Abstract
The association between polymorphisms of glutathione-related enzyme (GST) genes and the risk of schizophrenia has been investigated in many published studies. However, their results were inconclusive. Therefore, we performed a meta-analysis to explore the association between the GSTM1, GSTT1, and GSTP1 polymorphisms and the risk of schizophrenia. Twelve case-control studies were included in this meta-analysis. The odds ratio (OR) and 95% confidence interval (95% CI) were used to investigate the strength of the association. Our meta-analysis results revealed that GSTM1, GSTT1, and GSTP1 polymorphisms were not related to risk of schizophrenia (p > 0.05 in each model). Further analyses based on ethnicity, GSTM polymorphism showed weak association with schizophrenia in East Asian population (OR = 1.314, 95% CI = 1.025–1.684, p = 0.031). In conclusion, our meta-analysis indicated the GSTM1 polymorphism may be the only genetic risk factor for schizophrenia in East Asian population. However, more meta-analysis with a larger sample size were needed to provide more precise evidence.
Keywords: glutathione S-transferase enzymes, polymorphism, schizophrenia, meta-analysis
1. Introduction
Schizophrenia is a mental disorder that is characterized by abnormal social behavior and altered perception of reality. Several studies suggested that genetic background and environmental factors play an important role in the development of schizophrenia. Recently, there has also been increasing interest in the role of free oxidative stress in the pathogenesis of schizophrenia. Oxidative damage and neuronal inflammation can lead to the onset of schizophrenia [1,2,3,4,5].
Glutathione S-transferases (GSTs) are a family of eukaryotic and prokaryotic phase II metabolic isozymes. GSTs are one of the key enzymes that regulate the conversion of toxic compounds to hydrophilic metabolites for the purpose of detoxification [6,7]. In addition, they play an important role as neuro-protective antioxidants by protecting neural cells from oxidative stress [4,8,9]. GSTs are expressed in many tissues in the human body. Some studies showed that GST levels of the cerebrospinal fluid were decreased in patients with schizophrenia [10]. It suggested that GSTs may play a significant role in the development and progression of schizophrenia.
Human cytosolic GSTs belong to the alpha, zeta, theta, mu, pi, sigma, kappa, and omega classes and the main GSTs genes described as polymorphic in humans are glutathione S-transferase Mu1 (GSTM1), glutathione S-transferase T1 (GSTT1), and glutathione S-transferase P1 (GSTP1) [11,12,13,14]. The GSTM1 gene is located at 1p13.3, and the most common polymorphism in GSTM1 is a deletion of the whole GSTM1 gene with a lack of enzyme activity. The GSTT1 gene is located at 22q11.2, and a homozygous deletion in GSTT1 has also been reported. The GSTP1 gene is located at 11q13, and the functional polymorphism at codon 105 in exon 5 of GSTP1 has been found [11,12,13,14]. These polymorphisms of GSTM1, GSTT1, and GSTP1 have been investigated with various diseases including schizophrenia, hypertension, and capacity for oxidation and detoxification [15,16]. Previous studies showed that GSTM1 or GSTT1 deletion polymorphisms were contributed to the loss of GST enzyme activities, respectively. So, combination in these GSTM1 and GSTT1 polymorphisms have been also investigated in order to find relationship with various diseases.
Up to now, a number of studies have evaluated the association between polymorphisms of GSTs gene and risk of schizophrenia in diverse populations. However, these results from the published studies remain conflicting rather than conclusive.
Therefore, we performed a meta-analysis on all eligible case-control studies to clarify the association between the GSTM1, GSTT1, and GSTP1 polymorphisms and risk of schizophrenia.
2. Results and Discussion
2.1. Study Characteristics
The meta-analysis of this study was included 12 case and control studies. The characteristics from selected studies in GSTM1, GSTT1, and GSTP1 polymorphisms and schizophrenia are summarized in Table 1. The 12 articles included 2742 schizophrenia patients and 2762 control subjects. The number of analyzed articles for GSTM1, GSTT1, and GSTP1 polymorphisms were nine, eight, and four articles, respectively [3,17,18,19,20,21,22,23,24,25,26,27].
Table 1.
Information of eligible studies included in the meta-analysis.
| Authors | Population | Schizophrenia/Control | Schizophrenia | Control | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GSTM1 | GSTT1 | GSTP1 | GSTM1 | GSTT1 | GSTP1 | |||||||||||
| Null | Present | Null | Present | Ile/Ile | Ile/Val | Val/Val | Null | Present | Null | Present | Ile/Ile | Ile/Val | Val/Val | |||
| Harada et al. (2001) [17] | Japanese | 87/176 | 57 | 30 | ND | ND | ND | ND | ND | 87 | 89 | ND | ND | ND | ND | ND |
| Pae et al. (2004) [18] | Korean | 111/130 | 70 | 41 | ND | ND | ND | ND | ND | 61 | 69 | ND | ND | ND | ND | ND |
| Matsuzawa et al. (2009) [19] | Japanese | 214/220 | 129 | 85 | 88 | 127 | 154 | 55 | 5 | 119 | 101 | 80 | 140 | 162 | 54 | 4 |
| Rodríguez-Santiago et al. (2009) [20] | Spanish | 594/585 | 243 | 351 | 142 | 452 | ND | ND | ND | 289 | 296 | 105 | 480 | ND | ND | ND |
| Watanabe et al. (2010) [21] | Japanese | 627/620 | 336 | 291 | ND | ND | ND | ND | ND | 323 | 297 | ND | ND | ND | ND | ND |
| Gravina et al. (2011) [22] | Italy | 138/133 | 82 | 56 | 25 | 113 | 66 | 50 | 8 | 70 | 63 | 30 | 103 | 65 | 48 | 9 |
| Kashani et al. (2012) [23] | Iran | 93/99 | 15 | 78 | 6 | 87 | 48 | 37 | 8 | 26 | 73 | 2 | 97 | 64 | 27 | 8 |
| Kordi-Tamandani et al. (2014) [24] | Iran | 80/71 | ND | ND | 16 | 64 | ND | ND | ND | ND | ND | 34 | 37 | ND | ND | ND |
| Pae et al. (2003) [3] | Korean | 214/110 | ND | ND | ND | ND | 139 | 68 | 7 | ND | ND | ND | ND | 74 | 33 | 3 |
| Raffa et al. (2013) [25] | Tunisia | 138/123 | 79 | 59 | 59 | 79 | ND | ND | ND | 63 | 60 | 67 | 56 | ND | ND | ND |
| Saadat et al. (2007) [26] | Iran | 292/292 | ND | ND | 52 | 240 | ND | ND | ND | ND | ND | 99 | 193 | ND | ND | ND |
| Saruwatari et al. (2013) [27] | Japanese | 154/203 | 77 | 77 | 68 | 86 | ND | ND | ND | 99 | 104 | 99 | 104 | ND | ND | ND |
| Total | - | 2742/2762 | 1091 | 1065 | 456 | 1248 | 407 | 210 | 28 | 1136 | 1153 | 516 | 1210 | 365 | 162 | 24 |
ND, no data; GSTM1, glutathione S-transferase mu 1; GSTT1, glutathione S-transferase theta 1; GSTP1, glutathione S-transferase pi 1.
2.2. Quantitative Synthesis
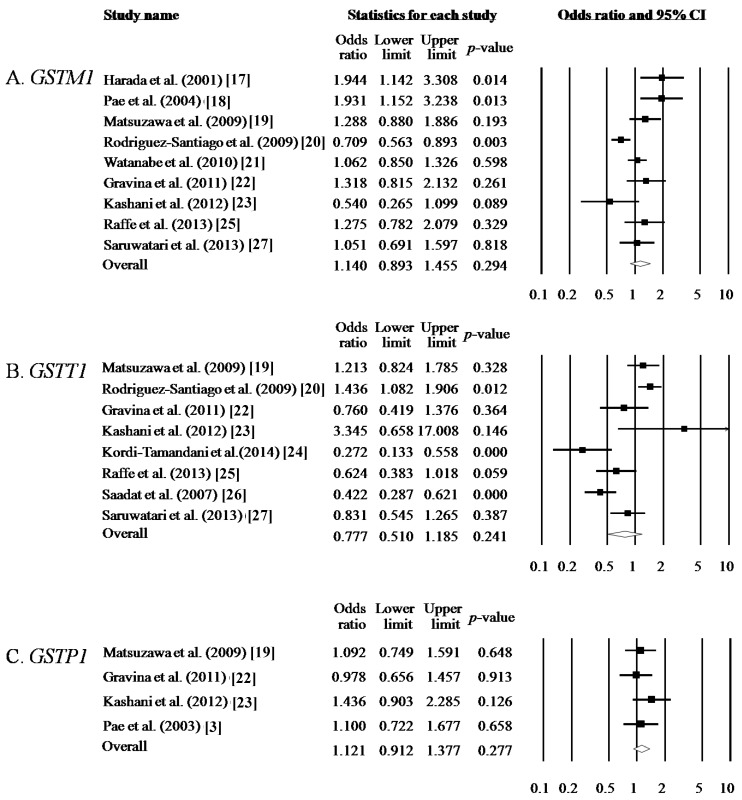
The results of this heterogeneity test for meta-analysis are shown in Table 2. The random-effects method was applied if the result of the Q test was p < 0.05 or I2 statistic was >50%. Otherwise, the fixed-effects method was adopted. For GSTM1 polymorphism, nine studies containing 2156 schizophrenia patients and 2289 control subjects were included. GSMT1 polymorphism did not show any significant association with schizophrenia (null type vs. present type, OR = 1.140, 95% CI = 0.893–1.455, p = 0.294 in Table 2 and Figure 1A). For GSTT1 polymorphism, eight studies containing 1703 schizophrenia patients and 1726 control subjects were included. GSTT1 polymorphism did not show any significant association with schizophrenia (null type vs. present type, OR = 0.777, 95% CI = 0.510–1.185, p = 0.241 in Table 2 and Figure 1B). Combination of GSTM1 and GSTT1 polymorphisms were analyzed using meta-analysis. Combination of Null type in GSTM1 and GSTT1 polymorphisms were compared with combination of other types in GSTM1 and GSTT1 polymorphisms between the schizophrenia group and the control group. Combinations of GSTM1 and GSTT1 polymorphisms were not associated with schizophrenia (OR = 1.241, 95% CI = 0.866–1.777, p = 0.240 in Table 3).
Table 2.
Overall analysis between polymorphisms of glutathione S-transferase genes (GSTM1, GSTT1, and GSTP1) and susceptibility of schizophrenia.
| Gene Symbols | Comparsions | Population | Heterogeneity | Model | OR | 95% CI | p | |
|---|---|---|---|---|---|---|---|---|
| p | I2 | |||||||
| GSTM1 | Null type vs. Present type | All | 0.001 | 70.969 | Random | 1.140 | 0.893–1.455 | 0.294 |
| East Asian | 0.090 | 50.291 | Random | 1.314 | 1.025–1.684 | 0.031 | ||
| GSTT1 | Null type vs. Present type | All | <0.001 | 83.745 | Random | 0.777 | 0.510–1.185 | 0.241 |
| East Asian | 0.194 | 40.655 | Fixed | 1.020 | 0.767–1.355 | 0.893 | ||
| GSTP1 | Ile/Ile vs. Ile/Val | All | 0.487 | 0.000 | Fixed | 1.167 | 0.905–1.504 | 0.235 |
| Ile/Ile vs. Val/Val | All | 0.939 | 0.000 | Fixed | 1.144 | 0.640–2.043 | 0.650 | |
| Ile/Ile vs. Ile/Val + Val/Val | All | 0.533 | 0.000 | Fixed | 1.163 | 0.911–1.484 | 0.227 | |
| Ile/Ile + Ile/Val vs. Val/Val | All | 0.889 | 0.000 | Fixed | 0.771 | 0.435–1.368 | 0.374 | |
| Ile vs. Val | All | 0.666 | 0.000 | Fixed | 1.121 | 0.912–1.377 | 0.277 | |
| Ile/Ile vs. Ile/Val | East Asian | 0.945 | 0.000 | Fixed | 1.082 | 0.779–1.504 | 0.637 | |
| Ile/Ile vs. Val/Val | East Asian | 0.954 | 0.000 | Fixed | 1.279 | 0.490–3.339 | 0.615 | |
| Ile/Ile vs. Ile/Val + Val/Val | East Asian | 0.954 | 0.000 | Fixed | 1.907 | 0.797–1.510 | 0.569 | |
| Ile/Ile + Ile/Val vs. Val/Val | East Asian | 0.982 | 0.000 | Fixed | 0.956 | 0.367–2.490 | 0.927 | |
| Ile vs. Val | East Asian | 0.979 | 0.000 | Fixed | 1.095 | 0.827–1.450 | 0.525 | |
OR, odds ratio; CI, confidence interval; GSTM1, glutathione S-transferase mu 1; GSTT1, glutathione S-transferase theta 1; GSTP1, glutathione S-transferase pi 1.
Figure 1.
Odds ratio and 95% CIs are presented for individual studies (black square and line) and meta-analysis results (diamond). (A) Analysis of null type vs. present type of GSTM1 polymorphism; (B) Analysis of null type vs. present type of GSTT1 polymorphism; (C) Analysis of Val allele vs. Ile allele of GSTP1 polymorphism.
Table 3.
Overall analysis between combination of glutathione S-transferase genes (GSTM1 and GSTT1) and susceptibility of schizophrenia.
| Gene symbols | Combination | Population | Heterogeneity | Model | OR | 95% CI | p | |
|---|---|---|---|---|---|---|---|---|
| p | I2 | |||||||
| GSTM1-GSTT1 | Null type vs. other types | All | 0.958 | <0.001 | Fixed | 1.241 | 0.866–1.777 | 0.240 |
OR, odds ratio; CI, confidence interval.
For GSTP1 polymorphism, four studies containing 659 schizophrenia patients and 562 control subjects were included. The genotype and allele of GSTP1 were also not found to be associated with schizophrenia (codominant, dominant, recessive, and allele models, p > 0.05, respectively in Table 2 and Figure 1C).
When stratified for ethnicity of East Asian, GSTM1 polymorphism showed weak association with schizophrenia (OR = 1.314, 95% CI = 1.025–1.684, p = 0.031). However, there was no association between, GSTT1 or GSTP1 polymorphisms and schizophrenia (p > 0.05 in Table 2 and Table 3).
To identify publication bias in meta-analysis, we evaluated publication bias using Egger’s regression. There was no publication bias (p > 0.05).
2.3. Discussion
Oxidative stress-mediated neuronal damage has been regarded as an important factor in the development of schizophrenia. We supposed that GSTs play an important role in antioxidant defenses by modulating various kinases, and we hypothesized that GSTs are related to the development of schizophrenia. [28,29,30]. In the present study, we examined the association between the polymorphisms of GSTM1, GSTT1, and GSTP1 and the schizophrenia risk. To the best of our knowledge, this is the first meta-analysis to investigate the association between these polymorphisms and the development of schizophrenia.
The correlations between GSTM1, GSTT1, and GSTP1 polymorphisms and the risk of schizophrenia have been investigated in a broad range of studies with either a relatively small or larger sample of the various populations. However, because of the differences in the number of participants and their genetic backgrounds, the evidence provided by each study is not sufficient to draw a convincing conclusion. We conducted a meta-analysis including with 2742 schizophrenia and 2762 controls from 12 case-control studies to evaluate the association between GSTM1, GSTT1, and GSTP1 polymorphisms and the development of schizophrenia.
In our study, there were no significant associations between GSTM1, GSTT1, and GSTP1 polymorphisms and risk of schizophrenia under any genetic model in the total population. Further subgroup analysis by ethnicity also demonstrated that only GSTM1 polymorphism showed weak association with increased the risk of schizophrenia. We should also note the importance of heterogeneity. Heterogeneity was found in some comparisons in our meta-analysis. To get a more full and accurate detail of the precious data, we used the random-effects model. The results were stable with the sensitivity analysis, which did not change the results of the meta-analysis.
Some limitations remain in this meta-analysis and the results should be interpreted with caution. First, meta-analysis is a secondary and retrospective study type that is limited by the quality of primary studies. Second, we were unable to analyze gene-gene and gene-environment interactions.
This study investigated the relationship between GSTM1, GSTT1, and GSTP1 polymorphisms and the development of schizophrenia. In conclusion, we found that GSTM1 polymorphism was associated with susceptibility to schizophrenia in only East Asian population. Further larger studies considering gene-gene and gene-environment interactions are required to provide more precise evidence of the association between GSTM1, GSTT1, and GSTP1 and the risk of schizophrenia.
3. Experimental Section
3.1. Search Strategy
Case and control studies were searched in PubMed, Google, Embase, and Korean databases (KISS, KMbase, and RISS) up to April 2015 without language restrictions. Relevant studies were identified using the terms: “glutathione-related enzyme” or “GSTM, or GSTT, or GSTP” and “polymorphism or polymorphisms” and “schizophrenia”. Only human studies were selected. Additional studies were identified by hand search of original or review articles. If data or data subsets were published in more than one article, only the publication with the largest sample size was included.
3.2. Inclusion Criteria
Studies were included if they met the following criteria: (1) they evaluated the association between the GSTM1, GSTT1, or GSTP1 polymorphisms and schizophrenia; (2) they used a case-control study design; (3) and they contained sufficient distribution of GSTM1, GSTT1, or GSTP1 polymorphism in the schizophrenia group and the control group for the estimation of an odds ratio (OR) with a 95% confidence interval (CI).
3.3. Data Extraction
The two investigators independently extracted data and formed an analysis. When they differed in their conclusions, they rechecked the data again and reached a consensus through discussion. Data extracted from the selected articles included the first author’s name, year of publication, country of origin, ethnicity of the study population, number of cases and controls, and the genotype frequency of GSTM1, GSTT1, or GSTP1 polymorphisms.
3.4. Statistical Analysis
Meta-analysis was performed using a comprehensive meta-analysis software program (Corporation, NJ, USA). The pooled p value, OR and 95% CI were used to investigate the association between risk of schizophrenia and GSTM1, GSTT1, or GSTP1 polymorphisms. Firstly, we calculated the heterogeneity of studies. A χ2-test-based Q statistic test and I2 test were applied. The random-effects DerSimonian and Laird method was adopted if the result of the Q test was p < 0.05 or I2 statistic was >50%, which indicated a statistically significant degree of heterogeneity between the studies. Otherwise, the fixed-effects Mantel-Haenszel method was adopted. Publication bias was evaluated by Egger’s regression.
For meta-analysis of GSTM1 and GSTT1 polymorphisms, the pooled ORs, 95% CI, and p value were calculated using null type versus (vs.) present type. And combination of GSTM1 and GSTT1 polymorphisms were also analyzed in meta-analysis [15]. For GSTP1, the pooled ORs were calculated for codominant 1 model (Ile/Ile vs. Ile/Val), codominant 2 model (Ile/Ile vs. Val/Val), dominant model (Ile/Ile vs. Ile/Val + Val/Val), recessive model (Ile/Ile + Ile/Val vs. Val/Val) and allelic model (Ile vs. Val). Further subgroup analysis by ethnicity, the East Asian population only included Koreans and Japanese. The value of p < 0.05 was regarded to indicate statistical significance.
4. Conclusions
GSTM1 polymorphism was associated with susceptibility to schizophrenia in only East Asian population and GSTT1 and GSTP1 polymorphisms did not related to schizophrenia.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Carter C.J. Schizophrenia susceptibility genes converge on interlinked pathways related to glutamatergic transmission and long-term potentiation, oxidative stress and oligodendrocyte viability. Schizophr. Res. 2006;86:1–14. doi: 10.1016/j.schres.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 2.Mahadik S.P., Mukherjee S. Free radical pathology and antioxidant defense in schizophrenia: A review. Schizophr. Res. 1996;19:1–17. doi: 10.1016/0920-9964(95)00049-6. [DOI] [PubMed] [Google Scholar]
- 3.Pae C.U., Kim J.J., Lee S.J., Lee C.U., Lee C., Paik I.H., Park H.R., Yang S., Serretti A. Association study between glutathione S-transferase P1 polymorphism and schizophrenia in the korean population. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2003;27:519–523. doi: 10.1016/S0278-5846(03)00043-5. [DOI] [PubMed] [Google Scholar]
- 4.Schulz J.B., Lindenau J., Seyfried J., Dichgans J. Glutathione, oxidative stress and neurodegeneration. Eur. J. Biochem. 2000;267:4904–4911. doi: 10.1046/j.1432-1327.2000.01595.x. [DOI] [PubMed] [Google Scholar]
- 5.Yao J.K., Reddy R.D., van Kammen D.P. Oxidative damage and schizophrenia: An overview of the evidence and its therapeutic implications. CNS Drugs. 2001;15:287–310. doi: 10.2165/00023210-200115040-00004. [DOI] [PubMed] [Google Scholar]
- 6.Raunio H., Husgafvel-Pursiainen K., Anttila S., Hietanen E., Hirvonen A., Pelkonen O. Diagnosis of polymorphisms in carcinogen-activating and inactivating enzymes and cancer susceptibility—A review. Gene. 1995;159:113–121. doi: 10.1016/0378-1119(94)00448-2. [DOI] [PubMed] [Google Scholar]
- 7.Roots I., Brockmoller J., Drakoulis N., Loddenkemper R. Mutant genes of cytochrome P-450IID6, glutathione S-transferase class Mu, and arylamine N-acetyltransferase in lung cancer patients. Clin. Investig. 1992;70:307–319. doi: 10.1007/BF00184667. [DOI] [PubMed] [Google Scholar]
- 8.Aoyama K., Watabe M., Nakaki T. Regulation of neuronal glutathione synthesis. J. Pharmacol. Sci. 2008;108:227–238. doi: 10.1254/jphs.08R01CR. [DOI] [PubMed] [Google Scholar]
- 9.Dringen R. Metabolism and functions of glutathione in brain. Prog. Neurobiol. 2000;62:649–671. doi: 10.1016/S0301-0082(99)00060-X. [DOI] [PubMed] [Google Scholar]
- 10.Do K.Q., Trabesinger A.H., Kirsten-Kruger M., Lauer C.J., Dydak U., Hell D., Holsboer F., Boesiger P., Cuenod M. Schizophrenia: Glutathione deficit in cerebrospinal fluid and prefrontal cortex in vivo. Eur. J. Neurosci. 2000;12:3721–3728. doi: 10.1046/j.1460-9568.2000.00229.x. [DOI] [PubMed] [Google Scholar]
- 11.Whitbread A.K., Masoumi A., Tetlow N., Schmuck E., Coggan M., Board P.G. Characterization of the omega class of glutathione transferases. Methods Enzymol. 2005;401:78–99. doi: 10.1016/S0076-6879(05)01005-0. [DOI] [PubMed] [Google Scholar]
- 12.Strange R.C., Spiteri M.A., Ramachandran S., Fryer A.A. Glutathione-S-transferase family of enzymes. Mutat. Res. 2001;482:21–26. doi: 10.1016/S0027-5107(01)00206-8. [DOI] [PubMed] [Google Scholar]
- 13.Hu X., Xia H., Srivastava S.K., Pal A., Awasthi Y.C., Zimniak P., Singh S.V. Catalytic efficiencies of allelic variants of human glutathione S-transferase p1-1 toward carcinogenic anti-diol epoxides of benzo[c]phenanthrene and benzo[g]chrysene. Cancer Res. 1998;58:5340–5343. [PubMed] [Google Scholar]
- 14.Ginsberg G., Smolenski S., Hattis D., Guyton K.Z., Johns D.O., Sonawane B. Genetic polymorphism in glutathione transferases (GST): Population distribution of GSTM1, T1, and P1 conjugating activity. J. Toxicol. Environ. Health B Crit. Rev. 2009;12:389–439. doi: 10.1080/10937400903158375. [DOI] [PubMed] [Google Scholar]
- 15.Lee B.-K., Lee S.J., Joo J.S., Cho K.-S., Kim N.S., Kim H.-J. Association of glutathione S-transferase genes (GSTM1 and GSTT1 ) polymorphisms with hypertension in lead-exposed workers. Mol. Cell. Toxicol. 2012;8:203–208. doi: 10.1007/s13273-012-0025-5. [DOI] [Google Scholar]
- 16.Zare M., Shahtaheri S.J., Mehdipur P., Abedinejad M., Zare S. The influence of CYP1A1 and GSTM1 polymorphism on the concentration of urinary 1-hydroxypyrene in cPAHs exposed iranian anode plant workers. Mol. Cell. Toxicol. 2013;9:303–309. doi: 10.1007/s13273-013-0038-8. [DOI] [Google Scholar]
- 17.Harada S., Tachikawa H., Kawanishi Y. Glutathione S-transferase M1 gene deletion may be associated with susceptibility to certain forms of schizophrenia. Biochem. Biophys. Res. Commun. 2001;281:267–271. doi: 10.1006/bbrc.2001.4347. [DOI] [PubMed] [Google Scholar]
- 18.Pae C.U., Yu H.S., Kim J.J., Kim W., Lee C.U., Lee S.J., Jun T.Y., Lee C., Paik I.H., Serretti A. Glutathione S-transferase M1 polymorphism may contribute to schizophrenia in the korean population. Psychiatr. Genet. 2004;14:147–150. doi: 10.1097/00041444-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Matsuzawa D., Hashimoto K., Hashimoto T., Shimizu E., Watanabe H., Fujita Y., Iyo M. Association study between the genetic polymorphisms of glutathione-related enzymes and schizophrenia in a japanese population. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2009;150B:86–94. doi: 10.1002/ajmg.b.30776. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez-Santiago B., Brunet A., Sobrino B., Serra-Juhe C., Flores R., Armengol L., Vilella E., Gabau E., Guitart M., Guillamat R., et al. Association of common copy number variants at the glutathione S-transferase genes and rare novel genomic changes with schizophrenia. Mol. Psychiatry. 2010;15:1023–1033. doi: 10.1038/mp.2009.53. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe Y., Nunokawa A., Kaneko N., Someya T. A case-control study and meta-analysis of association between a common copy number variation of the glutathione S-transferase mu 1 (GSTM1) gene and schizophrenia. Schizophr. Res. 2010;124:236–237. doi: 10.1016/j.schres.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Gravina P., Spoletini I., Masini S., Valentini A., Vanni D., Paladini E., Bossu P., Caltagirone C., Federici G., Spalletta G., et al. Genetic polymorphisms of glutathione S-transferases GSTM1, GSTT1, GSTP1 and GSTA1 as risk factors for schizophrenia. Psychiatry Res. 2011;187:454–456. doi: 10.1016/j.psychres.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Kashani F.L., Kordi-Tamandani D.M., Sahranavard R., Hashemi M., Kordi-Tamandani F., Torkamanzehi A. Analysis of glutathione S-transferase genes polymorphisms and the risk of schizophrenia in a sample of iranian population. Neuron Glia Biol. 2012;7:199–203. doi: 10.1017/S1740925X12000130. [DOI] [PubMed] [Google Scholar]
- 24.Kordi-Tamandani D.M., Mojahed A., Sahranavard R., Najafi M. Association of glutathione S-transferase gene methylation with risk of schizophrenia in an iranian population. Pharmacology. 2014;94:179–182. doi: 10.1159/000368083. [DOI] [PubMed] [Google Scholar]
- 25.Raffa M., Lakhdar R., Ghachem M., Barhoumi S., Safar M.T., Bel Hadj Jrad B., Haj Khelil A., Kerkeni A., Mechri A. Relationship between GSTM1 and GSTT1 polymorphisms and schizophrenia: A case-control study in a tunisian population. Gene. 2013;512:282–285. doi: 10.1016/j.gene.2012.10.031. [DOI] [PubMed] [Google Scholar]
- 26.Saadat M., Mobayen F., Farrashbandi H. Genetic polymorphism of glutathione S-transferase T1: A candidate genetic modifier of individual susceptibility to schizophrenia. Psychiatry Res. 2007;153:87–91. doi: 10.1016/j.psychres.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 27.Saruwatari J., Yasui-Furukori N., Kamihashi R., Yoshimori Y., Oniki K., Tsuchimine S., Noai M., Sato Y., Nakagami T., Sugawara N., et al. Possible associations between antioxidant enzyme polymorphisms and metabolic abnormalities in patients with schizophrenia. Neuropsychiatr. Dis. Treat. 2013;9:1683–1698. doi: 10.2147/NDT.S52585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arnold S.E., Trojanowski J.Q. Recent advances in defining the neuropathology of schizophrenia. Acta Neuropathol. 1996;92:217–231. doi: 10.1007/s004010050512. [DOI] [PubMed] [Google Scholar]
- 29.Catts V.S., Catts S.V. Apoptosis and schizophrenia: Is the tumour suppressor gene, p53, a candidate susceptibility gene? Schizophr. Res. 2000;41:405–415. doi: 10.1016/S0920-9964(99)00077-8. [DOI] [PubMed] [Google Scholar]
- 30.Kawasak Y., Vogeley K., Jung V., Tepest R., Hutte H., Schleicher A., Falkai P. Automated image analysis of disturbed cytoarchitecture in brodmann area 10 in schizophrenia: A post-mortem study. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2000;24:1093–1104. doi: 10.1016/S0278-5846(00)00131-7. [DOI] [PubMed] [Google Scholar]