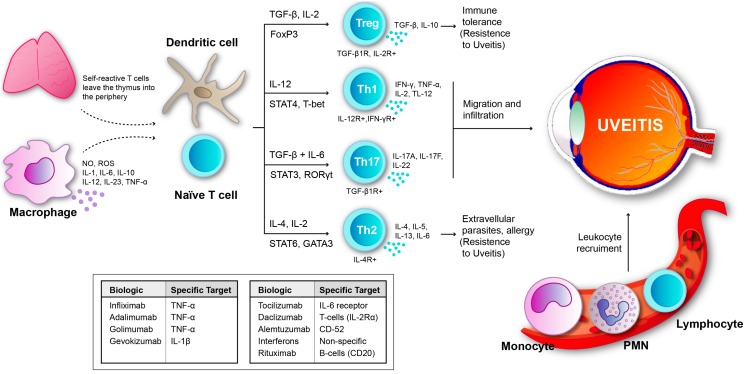
Figure 1.
Uveitis results from imbalance between inflammatory mechanisms and regulatory mechanisms. Acute inflammation initiated by those cells that are previously present in affected tissues, mainly resident macrophages and dendritic cells [12]. In autoimmune uveitis, self-reactive T cells leave the thymus and when they reach the eye they come in contact with retinal antigens. Myeloid dendritic cells present a solid ability of capturing antigens, which enables them to stimulate T cells. Therefore, T-lymphocytes may differentiate into Tregs, Th1, Th17 or Th2 for precise immune response in function of the antigen encountered and cytokine presence. Th1 and Th17 cells participate in inflammatory and autoimmune uveitis. Th1 cells are crucial for the development of uveitis, whereas Th17 cells play a relevant role in the late/chronic phase of uveitis, however induced Treg cells defeat both Th1 and Th17 cell responses [13,14,15,16,17]. Furthermore, the migration of Th1 and Th 17 to the eye, also results in the breaking down of the blood-retinal barrier and, consequently, different leukocytes from the circulation are recruited. In the figure, we can also see the main biologics that are being presently used in uveitis therapy and its targets.