Abstract
The American Academy of Sleep Medicine's (AASM) Taskforce on Sleep Telemedicine supports telemedicine as a means of advancing patient health by improving access to the expertise of Board-Certified Sleep Medicine Specialists. However, such access improvement needs to be anchored in attention to quality and value in diagnosing and treating sleep disorders. Telemedicine is also useful to promote professionalism through patient care coordination and communication between other specialties and sleep medicine. Many of the principles and key concepts adopted here are based on U.S. industry standards, with special consideration given to the body of work by the American Telemedicine Association (http://www.americantelemed.org/), and abide by standards endorsed by the American Medical Association (http://www.ama-assn.org/). Practitioners who wish to integrate sleep telemedicine into their practice should have a clear understanding of the salient issues, key terminology, and the following recommendations from the AASM.
The Taskforce recommends the following:
Clinical care standards for telemedicine services should mirror those of live office visits, including all aspects of diagnosis and treatment decisions as would be reasonably expected in traditional office-based encounters.
Clinical judgment should be exercised when determining the scope and extent of telemedicine applications in the diagnosis and treatment of specific patients and sleep disorders.
Live Interactive Telemedicine for sleep disorders, if utilized in a manner consistent with the principles outlined in this document, should be recognized and reimbursed in a manner competitive or comparable with traditional in-person visits.
Roles, expectations, and responsibilities of providers involved in the delivery of sleep telemedicine should be defined, including those at originating sites and distant sites.
The practice of telemedicine should aim to promote a care model in which sleep specialists, patients, primary care providers, and other members of the healthcare team aim to improve the value of healthcare delivery in a coordinated fashion.
Appropriate technical standards should be upheld throughout the telemedicine care delivery process, at both the originating and distant sites, and specifically meet the standards set forth by the Health Insurance Portability and Accountability Act (HIPAA).
Methods that aim to improve the utility of telemedicine exist and should be explored, including the utilization of patient presenters, local resources and providers, adjunct testing, and add-on technologies.
Quality Assurance processes should be in place for telemedicine care delivery models that aim to capture process measures, patient outcomes, and patient/provider experiences with the model(s) employed.
Time for data management, quality processes, and other aspects of care delivery related to telemedicine encounters should be recognized in value-based care delivery models.
The use of telemedicine services and its equipment should adhere to strict professional and ethical standards so as not to violate the intent of the telemedicine interaction while aiming to improve overall patient access, quality, and/or value of care.
When billing for telemedicine services, it is recommended that patients, providers, and others rendering services understand payor reimbursements, and that there be financial transparency throughout the process.
Telemedicine utilization for sleep medicine is likely to rapidly expand, as are broader telehealth applications in general; further research into the impact and outcomes of these are needed.
This document serves as a resource by defining issues and terminology and explaining recommendations. However, it is not intended to supersede regulatory or credentialing recommendations and guidelines. It is intended to support and be consistent with professional and ethical standards of the profession.
Citation:
Singh J, Badr MS, Diebert W, Epstein L, Hwang D, Karres V, Khosla S, Mims KN, Shamim-Uzzaman A, Kirsch D, Heald JL, McCann K. American Academy of Sleep Medicine (AASM) position paper for the use of telemedicine for the diagnosis and treatment of sleep disorders. J Clin Sleep Med 2015;11(10):1187–1198.
Keywords: telemedicine, position paper
1.0 BACKGROUND
There is increasing recognition of the prevalence of sleep disorders and their impact on patients and public health.1,2 Sleep disturbances, either difficulty falling asleep or excessive daytime sleepiness, affect an estimated 35% to 40% of the adult population in the US.3 The cost of these disorders is high; a study performed over a 4-year period ending in 2003 estimated the cost of insomnia through absenteeism and short-term disability claims to be approximately $1,200 higher per patient compared to those without insomnia.4 Likewise, obstructive sleep apnea (OSA) is associated with increased utilization of health care resources, and excess morbidity and mortality.5 Epidemiological studies estimate that the prevalence of OSA has increased, owing to increased prevalence of obesity.6 Shift worker disorder, restless legs syndrome (RLS), and excessive daytime sleepiness and fatigue also carry societal cost burden associated with lack of, or suboptimal, therapy.5
Given the increased recognition, prevalence, and impact of sleep disorders, a broader patient population is likely to need guidance as to optimal diagnosis and treatment options. The AASM fully supports integrated care models, whereby the patient, sleep specialists, primary care providers, and other members of the healthcare team work together to deliver the highest value care. However, with access to a larger treatment population some patients will require specialized expertise. Unfortunately, there is currently a substantial shortage of board-certified sleep medicine providers and other specialists, and parts of the United States are grossly underserved or not served at all. The specialist gap is expected to widen with such measures as the Affordable Care Act.7 According to the American Association of Medical Colleges (AAMC), there will be 46,000 fewer physician specialists available than needed by 2020, based on currently projected residency graduates.8
As the number of those seeking health care expands, and those available to provide it shrinks, more efficient and accessible ways to provide services beyond the traditional office model are needed. Telehealth applications, and telemedicine specifically, are increasingly seen as tools to deliver cost-effective care while increasing accessibility. Sleep medicine already utilizes telehealth applications for diagnosis and monitoring of sleep apnea and CPAP therapy through home sleep testing and monitoring technologies.
The growth of telemedicine services and tools has increased substantially. A recent report of companies with more than 1,000 U.S. employees suggests that from 2014 through 2016, employers are projecting a 68% increase (from 22% to 37%) in the use of telemedicine for consultations as alternatives to office visits and emergency room visits.9 Many institutions and professional societies have advocated for, or adopted, the use of telemedicine tools and applications to help meet the needs of improved access to primary care and specialist providers.10,11
In 2014 the AASM Board of Directors convened a Taskforce to understand and define the key features, processes, and standards for telemedicine specific to sleep medicine. This position paper is not intended to include all aspects of telehealth, and views telemedicine as a subset of telehealth applications.
There is a history of successful use of telemedicine in the diagnosis and treatment of sleep disorders. Recent studies have indicated the acceptance of telemedicine and patient satisfaction in OSA management models including diagnosis via tele-consultation and optimization of management via remote CPAP controls.12 Currently, expansion of sleep telemedicine into all aspects of sleep disorder management is limited by technology resources and facilities able to manage those resources, reimbursement and financial considerations, as well as willingness of physicians, patients and healthcare organizations to accept telemedicine as an alternative to in-office care. This position paper intends to discuss the specific advantages and disadvantages of telemedicine and to provide recommendations for appropriate use of telemedicine for the sleep specialist.
2.0 CLINICAL CONSIDERATIONS
2.1 Methodologies of Patient-Provider Interactions in Sleep Telemedicine
If the organizational, technical, and healthcare professional standards in this document are met, sleep medicine providers are then encouraged by the AASM to utilize telemedicine. In so doing, clinical standards of the AASM Practice Parameters and Clinical Guidelines should be upheld, and telemedicine-based best practices as endorsed by the American Telemedicine Association13 and American Medical Association14 (outline in Appendix 2) should be met.
In general, telemedicine applications can be divided into two categories: synchronous and asynchronous interactions.
2.1.1 Synchronous Live Interactions
Synchronous live interactive telemedicine visits are those in which patients and providers are separated by distance, but interact in real-time utilizing videoconferencing as the core technology. In this modality, the encounter is meant to function as a live office visit. Participants are separated by distance, but interact synchronously with the provider performing sleep medicine interviews of the patient, and diagnostic and treatment options are addressed through live video interaction between the patient and the provider. By convention, the site where the patient is located is referred to as the originating site and the site where the consultant is located is referred to as the distant site (may also be referred to as the destination site). The originating site may include, but will not necessarily be limited to, a provider's office, a sleep laboratory, or even the patient's home as long as the site is secure and upholds the technical and privacy standards described in this document. Similarly, the distant site is where the provider performing the clinical evaluation is located, and can be wherever a secure, private telecommunications channel that meets the technical requirements is located.
There are specific considerations for this modality including, but not limited to, the following:
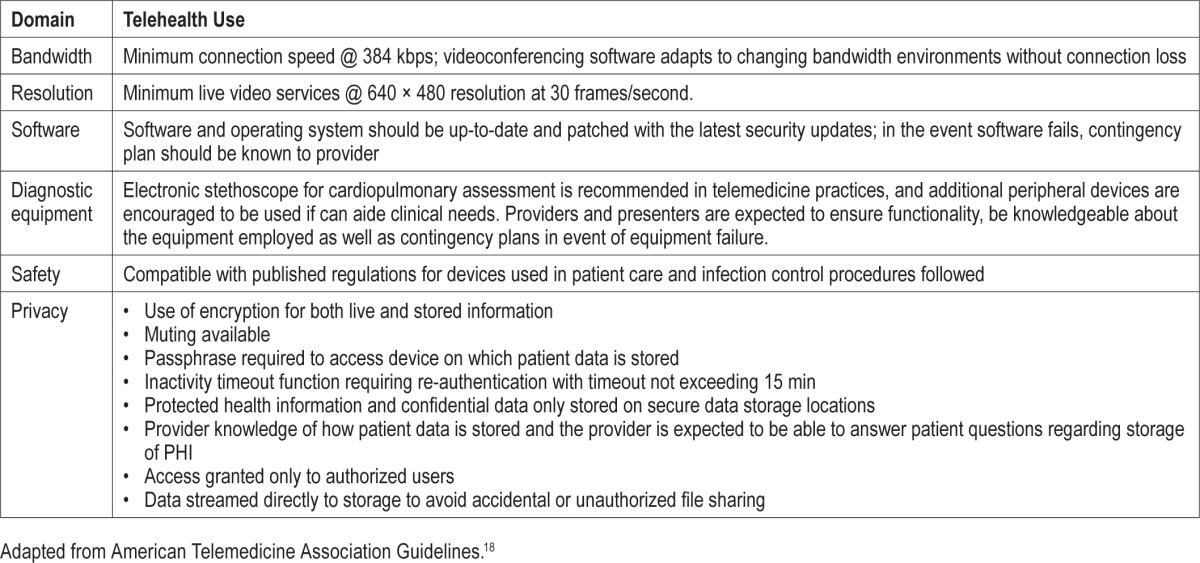
Technical abilities to enable this form of telemedicine include a robust telecommunications portal with appropriate bandwidth and backup systems (refer to Table 1 for minimal technical standards).
Documentation standards, including counseling for any testing and therapies employed, and prescriptions standards for this type of encounter should mirror those of in-person visits.
Reimbursement should be clarified with payors prior to providing telemedicine services.
- Regulations regarding telemedicine for Medicare and Medicaid patients which specify patient and service eligibility, required equipment, and required location to provide service. Reimbursement for these services will only occur when:
- Delivered by real-time, interactive, audio-video telecommunications system (not telephone, email, facsimile, or asynchronous interactions).
- The originating site is an approved site (practitioner office, critical access hospital, rural health clinic, federally qualified health center, hospital, skilled nursing facility, or community mental heal center) located in a health professional shortage area (HPSP) or outside of a metropolitan statistical area (MSA).
- The distant site provider is a physician, nurse practitioner, physician assistant, nurse midwife, clinical nurse specialist, clinical psychologist, or registered dietician
- Billing is performed using the appropriate Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) code plus the GT telehealth modifier.
- For details on requirements and eligible services, please refer to Appendix 3 or http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/TelehealthSrvcsfctsht.pdf
Table 1.
Technical requirements for sleep telemedicine.
2.1.2 Asynchronous Interactions
Asynchronous interactions via telemedicine refer to those encounters in which the patient and the provider are not only separated by distance, but also by time, meaning that key aspects of the clinical encounter were performed at separate times. There are several types of asynchronous interactions including (1) Remote Interpretation with Store-and-Forward Systems, (2) E-messaging, and (3) Self-care models of care delivery, each of which is discussed below.
There are several key aspects regarding the use of asynchronous care models:
It is important to clearly define the patient-provider relationships in any care model that utilizes this form of interaction, and explicitly document the assumptions parties may have in such encounters and roles.
There should be the ability to arrange a patient presenter, live-interactive telemedicine visits, or even face-to-face office visits when needed.
Reimbursement models for this form of care delivery are currently not provided in sleep medicine per the Taskforce's knowledge. Readers are referred to documents from the ATA as they are updated.14
Special consent may be required when physical examination is not performed, and informed consent from the patient should include the understanding that the patient is aware of the limitation of this approach.
The organizational and technical infrastructure for secure electronic communication and record keeping should align with the standards set forth in this document. Attention to secure telecommunications that ensure safety and meet technical standards outlined elsewhere in this document still apply.
2.1.2.1 REMOTE INTERPRETATION USING SLEEP TELEMEDICINE WITH STORE-AND-FORWARD SYSTEMS
This refers to a method of providing consultations and clinical decision-making to referring providers or patients, rather than direct, interactive care to patients. A sleep medicine history with certain diagnostic/therapeutic data are collected at the point of care and transmitted to the sleep medicine provider for review. In turn, the sleep medicine specialist provides clinical advice via a written or electronic report to the referring provider within a reasonable time frame to make clinical decisions. The data stored can include an array of medical records, images of anatomical findings, sleep study data with/without video recordings, PAP device data or other data, and mobile technologies. An example could include requests from primary care providers or other clinicians for the sleep medicine provider to review a patient's record for a specific clinical question without the provider examining the patient formally.
2.1.2.2. E-MESSAGING
E-messaging (e.g., through email or online asynchronous technologies) refers to the ability for health providers to respond or interact with patients asynchronously through a secure electronic channel. E-messages are typically member-initiated (the member being the patient or family member), and historically have been used to address non-urgent ongoing or new symptoms. There is a growing body of literature on the use of e-messaging, and an increasing utilization of this type of care model. In this type of care model, the origination site is wherever the patient is linked to the provider electronically. The destination site is the sleep medicine provider who may be at any electronic portal, but the interaction between patient and provider does not occur in real time.
2.1.2.3 SELF-DIRECTED CARE MECHANISMS
Self-directed care mechanisms are increasingly being utilized, in which patients have direct access to interactive feedback, coaching, or other sleep-related care mechanisms that do not directly involve interaction with the sleep provider. Examples currently include online programs related to cognitive-behavioral therapies, programs that optimize adherence to PAP therapies, smartphone applications of sleep-wake data, etc. The taskforce believes these may likely have more important roles in managing the health of patients with sleep disorders in the future. However, the AASM believes that if used for treatment decisions: (1) the information from these systems must be easily available to the ordering physician, and (2) the time spent on managing data, quality-assurance, and other aspects of care delivery should be remunerated as value-based payment schemes are developed.
2.2 The Sleep Patient Evaluation, Diagnostic Testing, and Treatment
-
Initial Clinical Consultation for Sleep Disorders
Providers should perform key elements of the sleep-relevant medical history as if the visit were an in-person visit. Clinical services should be provided in accordance with the AASM Clinical Practice Guidelines (http://aasmnet.org/practiceguidelines.aspx).
-
Diagnostic Testing Standards
Sleep diagnostics should be performed in a manner that is in accordance with standards, clinical practice guidelines, and practice parameters established by the AASM. Home sleep apnea testing (also called “out-of-center,” “portable,” or “unattended”) devices are to be used when clinically appropriate in a manner that is consistent with current clinical standards. Providers' offices and patients are encouraged to review a patient's individual payor plans when considering diagnostic testing.
-
Interpretation of Sleep Studies
Interpretation of sleep studies should be in accordance with the AASM Manual for the Scoring of Sleep and Associated Events. Sleep providers may make patient-specific recommendations within the interpretation statements to help guide referring providers in key elements of patient management; such statements should ensure consistency with current accreditation and CMS standards.
-
Prescription therapies of Sedative Hypnotics, Stimulant Medications, Wakefulness Promoting Medications, and/or other Controlled Substances
The Taskforce endorses the use of live interactive telemedicine as a suitable alternative for patients for prescription of sedative hypnotics, stimulant medications, wakefulness-promoting medications, or other controlled substances prescribed by the sleep provider.13 Some states do not allow for controlled substances to be prescribed to patients that the provider has not seen in a face-to-face encounter. However, in the event that the provider is allowed and comfortable prescribing such medications, the following principles are recommended:- There is consistent and clear electronic documentation by the referring provider regarding the evaluation and management plan for such patients.
- Providers have an active current license in the state in which the substance is being prescribed (i.e., the originating site).
- Providers adhere to federal, state, and local guidelines regarding prescription practices for controlled substances.
- Clinical judgment regarding the abilities and limitations of telemedicine be considered (see section 2.3 in this paper)
-
Patient Education
The Taskforce endorses the use of telemedicine applications for education of patients with regard to all aspects of sleep care, including diagnostic tests and treatment.
-
Follow-up Visits of Sleep Disorders
Documentation of therapeutic adherence will be the responsibility of the provider who prescribes the initial therapy. In the case of PAP therapies, sleep providers are encouraged to assist their referring providers and affiliated durable medical equipment companies (DME) to monitor and improve PAP adherence as well as be available for follow-up visits as per current clinical standards. Providers should perform key elements of the follow-up evaluation as if the visit were in person. The Taskforce expects that live interactive telemedicine visits, coordinated with PAP download data, are most often sufficient to meet the standards for PAP troubleshooting and adherence in lieu of face-to-face visits. The Taskforce encourages payors to adopt reasonable reimbursement policies for this model of care delivery.
2.3 Methods to Enhance Clinical Decision-Making in Telemedicine
There are a number of mechanisms that may be used to enhance the abilities of providers to more accurately diagnose and treat sleep disorders especially where clinical uncertainty exists. In addition, payors, regulators, or organizations may have different requirements regarding information needed for purposes of either reimbursement and/or quality assurance. Sleep providers are encouraged to explore the resources available, whether such methods are to be used directly or indirectly through other providers/services, and also consider the costs to the patient, provider, and organization when employing these methods. Although not mandatory, sleep providers may consider utilizing one or more of the following resources as needed/available:
-
Patient Presenters
A patient presenter is an individual who can facilitate the communication between the patient at the originating site, and the provider at the distant site. For instance, a medical office assistant may move the patient in front of the camera, ensure the system is working correctly, clarify the questions or tasks for the patient through the interview, and perform technical adjustments of the equipment depending on the needs of the situation. The presenter can help gather ancillary information efficiently, clarify the information transmitted, connect telemedicine tools such as electronic stethoscopes, and perform a number of adjunct roles at the originating site. Depending on the scope of practice of the individual in this role, the services of the patient presenter may be of additional clinical and experiential value, such as assisting with the performance of elements of the physical exam or educating the patient about the provider's recommendations.
-
Locally Available Providers (including Primary Care providers, Specialists, and Subspecialists)
Local resources may exist in a number of disciplines related to sleep health that the sleep medicine provider may be able to utilize if clinically warranted. In addition, sleep providers may consider hiring and developing their own local staff (e.g., Nurse Practitioner or Physician Assistant) to support specific needs and serve as a local resource.
-
Questionnaires and Self-care Tools
Such asynchronous tools may provide important diagnostic and treatment information; the information from these should be easily accessible to the sleep provider.
-
Detailed PAP Download Data
As PAP device manufacturers have provided increasingly sophisticated download data (e.g., detailed physiological information, pressure adjustments, leak information), such information may provide important insight into diagnosing and treating sleep disorders. Methods to maximize physician access to this information should be developed and encouraged. Determining clinical decisions based on PAP download data information should be consistent with current standards of care for patients cared for in current clinical arrangements between the patients, providers, DME offices, and others. We expect these standards to evolve15 and for telemedicine practices to also evolve to incorporate such data to enhance access, quality, and efficiencies of care.
-
Ancillary Diagnostic Testing
Sleep providers should consider using additional testing such as radiography, spirometry, electrocardiography and/or echocardiography, home oximetry, or other tests depending on specifics of the clinical situation.
-
Use of Peripheral Devices and Wearable technologies
Increasingly, technologies such as electronic stethoscopes to auscultate heart and lung sounds are available to providers. If a cardiopulmonary examination is needed, the use of a patient presenter and electronic stethoscope may provide a sufficient examination as long as the sleep provider assesses the accuracy of the examination. Other peripherals to consider include actigraphy technologies, wearable devices (although the validity of these devices is not uniformly proven), and other hardware/software combinations that aide the clinician in diagnostic and treatment decisions.
3.0 QUALITY ASSURANCE IN SLEEP TELEMEDICINE
Telemedicine care should reflect the same standards as face-to-face care, but the Taskforce also recommends additional Quality Assurance (QA) processes that specifically address telemedicine tools, processes and applications. The AASM has developed quality measures for five sleep disorders (Adult OSA, Pediatric OSA, RLS, Insomnia, and Narcolepsy) that specifically address the data elements to be captured. Providers and organizations are also encouraged to develop and maintain a QA process that addresses domains that relate to:
Process measures—demonstrate that appropriate steps were taken by the healthcare provider during each telemedicine visit/service to ensure optimum care. These should mirror, as much as possible, current accepted standards for live visits, and include telemedicine-specific processes outlined here and in other guidelines (e.g., the ATA's Core Operational Guidelines for Telehealth Services Involving Provider-Patient Interactions.)
Patient-centered outcomes—consider measures of patient satisfaction, symptom assessments, and treatment adherence. These should mirror current accepted standards for live visits.
Overall provider experience—staff and referring provider satisfaction with the telemedicine services rendered.
Technical ease, reliability, and safety should be specifically addressed in the data assessments above.
Compliance with the Health Insurance Portability and Accountability Act (HIPAA) is of high importance, and use of encrypted communications and storage mechanisms is a requirement, as are clear contingency plans in the event of loss of communications.
4.0 ROLES AND RESPONSIBILITIES OF OTHER HEALTHCARE MEMBERS
4.1 Advanced Clinical Practitioners
Advanced Clinical Practitioners (ACPs, specifically Nurse Practitioners [NPs] and Physician Assistants [PAs] for the purposes of this document), and other providers specifically trained in sleep should follow the same professional standards as outlined elsewhere in this document for the sleep physician. In general, the standards for supervision should follow the same general guidelines as those for ACPs working with physicians in the live setting. Medicare rules and guidelines are often cited to clarify the scope, practice, and reimbursement of ACPs in medical arenas, and some professional societies have adopted additional guidelines to assist clarification.16 But as these are in flux, all providers involved are encouraged to review their facilities' and institutions' bylaws and human resource documents. Moreover, relevant regulatory documents related to the provision of care are to be followed, and providers and organizations are to ensure such care is consistent with policies regarding scope of practice and state licensing laws of all involved parties.
Physicians and practices should be cognizant of the relationship between ACPs, physicians, and the practices involved; moreover the roles and responsibilities of each should be explicitly communicated. Physician Assistants (PAs) at the time of this printing, are nearly always in a supervisory relationship with a physician, and in many states the same is true for NPs.
Supervision includes, but is not limited to:
The continuous availability of direct communication either in person or by electronic communications between the non-physician practitioner (NPP) and supervising physician
Personal review of the NPP's practice at regular intervals including an assessment of referrals made or consultations requested by the NPP with other health professionals
Regular chart review
The delineation of a plan for emergencies
The designation of an alternate physician in the absence of the supervisor
A review plan for narcotic/controlled substance prescribing and formulary compliance.
The circumstance of each practice determines the exact means by which responsible supervision is accomplished. Moreover, it is the responsibility of the physician to ensure that appropriate directions are given, understood, and executed.16 These directions may take the form of written protocols, in person, over the phone, or by some other means of electronic communication. In all cases, the activities must be consistent with applicable state laws and regulations governing NPPs.
Generally speaking, the taskforce believes that asynchronous and synchronous applications in telemedicine can be used to enhance communication and medical decision-making of the ACP, thereby augmenting ACPs' ability to participate in providing higher-quality sleep medical care. In terms of coding, compliance, and billing, however, it is worth noting what CMS has defined as the three main distinct forms of supervision17:
- General supervision: The physician must be available by telephone to provide assistance and direction if needed.
- The Taskforce believes that Telemedicine can be readily used to augment general supervision, and that asynchronous methods may be employed.
- Direct supervision: The physician must be “immediately available” and “interruptible” to provide assistance and direction throughout the performance of the procedure; however, he or she does not need to be present in the room when the procedure is performed
- The Taskforce believes that if the physician at the distant site views the patient-ACP encounter real-time through a live-interactive telemedicine visit, this should be considered sufficient to meet the definition of direct supervision for purposes of documentation, billing, and compliance.
- Personal supervision: The physician must be in attendance in the room during the procedure.
- At this time, the Taskforce does not believe that telemedicine tools and applications meet this definition of personal supervision.
In any arrangement, quality assurance processes should be in place to monitor the performance of ACPs that specifically address the telemedicine processes and methodology employed.
4.2 Respiratory Care Practitioners and Sleep Technologists
Respiratory Care Practitioners (RCPs, also known as Respiratory Therapists) and Sleep Technologists (STs) that are involved in the care of sleep patients are likely to serve key roles to support a sleep telemedicine program. These individuals should follow the same professional standards as outlined elsewhere in this document, even though these individuals may not operate under the license of a physician. In general, the standards for supervision should follow the same general guidelines as those for RCPs and STs working with physicians, offices, and HME companies in the live setting. All providers involved are encouraged to review their facilities' and institutions' bylaws, human resource documents, and relevant regulatory documents related to the provision of care, and ensure such care is consistent with policies regarding scope of practice and state licensing laws of all involved parties.
4.3 Patient Presenters
Telehealth encounters may require the distant provider to perform an exam of a patient from many miles away. If a patient presenter is utilized, an individual with a clinical background trained in the use of the equipment must be available at the originating site to properly position the patient, manage the cameras and perform any activities to successfully allow the provider to complete the exam. This must be performed in a manner that is within the limits of the individual's license and clearly defined scope of practice, and additional training should be obtained if necessary. For example, a nurse may apply the diaphragm of an electronic stethoscope to the patient's chest so that the distant provider can auscultate heart and lung sounds. It should be noted that in certain cases, such as interview-based clinical consultations, a licensed practitioner might not be necessary, and a non-licensed provider such as support staff, could provide tele-presenting functions.
Patient presenters should be knowledgeable about the technical aspects of daily equipment operation, and should be versed in basic troubleshooting and contingency plans in the event of operation failure.
The following individuals may function in the role of Patient Presenters provided the proper skills and qualifications are met, and the function is defined within the individual's scope of practice:
Physician
Nurse Practitioner
Physician Assistant
Respiratory Therapist
Sleep Technologist
Certified Nurse Specialist
Licensed Practice Nurse
Registered Nurse
Medical Office Assistant
5.0 ETHICAL AND LEGAL CONSIDERATIONS WITH SLEEP TELEMEDICINE
The methods with which telemedicine and its equipment or training is used should adhere to strict professional and ethical standards so as (1) not to violate the intent of the telemedicine interaction and (2) to improve overall patient access, quality and/or value of care. The AASM does not endorse telemedicine practices that violate the professional and ethical standards that are outlined in this document nor those that violate the patient-provider relationship and general public trust. The following domains warrant specific attention:
-
Financial Conflicts or Perceived Conflicts of Interest
Medicare addresses anti-kickback statutes which apply to telemedicine services wherein providers are restricted from providing equipment or services solely to induce referrals or services reimbursable by Medicare. In a similar manner, the Office of the Inspector General (OIG) guidelines limit the use of equipment provided for telemedicine exclusively to telemedicine and not for personal use. Providers should be cognizant of any specific anti-kickback or health care abuse laws applicable in the state in which the patient is being treated. Examples of possible restrictions include:- Restrictions on sleep physicians providing free telemedicine equipment and telemedicine referrals to primary care practices in return for exclusive referrals for federal health care reimbursable services.
- Restrictions on sleep physicians receiving financial benefits including free hardware, software, and training. If any of the above are provided by an entity which then benefits from referrals due to the supplied items or services, Stark law provisions may be violated. In addition, at this time, providers must be licensed in each state in which patients to be treated are located, and, consistent with that, providers should be cognizant of any specific anti-kickback or health care abuse laws applicable in that state.
-
Establishing and Defining the Patient-Physician Relationship
A physician-patient relationship occurs when others contract the physician for health services rendered for the patient's benefit, either with express or implied consent. Therefore, sleep providers who are interpreting studies and answering advice via live interactive telemedicine visits are, in effect, establishing physician-patient relationships.- The telemedicine encounter also establishes a physician-patient relationship such that unilaterally severing ties without notice or not providing alternative medical care if indicated results in patient abandonment.
- The Taskforce recommends every sleep medicine provider be explicit with the referring provider about roles and responsibilities regarding important domains of care delivery, and actively clarify such issues with referring and local providers of the patients. By the same token, if and when severing ties with patients occurs, this should occur through traditional channels and processes as if a patient received a face-to-face visit with the practitioner.
-
Technical Knowledge Deficiencies
Providers are expected to know how to use the telemedicine equipment appropriately; if improper use or lack of training on the equipment affects proper patient assessment and harm occurs, malpractice may exist.
-
Malpractice Insurance
The Taskforce considers telemedicine activities equivalent to face-to- face visits, when adhering to stated guidelines, but recommends providers contact their insurance providers for clarity.
-
Compliance with all aspects of the Health Insurance Portability and Accountability Act (HIPAA)
HIPAA is of high importance, and use of encrypted communications and storage mechanisms is a requirement, as are clear contingencies plans in the event of loss of communications.
6.0 FUTURE VISION OF TELEMEDICINE APPLICATIONS IN SLEEP
Telemedicine applications and roles will expand as the technologies and care models evolve. Potential areas of expansion include high-risk population management such as hospitalized patients with sleep disorders, wearable device technology, bundled payment schemes, integrative care models of delivery, wellness programs, and in-home diagnostic and treatment services. Further research is needed regarding the utilization of such telemedicine applications including comparisons between in-person and telemedicine visits, patient and physician satisfaction, outcome measures, and when “hybrid” models of care (in-person and telemedicine visits) may be required.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Epstein has served as a consultant for AIM Specialty Health and eviCore Healthcare, and has received salary from Welltrinsic Sleep Network Inc. Ms. McCann and Mr. Heald are employees of the American Academy of Sleep Medicine. The other authors have indicated no financial conflicts of interest.
Disclaimer: This document is intended to be for informational and educational purposes only. It is not intended to establish a legal, medical, or other standard of care. Individual physicians should make independent treatment decisions based on the facts and circumstances presented by each patient. The information presented herein is provided “as is” and without any warranty or guarantee as to accuracy, timeliness, or completeness. AASM disclaims any liability arising out of reliance on this position paper for any adverse outcomes from the application of this information for any reason, including, but not limited to, the reader's misunderstanding or misinterpretations of the information contained herein. Users are advised that this position paper does not replace or supersede local, state, or federal laws. As telemedicine laws vary by state, this document is not a substitute for attorney or other expert advice regarding your state law, policies and legal compliance with applicable statutes. The material in this document is based on information available at the time of publication. As laws and regulations continually change, practitioners must keep themselves informed of changes on an ongoing basis.
APPENDIX 1. GLOSSARY
Asynchronous: Sometimes used to describe store and forward transmission of medical images or information because the transmission typically occurs in one direction in time. This is the opposite of synchronous.
Distant site: The site where the provider who is performing the telehealth function (e.g. the board-certified sleep provider) is located.
E-messaging: The ability for health providers to respond or interact with patients or other healthcare providers through a secured electronic channel asynchronously (e.g., email, online medical evaluations, etc.).
Face-to-face visits: Traditional in-office visits where providers evaluate, diagnose and treat patients in an exam room with the patient.
Live interactive telemedicine: Real-time, synchronous encounters through a videoconferencing platform between the patient and the clinical provider.
Originating site: The originating site is where the patient and/or the patient's physician is located during the telehealth encounter or consult. Other common names for this term include spoke site, patient site, remote site, and rural site.
Presenter (patient presenter): An individual at the originating site who facilitates the patient's interaction with the audio-visual equipment to enhance the telemedicine encounter (see section 4.3 in this paper).
Store and forward (S&F): S&F is a type of telehealth encounter or consult that uses still digital images of a patient for the purpose of rendering a medical opinion or diagnosis. Common types of S&F services include radiology, pathology, dermatology, and wound care. Store and forward also includes the asynchronous transmission of clinical data, such as CPAP download data and sleep study reports, to another site (e.g., to another provider, home health agency, hospital, clinic).
Synchronous: Sometimes used to describe interactive video connections because the transmission of information in both directions is occurring at exactly the same time period.
Telehealth: Electronic exchange of medical information to improve a patient's health status. This is a broader concept than telemedicine.
Telemedicine: A legal patient/clinician encounter using electronic communication.
APPENDIX 2. CORE STANDARDS FOR TELEHEALTH IN GENERAL
Adapted from the American Telemedicine Association's Guidelines 201413,18
1.0 Organizational Standards
Organizations providing telemedicine services should follow the standard operating policies and procedures of the governing institution, and may consider specifically addressing telemedicine-specific issues regarding federal, state, and other credentialing and regulatory agency requirements. Additional attention may be needed in regards to understanding resource management, privacy and confidentiality, and documentation.
Organizations and health professionals providing telemedicine services should ensure compliance with relevant legislation, regulations, and accreditation requirements for supporting patient/client decision-making and consent, including protection of patient health information.
Organizations providing Tele-Sleep services should have in place a systematic quality improvement and performance management process that complies with any organizational, regulatory, or accrediting requirements for outcomes management.
Organizations should have a mechanism in place for assuring that patients are aware of their rights and responsibilities with respect to accessing health care via telemedicine technologies, including the process for communicating complaints.
Organizations providing telemedicine services that establish collaborative partnerships should be aware of applicable legal and regulatory requirements for appropriate written agreements, memorandum of understanding, or contracts. Those contracts, agreements, etc., should be based on the scope and application of the telemedicine services offered, and should address all applicable administrative, clinical, and technical requirements.
Organizations should ensure that whenever feasible, patients are given choices of providers, and that informed consent for telemedicine encounters, including the option to decline telemedicine encounters, is clearly documented. Documentation of such informed consent should be made available.
2.0 Healthcare Professional Standards
Health professionals providing telemedicine services should be fully licensed and registered with their respective regulatory/licensing bodies and with respect to the site where the patient is located.
Health professionals should be aware of their locus of accountability and any/all requirements (including those for liability insurance) that apply when practicing telemedicine in another jurisdiction.
Health professionals using telemedicine should be cognizant of when a provider-patient relationship has been established within the context of a telemedicine encounter between the health care provider and the patient and proceed accordingly with an evidence-based, value-based, and best possible standard of care.
Health professionals providing telemedicine services should have the necessary education, training/orientation, and ongoing continuing education/ professional development to ensure they possess the necessary competencies for the safe provision of quality health services in their specialty area.
Nurse Practitioners and Physician Assistants practicing under the license of the supervising sleep medicine physician should follow the same professional standards as outlined for the sleep physician.
3.0 Technical Standards
Organizations should ensure that equipment sufficient to support diagnostic needs is available and functioning properly at the time of clinical encounters.
Organizations should comply with all relevant safety laws, regulations, and codes for technology and technical safety.
Organizations should have infection control policies and procedures in place for the use of telemedicine equipment and patient peripherals that comply with organizational, legal, and regulatory requirements.
Organizations providing telemedicine services should have policies and procedures in place to comply with local legislated and regulatory rules for protection of patient health information and to ensure the physical security of telemedicine equipment and the electronic security of data.
Organizations should have appropriate redundant systems in place that ensure availability of the network for critical connectivity, and if such systems are not functional then a back-up plan and communication of this plan to patients and levels of the organization affected.
Organizations should have appropriate redundant clinical video and exam equipment for critical clinical encounters and clinical functions. A back-up plan for critical encounters and communication of that plan is also recommended before and during employment.
Organizations should meet required published technical standards for safety and efficacy for devices that interact with patients or are integral to the diagnostic capabilities of the practitioner when and where applicable.
Organizations providing telemedicine services should have processes in place to ensure the safety and effectiveness of equipment through ongoing maintenance.
APPENDIX 3. SPECIFICS OF MEDICARE AND UTILIZATION OF TELEMEDICINE
1.0 Introduction
When Congress passed the Balanced Budget Act of 1997, this included the mandate that Medicare should begin reimbursement for telemedicine services. Telemedicine services that are covered under Medicare Part B are defined under Title 42, Chapter IV, Subchapter B, Part 410.78. The Center for Medicare & Medicaid Services (CMS) administers the Medicare program and additional questions can be referenced at http://www.medicare.gov and http://www.cms.gov/Medicare/Medicare-General-Information/Telehealth.
Listed below are relevant considerations for the sleep specialist when providing telemedicine care specifically to Medicare patients, but please be advised to consult current Medicare requirements as specifics of this program may change. It is also important to note that state law establishes what telemedicine services each provider of telemedicine may furnish; therefore, providers should check with their individual state governing bodies.
2.0 Eligibility for Coverage
To qualify for Medicare coverage of telemedicine services, there are several specific eligibility criteria:
Live-interactive visits only are covered in which there is clear distance separation from the patient and provider
Only fee-for-service patients are eligible (Medicare will not reimburse for beneficiaries under capitated plans).
Patient must be “presented from an originating site located in either a Rural Health Professional Shortage Area (HPSA) [as defined by §332(a)(1) (A) of the Public Health Services Act] or in a county outside of a MSA [Metropolitan Statistical Area, as defined by §1886(d) (2)(D) of the Act].” The US Department of Health and Human Services Health Resources and Services Administration (HRSA) developed a tool, called “the HRSA Medicare Telehealth Payment Eligibility Analyzer,” to help providers determine geographic eligibility for Medicare telemedicine services. This locator checks both the HPSA and the MSA designations and can be found at: http://datawarehouse.hrsa.gov/telehealthAdvisor/telehealthEligibility.aspx
3.0 Medicare Definitions of Shortage Areas
- A health professional shortage area is defined in 42 U.S.C. § 254e as:
- An area in an urban or rural area (which need not conform to the geographic boundaries of a political subdivision and which is a rational area of the delivery of health services) which the Secretary determines has a health manpower shortage and which is not reasonably accessible to an adequately served area
- A population group which the Secretary determines has such a shortage, or
- A public or nonprofit private medical facility or other public facility, which the Secretary determines, has such a shortage
A metropolitan statistical area is defined as an urbanized area with a population of 50,000 or more.
Exception to rural HPSA and non MSA geographic requirements: Entities participating in a Federal telemedicine demonstration project that were approved by or were receiving funding from the Secretary of Health and Human Services as of December 31, 2000, qualify as originating sites regardless of geographic location. Such entities are not required to be in a rural HPSA or non-MSA.
4.0 Medicare Definitions of Originating and Distant Sites
An originating site is the location of an eligible Medicare beneficiary at the time the service being furnished (via a telecommunications system) occurs. Originating sites authorized by law include:
The office of a physician or practitioner
A hospital (as defined in section 1861(e) of the Act)
A critical access hospital (CAH) [as described in section 1861(mm)(1) of the Act]
A rural health clinic (as described in section 1861(aa)(2) of the Act)
A federally qualified health center [as described in section 1861(aa)(4) of the Act]
Skilled Nursing Facility (SNF) [as defined in section 1819(a) of the Act]
Community Mental Health Center (CMHC) [as defined in section 1861(ff)(3)(B) of the Act]
Distant site practitioners who may administer and receive payment for covered telemedicine services are:
Physicians as described in § 410.20
Physician assistants (PA) as described § 410.74
Nurse practitioners (NP) as described in § 410.75
Nurse-midwives as described in § 410.77
Clinical nurse specialists (CNS) as described in § 410.76
Clinical psychologists (CP) as described in § 410.71
Clinical social workers (CSW) as described in § 410.73
Registered dieticians or nutrition professionals as described in § 410.134
CPs and CSWs cannot bill for psychotherapy services that include medical services or medical evaluation and management services under Medicare. These practitioners may not bill or receive payment for Current Procedural Terminology (CPT) codes 90792, 90833, 90836, and 90838.
The physician visits required under § 483.40(c) for care provided in long term care facilities may not be furnished as tele-medicine services.
5.0 Eligible Medicare Telemedicine Services
The use of a telecommunications system may substitute for a face-to-face, “hands on” encounter for consultation, office visits, individual psychotherapy, and pharmacologic management. These services and corresponding current procedure terminology (CPT) codes include:
Consultations (CPT codes 99241–99245)
Office or other outpatient visits, new patients (CPT codes 99201–99205)
Office or other outpatient visits, established patients (CPT codes 99211–99215)
Individual psychotherapy (CPT codes 90832–90838)
Pharmacologic management (CPT code 90863)
In general, covered Medicare telemedicine services include:
Telemedicine consultations, emergency department or initial patient
Office or other outpatient visits
Subsequent hospital care services, with the limitation of 1 telemedicine visit every 3 days
Subsequent nursing facility care services, with the limitation of 1 telemedicine visit every 3 days
Subsequent nursing facility care services, with the limitation of 1 telemedicine visit every 30 days
Individual and group health and behavior assessment and intervention
Individual psychotherapy
Telemedicine pharmacologic management
Psychiatric diagnostic interview examination
Individual and group medical nutrition therapy
Neurobehavioral status examination
Smoking cessation services
Alcohol and/or substance (other than tobacco) abuse structured assessment and intervention services
Annual alcohol misuse screening, 15 minutes
Transitional care management services with moderate medical decision complexity (face-to-face visit within 7 days of discharge)
6.0 Billing Medicare for Professional Services via Telemedicine
Conditions for payment: As a condition of payment, an interactive audio and video telecommunications system must be used that permits real-time communication between the “provider” at the distant site and the “beneficiary” (i.e., patient) at the originating site. The patient must be present and participating in the telemedicine visit. The medical examination of the patient is under the control of the physician or practitioner at the distant site. A patient presenter is not required to present the beneficiary to physician or practitioner at the distant site unless medically necessary. The decision of medical necessity will be made by the physician or practitioner located at the distant site.
7.0 Exception to the Interactive Telecommunications Requirement
Medicare payment is permitted for telemedicine when asynchronous “store and forward technology,” in single or multimedia formats, is used as a substitute for an interactive telecommunications system only in the case of Federal tele-medicine demonstration programs conducted in Alaska or Hawaii. The originating site and distant site practitioner must be included within the definition of the demonstration program.
Asynchronous “store and forward” technology refers to the transmission of a patient's medical information from an originating site to the physician or practitioner at the distant site to be viewed later by the provider, without the patient being present. This may include, but is not limited to video clips, still images, x-rays, MRIs, EKGs and EEGs, laboratory results, audio clips, and text. The physician or practitioner at the distant site reviews the case without the patient being present. Store and forward substitutes for an interactive encounter with the patient present; the patient is not present in real-time. Asynchronous telecommunications system in single media format does NOT include telephone calls and images transmitted via fax, text messages, or email (without real-time visualization of the patient).
Submitting Claims: Claims are billed to the Medicare Administrative Contractor (MAC) for covered telemedicine services. Claims for telemedicine services should be submitted using the CPT or HCPCS code for the appropriate professional service along with the telemedicine modifier GT, “via interactive audio and video telecommunications systems” (for example, 99201 GT). Coding and billing the GT modifier with a covered telemedicine procedure code certifies that the beneficiary was present at an eligible originating site when the tele-medicine service was furnished.
For Federal telemedicine demonstration programs conducted in Alaska or Hawaii, claims should be submitted using the appropriate CPT or HCPCS code for the professional service along with the telemedicine modifier GQ if telemedicine services were performed “via an asynchronous telecommunications system” (for example, 99201 GQ). By using the GQ modifier, you are certifying that the asynchronous medical file was collected and transmitted to you at the distant site from a Federal telemedicine demonstration project conducted in Alaska or Hawaii.
Payments: Medicare pays the distant site provider the appropriate amount under the Medicare Physician Fee Schedule (PFS) for telemedicine services. If part of a CAH and billing rights have been reassigned to the CAH that has elected the Optional Payment Method, the CAH bills the MAC for tele-medicine services and the payment amount is 80% of the Medicare PFS for telemedicine services.
Originating site facility fee is a separately billable Part B payment and should also be billed to the MAC. Originating sites are paid an originating site facility fee for telemedicine services as described by HCPCS code Q3014.
When a CMHC serves as an originating site, the originating site facility fee does not count toward the number of services used to determine payment for partial hospitalization services.
8.0 Telemedicine for the Medicaid Patient
The federal Medicaid statute does not recognize telemedicine as a distinctive service, but it does recognize telemedicine as a potentially cost-effective option for providing medical care. CMS permits reimbursement for telemedicine services provided to the Medicaid beneficiary under the following guidelines:
Technology—Electronic system requires the ability to conduct interactive audio and video communication.
Provider and Facilities—All providers should practice within their scope of practice as defined in the practice acts that vary state by state. Some states require providers across state lines to have a valid state license where the patient is located.
Reimbursement criteria are determined on a state-by-state basis which includes the following considerations:
Whether to provide reimbursement (At this time, most states will provide reimbursement except for Idaho, Massachusetts, New Hampshire, New Jersey, Ohio, Rhode Island, and Tennessee).
Where in the state it can be covered.
What types of telemedicine providers may be reimbursed.
How much to reimburse (payments cannot exceed Federal Upper Limits).
A summary of Medicaid coverage can be found at: http://www.ncsl.org/research/health/state-coverage-for-telehealth-services.aspx
Additional information can be found at: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Delivery-Systems/Telemedicine.html
9.0 Specific Considerations for the Sleep Specialist
Many of the CMS reimbursement criteria are relevant to the sleep specialist. Multiple types of sleep medicine providers are eligible to provide telemedicine care including physicians, physician assistants and nurse practitioners, and clinical psychologists. Sleep medicine services eligible for reimbursement include consultations and office follow-up visits, psychotherapy, and medication management. Here are a couple of additional considerations specific to sleep medicine:
Reimbursement for polysomnography (including home sleep apnea testing) interpretation is not limited by the current CMS criteria which limits eligibility of store-and-forward asynchronous telemedicine services to beneficiaries only in Alaska and Hawaii. Sleep studies that are attended can have the actual interpretation performed remotely and reimbursed. However, this requires adherence to usual state and federal guidelines to provide clinical care, such as having an active state license where the sleep study was performed.
Respiratory therapists and sleep technologists are often utilized to provide services such as CPAP fitting and troubleshooting. These services performed via telemedicine are not eligible for reimbursement.
10.0 Summary
As use of telemedicine to provide sleep medicine care continues to grow and evolve, understanding the CMS guidelines for reimbursement is essential to providing telemedicine care to the Medicare patient. CMS continues to expand their eligibility criteria, and the sleep practitioner should regularly seek updates regarding types of services and areas eligible for reimbursement.
REFERENCES
- 1.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the Sleep Heart Health Study. Circulation. 2010;122:352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hossain J, Shapiro C. The prevalence, cost implications, and management of sleep disorders: an overview. Sleep Breath. 2002;6:85–102. doi: 10.1007/s11325-002-0085-1. [DOI] [PubMed] [Google Scholar]
- 4.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10:427–38. doi: 10.1016/j.sleep.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Skaer T, Sclar D. Economic implications of sleep disorders. Pharmacoeconomics. 2010;28:1015–23. doi: 10.2165/11537390-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirch DG, Henderson MK, Dill MJ. Physician workforce projections in an era of health care reform. Ann Rev Med. 2012;63:435–45. doi: 10.1146/annurev-med-050310-134634. [DOI] [PubMed] [Google Scholar]
- 8.Harris S. Physician shortage spreads across specialty lines. Association of Medical Colleges Reporter. 2010. Oct, Available from: https://www.aamc.org/newsroom/reporter/oct10/152090/physician_shortage_spreads_across_specialty_lines.html.
- 9.Towers Watson. Current telemedicine technology could mean big savings. 2014. Aug 11, [cited 2014 August 11]. Available from: http://www.towerswatson.com/en-US/Press/2014/08/current-telemedicine-technology-could-mean-big-savings.
- 10.Wechsler LR, Tsao JW, Levine SR, et al. Teleneurology applications: report of the Telemedicine Work Group of the American Academy of Neurology. Neurology. 2013;80:670–6. doi: 10.1212/WNL.0b013e3182823361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lilly CM, Zubrow MT, Kempner KM, et al. Critical care telemedicine: evolution and state of the art. Crit Care Med. 2014;42:2429–36. doi: 10.1097/CCM.0000000000000539. [DOI] [PubMed] [Google Scholar]
- 12.Parikh R, TouVelle MN, Wang H, Zallek SN. Sleep telemedicine: patient satisfaction and treatment adherence. Telemed J E Health. 2011;17:609–14. doi: 10.1089/tmj.2011.0025. [DOI] [PubMed] [Google Scholar]
- 13.American Telemedicine Association. Core operational guidelines for telehealth services involving provider-patient interactions. 2014. Available from: http://www.americantelemed.org/resources/telemedicine-practice-guidelines/telemedicine-practice-guidelines/core-operational-guidelines-for-telehealth-services-involving-provider-patient-interactions.
- 14.Wilson CF. Report 7 of the council on medical service: coverage and payment for telemedicine. [Last accessed May 2015]. Available from: https://download.ama-assn.org/resources/doc/washington/x-pub/cms-telemedicine-report.pdf.
- 15.Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. the optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188:613–20. doi: 10.1164/rccm.201307-1282ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Family Physicians. Guidelines on the supervision of certified nurse midwives, nurse practitioners and physician assistants. 2008. Available from: http://www.aafp.org/about/policies/all/guidelines-nurses.html.
- 17.Department of Health & Human Services, Centers for Medicare & Medicaid Services. CMS manual system: Pub 100-02 medicare benefit policy, transmittal 169. 2013. Mar 1, [Last accessed May 2015]. Available from: http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R169BP.pdf.
- 18.Gough F, Budhrani S, Cohn E, et al. Practice guidelines for live, on demand primary and urgent care. Telemed J E Health. 2015;21:233–41. doi: 10.1089/tmj.2015.0008. [DOI] [PubMed] [Google Scholar]


