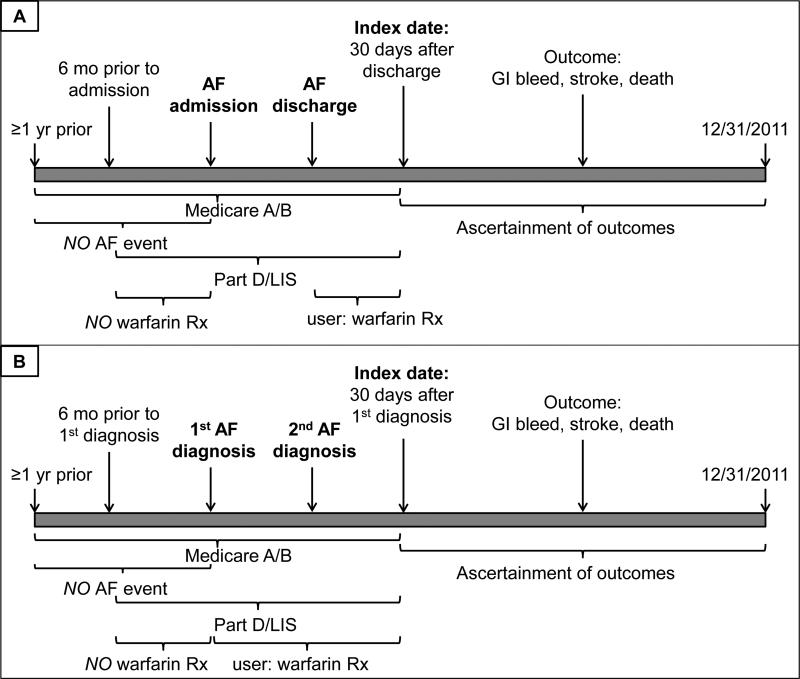
Figure 2.
Timeline of enrollment criteria, ascertainment of exposure, covariates, and outcomes for patients on maintenance hemodialysis newly diagnosed with atrial fibrillation as inpatients (Panel A) or outpatients (Panel B) between 7/1/2007 and 12/1/2011. AF – atrial fibrillation. Patients were required to have continuous Medicare A and B coverage for at least one year prior to either the AF admission or the 1st outpatient AF diagnosis until 30 days after discharge or the 1st outpatient diagnosis. They also were required to have continuous enrollment in a low-income subsidy program of Medicare Part D for at least 6 months prior to admission/1st outpatient diagnosis until 30 days after discharge/1st outpatient diagnosis. Patients with any AF in at least the year prior to admission/1st outpatient diagnosis were excluded, as were patients with any warfarin prescription in the 6 months prior to admission/1st outpatient diagnosis. Patients were considered users if they filled a prescription for warfarin in the 30 days after discharge/1st outpatient diagnosis. Outcomes were ascertained starting 30 days after discharge/1st outpatient diagnosis (index date) until 12/31/2011.