Abstract
Background
To compare risk of carpal tunnel syndrome (CTS) in distal radius fracture (DRF) patients after 7 treatments using bridging external fixation (BrEF), non-bridging external fixation (non-BrEF), plaster fixation, K-wire fixation, dorsal plating fixation, volar plating fixation, and dorsal and volar plating by performing a network meta-analysis.
Material/Methods
An exhaustive search of electronic databases identified randomized controlled trails (RCTs) closely related to our study topic. The published articles were screened, based on predefined inclusion and exclusion criteria, to select high-quality studies for the present network meta-analysis. Data extracted from the selected studies were analyzed using STATA version 12.0 software.
Results
The literature search and selection process identified 12 eligible RCTs that contained a total of 1370 DRF patients (394 patients with BrEF, 377 patients with non-BrEF, 89 patients with K-wire fixation, 192 patients with plaster fixation, 42 patients with dorsal plating fixation, 152 patients with volar plating fixation, and 124 patients with dorsal and volar plating fixation). Our network meta-analysis results demonstrated no significant differences in CTS risk among the 7 treatments (P>0.05). The value of surface under the cumulative ranking curve (SUCRA), however, suggested that dorsal plating fixation is the optimal treatment, with the lowest risk of CTS in DRF patients (dorsal plating fixation: 89.2%; dorsal and volar plating: 57.8%; plaster fixation: 50.9%; non-BrEF: 50.6%; volar plating fixation: 39.6%; BrEF: 38.4%; K-wire fixation: 23.6%).
Conclusions
Our network meta-analysis provides evidence that dorsal plating fixation significantly decreases the risk of CTS and could be the method of choice in DRF patients.
MeSH Keywords: Carpal Tunnel Syndrome, Distal Myopathies, Randomized Controlled Trial
Background
Distal radius fracture (DRF), also called wrist fracture, is the most common fracture of the upper extremities seen in emergency rooms [1]. DRFs are disproportionately high in elderly women over age 60 years and occur at a male-to-female ratio of 1: 4, which is attributed to osteoporosis [2,3]. Carpal tunnel syndrome (CTS) is one of the major complications following DRF and its incidence is between 3.3% and 17.2% [4]. The incidence of CTS in the United States is estimated at 1–3 cases per 1000 subjects per year [5]. CTS symptoms include decreased sensation, numbness and pain in the median nerve region [6]. Interestingly, studies showed that application of local anaesthetics, hematoma caused by injury and surgical trauma are involved in the pathophysiology of CTS risk in DRF patients [7]. Based on recent statistics, a woman over the age of 65 will have at least 1 incident of DRF before end of life. Thus, considering the increased life expectancy in the elderly population due to healthy lifestyles and medical advances, treatment of DRF for full anatomical restoration and complete functional recovery is of utmost importance in this population [8]. However, the optimal treatment strategy for DRF in the elderly is controversial and includes both non-surgical and surgical treatments [9,10]. In recent decades, surgical options for DRF, such as K wires fixation, percutaneous pinning, and volar or dorsal plates, have gained significant popularity [3, 11].
Bridging external fixation (BrEF), used with static fixators, is a popular method to bridge the wrist and stabilize the joint as well as the fracture [12]. On the other hand, non-bridging external fixation (non-BrEF) for DRF treatment is a more generalized technique aimed to restore carpal alignment [13]. Moreover, when the dorsal fragments are twisted 180°, such as in complex DRFs, the dorsally displaced fragments of DRF should be treated directly by fragment specific fixation via the dorsal approach; thus, the low profile dorsal locking plate was developed to address this [14,15]. Plaster fixation and closed reduction have been the more traditional treatments performed in older DRF patients [16]. Volar locked plating is a popular method for treatment in DRF patients due to its rapid stabilization of the fracture and early wrist mobilization [12]. Locked volar plate fixation technique has a lower risk of tendon damage compared to dorsal plates due to the plate coverage by the pronator quadratus muscle [17]. A volar and dorsal plate fixation has the potential to stabilize the displaced fracture and avoid the extensor tendon problems [18]. Although DRFs are among the most common injuries treated by orthopedic, trauma, and hand surgeons, the treatment options are variable and the best approach is a matter of intense debate because prospective randomized studies are inconclusive in their support of any single method [8,17]. In this respect, a meta-analysis is a useful tool to combine evidence from published literature to make more definitive comparisons between treatment choices. In the current study, we analyzed the outcomes and complications for 7 common DRF treatment methods: BrEF, non-BrEF, plaster fixation, K wires fixation, dorsal plating, volar plating and dorsal and volar plating.
Traditional meta-analysis combines results from homogeneous studies on the same topic and it is not feasible to simultaneously compare more than two interventions [19]. In the absence of a direct comparison between treatments, indirect analysis can be used to assess the relative effectiveness of different treatments [20]. A network meta-analysis uses information extracted from published studies and integrates the information to measure relative treatment efficacies [21]. The objective of this network meta-analysis was to assess, using both direct and indirect comparisons, the risk of CTS in DRF patients who underwent these 7 different treatments: BrEF, non-BrEF, plaster fixation, K wires fixation, dorsal plating fixation, volar plating fixation, and dorsal and volar plating fixation.
Material and Methods
Search strategy
Public databases, PubMed and Cochrane Library, were exhaustively searched (last updated search, October 2014) to locate published studies related to CTS and DRF. Keywords used for the literature search were a combination of the following: distal radius fracture, carpal tunnel syndrome, external fixation and internal fixation. The language of publication was restricted to English. Manual search was conducted to identify additional related literature from cross-references.
Inclusion and exclusion criteria
Selection of studies for enrollment into this network meta-analysis was based on the following inclusion criteria: (1) study design: randomized controlled trail (RCT); (2) study subject: clinical or radiological confirmation of DRF patients; (3) outcomes: incidence of CTS in DRF patients; (4) diverse DRF treatment methods. Studies were excluded if they (1) lacked data integrity; (2) were not RCT study design; (3) duplicate literature; (4) complex intervention strategy.
Data extraction
Two independent investigators extracted the required data by using a standard data collection form. The following information was collected: first author, publication year, country, ethnicity, interventions, age, gender and number of research subjects. Discrepancies during study selection or data collection were resolved by discussion with other investigators.
Statistical analysis
STATA 12.0 software (Stata Corp, College Station, TX, USA) with mvmeta command was applied for network meta-analysis. Odds ratio (OR) with 95% confidence interval (95% CI) was calculated by fixed-effects model or random-effects model to evaluate the incidence of CTS in DRF patients following various treatments. Z-test was utilized to evaluate the overall effects size [22]. Cochran’s Q-statistic (P<0.05 was considered significant) and I2 tests were applied to quantify heterogeneity among studies [23,24]. In order to calculate the pooled ORs, fixed-/random-effects models were used. A fixed-effects model was used when significant heterogeneity was observed (P<0.05 or I2>50%), otherwise a random-effects model was employed [25]. Network meta-analysis synthesizes information from a network of related studies comparing more than 2 treatments in DRF patients. If a direct comparison between treatments is absent, a combination of direct evidence and indirect evidence evaluates the direct and indirect comparisons with precision and generates a CTS risk ranking based on the outcomes reported in the included studies. In a closed loop, we employed inconsistency factor (IF) to evaluate heterogeneity among included studies. If the 95% confidence intervals of IF values were truncated at zero, it suggested that the direction of IF was not important [26]. Funnel plots were used to identify the presence of small-study effects and validate the reliability of the results [27]. The assumption of consistency models allows heterogeneity of intervention effects without significant differences in study design. After the generation of a heterogeneity matrix, frequentist statistical approach was used for the fitted model to calculate the ranking probabilities [28]. To rank the treatments, we first used posterior probabilities of outcomes to calculate probabilities of treatment ranking. Next, we used surface under the cumulative ranking probabilities (SUCRA) to identify the best treatment.
Results
The electronic database search and manual search identified a total of 974 articles. After removing duplicate studies (n=231), letters, reviews, meta-analyses (n=18), non-human studies (n=9) and studies irrelevant to DRF (n=165), 551 studies remained for further evaluation. Of these, 529 articles were excluded because they were not RCT or were not relevant to CTS or were not relevant to network, leaving 22 articles for further consideration After the exclusion of 6 studies without data and 4 studies with incomplete or weakly correlated data, only 12 trials met our stringent requirements and were finally included in this network meta-analysis. These 12 studies contained the required data related to 1370 DRF patients (394 patients with bridging external fixation; 377 patients with non-bridging external fixation; 89 patients with K-wire fixation; 192 patients with plaster fixation; 42 patients with dorsal plating fixation; 152 patients with volar plating fixation; 124 patients with dorsal and volar plating fixation). Dual-arm tests were presented in each study, with a total of 12 comparisons of the different treatment strategies [8,12,13,17,29–36]. The baseline characteristics of the included studies are presented in Table 1.
Table 1.
Baseline characteristics of included studies.
| First author | Year | Country | Treatments | Total | Number | Gender (M/F) | Age (years) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | A | B | A | B | A | B | ||||
| McQueen MM [34] | 1996 | UK | Plaster | BrEF | 60 | 30 | 30 | 2/28 | 4/26 | 64±14.5 | 63±11.6 |
| Westphal T [36] | 2005 | Germany | Plaster | DV | 131 | 77 | 54 | 31/46 | 26/28 | 60.6±15.3 | 59.5±15.8 |
| Atroshi I [31] | 2006 | Sweden | non-BrEF | BrEF | 38 | 19 | 19 | 3/16 | 4/15 | 70 (55–86) | 71 (57–84) |
| Hayes AJ [13] | 2008 | Canada | non-BrEF | BrEF | 588 | 358 | 230 | 47/311 | 71/159 | 64 | 58 |
| Leung F [33] | 2008 | Taiwan | K-wire | DV | 144 | 74 | 70 | 85/52 | 42 (17–60) | ||
| Abramo A [29] | 2009 | Sweden | Dorsal | BrEF | 50 | 26 | 24 | 14/36 | 48 (20–65) | ||
| Arora R [8] | 2009 | Australia | Plaster | Volar | 114 | 61 | 53 | 19/42 | 17/36 | 80.9±5.7 | 75.9±4.8 |
| Schmelzer-Schmied N [35] | 2009 | Germany | K-wire | Volar | 30 | 15 | 15 | NR | 60 (50–70) | ||
| Aktekin CN [30] | 2010 | Turkey | Plaster | BrEF | 46 | 24 | 22 | 5/19 | 9/13 | 71.2±5.2 | 69.8±4.5 |
| Chappuis J [17] | 2011 | Belgium | Dorsal | Volar | 31 | 16 | 15 | 2/14 | 2/13 | 71.69±11.2 | 71.73±13.6 |
| Wilcke MK [12] | 2011 | Sweden | Volar | BrEF | 63 | 33 | 30 | 30/25 | 33/23 | 55 (20–69) | 56 (21–69) |
| Jeudy J [32] | 2012 | France | Volar | BrEF | 75 | 36 | 39 | 10/26 | 8/31 | 64.7±3.7 | 64.6±3.5 |
M – male; F – female; NR – not reported; Plaster – plaster fixation; BrEF – bridging external fixation; non-BrEF – non-bridging external fixation; dorsal – dorsal plating fixation; volar – volar plating fixation; DV – dorsal and volar plating fixation; K-wire – K-wire fixation.
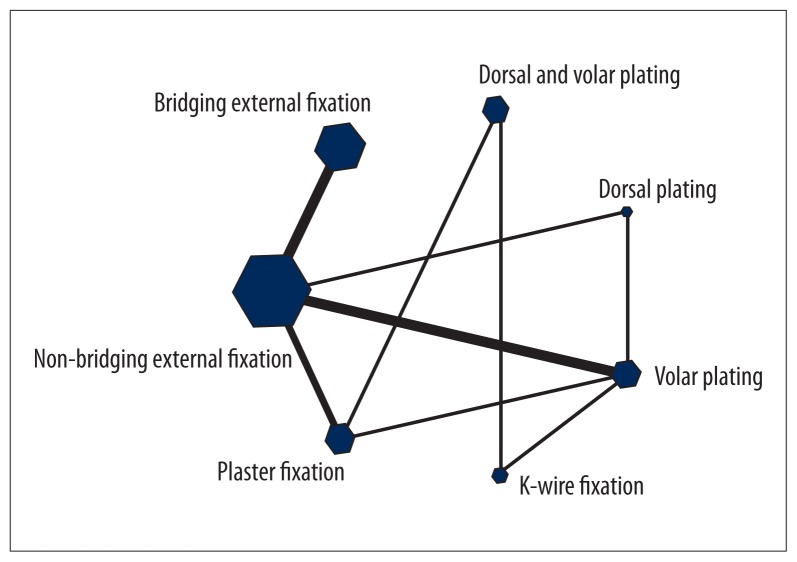
Evidence network
As shown in Figure 1, the connecting lines show direct comparisons between the two connected interventions and pairs of interventions without direct connection can be indirectly compared through network meta-analysis. The width of the lines indicates the number of trails. The size of nodes corresponds to the overall sample size of intervention. The color of lines represents the risk of bias of enrolled trails. This study included 7 treatments for DRF (BrEF; non-BrEF; K-wire fixation; plaster fixation; dorsal plating fixation; volar plating fixation; dorsal and volar plating fixation).
Figure 1.
Networks of evidence of all trials in this network meta-analysis.
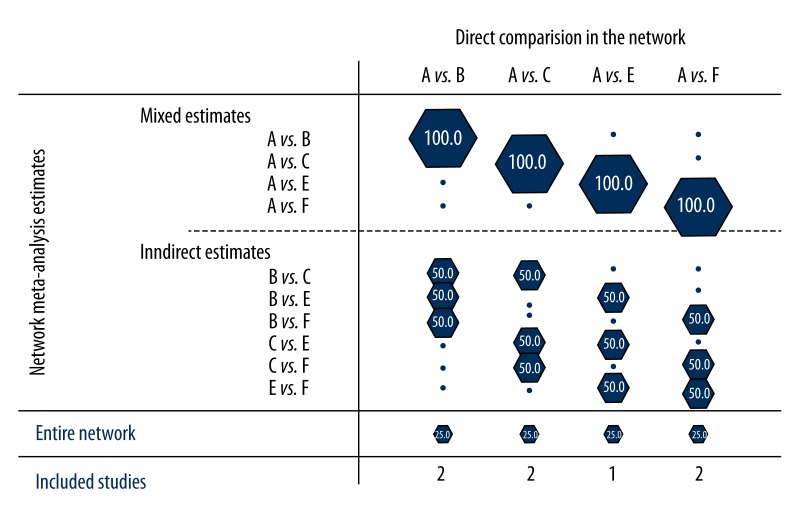
Contribution plot
The contribution of each study to the results of the network meta-analysis are shown in Figure 2: (1) direct comparison between BrEF and non-BrEF were reported in two studies with contributions to the comparisons between non-BrEF and plaster fixation, non-BrEF and dorsal plating fixation, non-BrEF and volar plating fixation at 50%, 50%, and 50%, respectively, and 20% for the whole network meta-analysis; (2) 2 studies investigated the comparisons between BrEF and plaster fixation and their contributions to the comparisons between non-BrEF and plaster fixation, plaster fixation and dorsal plating fixation, plaster fixation and volar plating fixation were 50%, 50%, and 50%, respectively, with 20% contribution to whole network meta-analysis; (3) one study compared BrEF and dorsal plating fixation and the contributions for non-BrEF and dorsal plating fixation, plaster fixation and dorsal plating fixation, dorsal plating fixation and volar plating fixation were 50%, 50%, and 50%, respectively, with 20% contribution to the whole network meta-analysis; (4) 2 studies reported the direct comparison between BrEF and volar plating fixation and the contribution to the comparisons between non-BrEF and volar plating fixation, plaster fixation and volar plating fixation, dorsal plating fixation and volar plating fixation were 50%, 50%, and 50%, respectively, and 20% to the whole network meta-analysis.
Figure 2.
Contribution plot of included studies in this network meta-analysis (A – bridging external fixation; B – non-bridging external fixation; C – plaster fixation; D – K-wire fixation; E – dorsal plating fixation; F – volar plating fixation; G – dorsal and volar plating fixation).
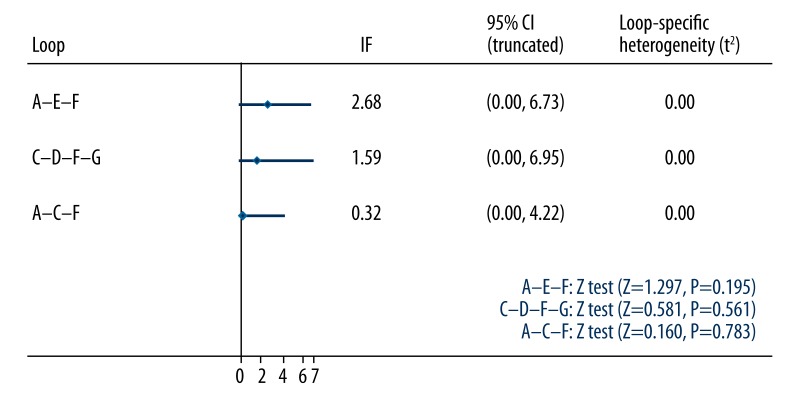
Evaluating and presenting assumptions of network meta-analysis
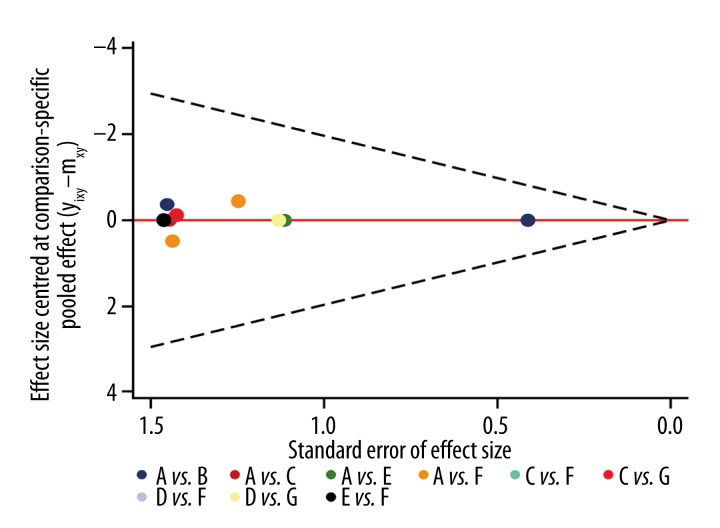
Inconsistency plot was used to identify heterogeneity among studies in the closed loops of this network meta-analysis (Figure 3). Two triangular loops and 1 quadrangle loop were present in the network meta-analysis, including BrEF-dorsal plating fixation-volar plating fixation loop, BrEF-plaster fixation-volar plating fixation loop and plaster fixation- K-wire fixation- volar plating fixation-dorsal and volar plating fixation loop. IF values with 95%CI were truncated at zero, suggesting no significant inconsistency. The P values of greater than 0.05 further confirmed that direct comparisons and indirect comparisons of the 7 treatment strategies showed consistency.
Figure 3.
Inconsistency test for direct and indirect comparison (A – bridging external fixation; B – non-bridging external fixation; C – plaster fixation; D – K-wire fixation; E – dorsal plating fixation; F – volar plating fixation; G – dorsal and volar plating fixation).
Comparisons of the risk of CTS
The present network meta-analysis revealed no statistically significant differences in the risk of CTS in DRF patients who underwent non-BrEF, K-wire fixation, plaster fixation, dorsal plating fixation, volar plating fixation, dorsal and volar plating fixation when compared with BrEF, (non-BrEF: OR=0.823, 95%CI=0.378~1.790, P=0.623; plaster fixation: OR=0.788, 95%CI=0.171~3.633, P=0.760; K-wire fixation: OR=1.809, 95%CI=0.142~23.057, P=0.648; dorsal plating fixation: OR=0.224, 95%CI=0.036~1.377, P=0.106; volar plating fixation: OR=1.012, 95%CI=0.239~4.271, P=0.987; dorsal and volar plating fixation: OR=0.649, 95%CI=0.512~8.240, P=0.739). After ignoring covariance, further analysis suggests no significant differences among the results (all P>0.05) (Table 2).
Table 2.
Comparisons of the carpal tunnel syndrome risk among seven treatments in distal radius fracture patients.
| Non-BrEF vs. BrEF | Plaster vs. BrEF | K-wire vs. BrEF | Dorsal vs. BrEF | Volar vs. BrEF | DV vs. BrEF | |||
|---|---|---|---|---|---|---|---|---|
| CTS (correlation not ignored) | OR | 0.823 | 0.788 | 1.809 | 0.224 | 1.012 | 0.649 | |
| 95%CI | UL | 1.790 | 3.633 | 23.057 | 1.377 | 4.271 | 8.240 | |
| LL | 0.378 | 0.171 | 0.142 | 0.036 | 0.239 | 0.512 | ||
| Z | −0.49 | −0.31 | 0.46 | −1.61 | 0.02 | −0.33 | ||
| CTS (correlation ignored) | OR | 0.823 | 0.946 | 5.315 | 0.097 | 1.514 | 1.351 | |
| 95%CI | UL | 1.790 | 5.716 | 287.472 | 0.863 | 9.589 | 37.378 | |
| LL | 0.378 | 0.157 | 0.098 | 0.011 | 0.239 | 0.049 | ||
| Z | −0.49 | −0.06 | 0.82 | −2.09 | 0.44 | 0.18 |
CTS – Carpal tunnel syndrome; OR – odds ratio; 95%CI – 95% confidential intervals; non-BrEF – non-bridging external fixation; BrEF – bridging external fixation; plaster – plaster fixation; K-wire – K-wire fixation; dorsal – dorsal plating fixation; volar – volar plating fixation; DV – dorsal and volar plating fixation.
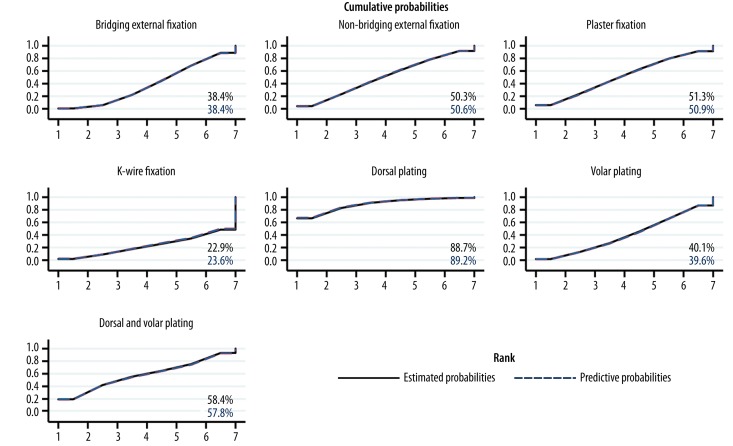
Ranking of interventions
The relative ranking of estimated probabilities for 7 different treatments for CTS risk in DRF patients were 38.4% for BrEF, 50.3% for non-BrEF, 51.3% for plaster fixation, 22.9% for K-wire fixation, 88.7% for dorsal plating fixation, 40.1% for volar plating fixation and 58.4% for dorsal and volar plating fixation, indicating that dorsal plating fixation has the highest treatment relative ranking of estimated probabilities. The cumulative probability ranking of treatments is shown in Figure 4. The SUCRA values for treatment relative ranking of predictive probabilities of the 7 treatments were 38.4% for BrEF, 50.6% for non-BrEF, 50.9% for plaster fixation, 23.6% for K-wire fixation, 89.2% for dorsal plating fixation, 39.6% for volar plating fixation, and 57.8% for dorsal and volar plating fixation, with dorsal plating fixation as the highest treatment relative ranking of predictive probabilities. Thus, DRF patients with dorsal plating fixation showed the lowest CTS risk and dorsal plating fixation was found to be the optimal method to treat DRF in this pooled group of patients.
Figure 4.
Surface under the cumulative ranking curves of treatment relative ranking of predictive probabilities for comparisons of the carpal tunnel syndrome risk among 7 treatments in distal radius fracture.
Assessment of publication bias
Figure 5 shows the funnel plot for the 7 different treatments network, which indicates the presence of small-size effect. All included studies were symmetrically distribute around the vertical line (x=0), suggesting no evidence of publication bias caused by small-size effect in the network.
Figure 5.
Publications bias assessment for included studies (A – bridging external fixation; B – non-bridging external fixation; C – plaster fixation; D – K-wire fixation; E – dorsal plating fixation; F – volar plating fixation; G – dorsal and volar plating fixation)
Discussion
In this study, we performed a systematic network meta-analysis of 7 most common DRF treatments and their associated risks for CTS. The primary aim was to provide a focus for future research to design better DRF treatment strategies for optimal outcomes. Our network meta-analysis consisted of 1370 DRF patients pooled from 12 RCTs that reported the risk of CTS in DRF patients. Network meta-analyses have several advantages: they can directly or indirectly compare more than two treatments simultaneously; provide risk estimates for all treatment comparisons, even for those that were not directly compared in head-to-head trials; predict the best treatment based on probability; and reduce the uncertainty in the risk estimates. Interestingly, the difference in CTS risk in DRF patients following 7 different treatments was not statistically significant.
Indirect comparisons from our network meta-analysis suggested that dorsal plating fixation showed the highest SUCRA values, implying that dorsal plating fixation is the best approach to reduce risk of CTS, among the 7 common DRF treatments. Compared with other surgical interventions, the dorsal double-plating technique has shown promising results in DRF treatment [37]. Dorsal locking plates have the advantage of acting as a buttress to posterior comminution and the locking plates may also allow increased periosteal blood supply [38]. Dorsal plating fixation is an accepted treatment for unstable, dorsally displaced DRFs with many benefits, including the ease of exposure, visualization of the articular surface, and biomechanical advantage of plate placement as a dorsal buttress [39]. Previous studies showed that dorsal locking plating was associated with extensor tendon complications, consequently volar locking plating gained more acceptance. However, this is still controversial and is contradicted by another study that showed comparable complication rates between volar and dorsal plating compared to dorsal plating with a low-profile titanium plate [40,41]. The volar plating approach was believed to decrease the complication of tendon rupture, but not the irritation and rupture of the flexor and extensor tendon [3,18]. Consistent with the result in our network meta-analysis, a previous study showed no significant difference between locked volar plating and BrEF, both in terms of maintaining the radial length and in terms of restoration of the articular profile [32]. Our results also revealed that plaster fixation showed the second-lowest rate of complications, in accordance with a previous study that demonstrated plaster fixation had the lowest complication rate, whereas volar locking plating was associated with significantly increased complications requiring additional surgical interventions [3].
One of the main strengths of this network meta-analysis is the simultaneous comparison of a wide range of treatment strategies for DRF in a single study. Second, all the studies were selected based on a rigorous and extensive literature search aimed at identifying and including all relevant RCTs in this network meta-analysis. Third, all RCTs were homogeneous in study design. Any existing differences in key characteristics across trials, which may act as effect modifiers possibly causing bias in the analysis, appear to be small. However, the strengths of this network meta-analysis should be weighed against its inherent limitations. First, the limited number of trials and the absence of head-to-head comparisons increase the uncertainty of our conclusions. Second, the maintenance trials included in our study could bias the results due to incomplete outcome data. Third, only 12 RCTs were eligible for inclusion in this study. Due to the limited sample size, our network meta-analysis results may be somewhat weak and most data could only be estimated with moderate confidence.
Conclusions
In summary, our network meta-analysis provides convincing evidence that dorsal plating fixation is the best approach for DRF treatment, with the lowest risk of CTS, compared to BrEF, non-BrEF, plaster fixation, K-wire fixation, dorsal and volar plating fixation, and volar plating fixation. However, our conclusions will need to be confirmed using better-designed randomized trials with larger sample sizes to provide the necessary strength of evidence for clinical applications.
Footnotes
Conflicts of interest
None of the authors have any conflict of interest with regard to this research.
Source of support: Departmental sources
References
- 1.Christen D, Melton LJ, III, Zwahlen A, et al. Improved fracture risk assessment based on nonlinear micro-finite element simulations from HRpQCT images at the distal radius. J Bone Miner Res. 2013;28:2601–8. doi: 10.1002/jbmr.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karagiannopoulos C, Sitler M, Michlovitz S, Tierney R. A descriptive study on wrist and hand sensori-motor impairment and function following distal radius fracture intervention. J Hand Ther. 2013;26:204–14. doi: 10.1016/j.jht.2013.03.004. quiz 15. [DOI] [PubMed] [Google Scholar]
- 3.Diaz-Garcia RJ, Oda T, Shauver MJ, Chung KC. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am. 2011;36:824–35e2. doi: 10.1016/j.jhsa.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Itsubo T, Hayashi M, Uchiyama S, et al. Differential onset patterns and causes of carpal tunnel syndrome after distal radius fracture: a retrospective study of 105 wrists. J Orthop Sci. 2010;15:518–23. doi: 10.1007/s00776-010-1496-7. [DOI] [PubMed] [Google Scholar]
- 5.Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91:2478–79. doi: 10.2106/JBJS.I.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hiltunen J, Kirveskari E, Numminen J, et al. Pre- and post-operative diffusion tensor imaging of the median nerve in carpal tunnel syndrome. Eur Radiol. 2012;22:1310–19. doi: 10.1007/s00330-012-2381-x. [DOI] [PubMed] [Google Scholar]
- 7.Ho AW, Ho ST, Koo SC, Wong KH. Hand numbness and carpal tunnel syndrome after volar plating of distal radius fracture. Hand (NY) 2011;6:34–38. doi: 10.1007/s11552-010-9283-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arora R, Gabl M, Gschwentner M, et al. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23:237–42. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 9.Bartl C, Stengel D, Bruckner T, et al. Open reduction and internal fixation versus casting for highly comminuted and intra-articular fractures of the distal radius (ORCHID): protocol for a randomized clinical multi-center trial. Trials. 2011;12:84. doi: 10.1186/1745-6215-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matschke S, Marent-Huber M, et al. The surgical treatment of unstable distal radius fractures by angle stable implants: a multicenter prospective study. J Orthop Trauma. 2011;25:312–17. doi: 10.1097/BOT.0b013e3181f2b09e. [DOI] [PubMed] [Google Scholar]
- 11.Arora R, Lutz M, Deml C, et al. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93:2146–53. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 12.Wilcke MK, Abbaszadegan H, Adolphson PY. Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year. Acta Orthop. 2011;82:76–81. doi: 10.3109/17453674.2011.552781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayes AJ, Duffy PJ, McQueen MM. Bridging and non-bridging external fixation in the treatment of unstable fractures of the distal radius: a retrospective study of 588 patients. Acta Orthop. 2008;79:540–47. doi: 10.1080/17453670710015553. [DOI] [PubMed] [Google Scholar]
- 14.Blythe M, Stoffel K, Jarrett P, Kuster M. Volar versus dorsal locking plates with and without radial styloid locking plates for the fixation of dorsally comminuted distal radius fractures: A biomechanical study in cadavers. J Hand Surg Am. 2006;31:1587–93. doi: 10.1016/j.jhsa.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Chou YC, Chen AC, Chen CY, et al. Dorsal and volar 2.4-mm titanium locking plate fixation for AO type C3 dorsally comminuted distal radius fractures. J Hand Surg Am. 2011;36:974–81. doi: 10.1016/j.jhsa.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 16.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–73. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chappuis J, Boute P, Putz P. Dorsally displaced extra-articular distal radius fractures fixation: Dorsal IM nailing versus volar plating. A randomized controlled trial. Orthop Traumatol Surg Res. 2011;97:471–78. doi: 10.1016/j.otsr.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Soong M, van Leerdam R, Guitton TG, et al. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011;36:3–9. doi: 10.1016/j.jhsa.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 19.Peruzzi M, De Luca L, Thomsen HS, et al. A network meta-analysis on randomized trials focusing on the preventive effect of statins on contrast-induced nephropathy. Biomed Res Int. 2014;2014:213239. doi: 10.1155/2014/213239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hadjigeorgiou GM, Doxani C, Miligkos M, et al. A network meta-analysis of randomized controlled trials for comparing the effectiveness and safety profile of treatments with marketing authorization for relapsing multiple sclerosis. J Clin Pharm Ther. 2013;38:433–39. doi: 10.1111/jcpt.12090. [DOI] [PubMed] [Google Scholar]
- 21.Numthavaj P, Thakkinstian A, Dejthevaporn C, Attia J. Corticosteroid and antiviral therapy for Bell’s palsy: a network meta-analysis. BMC Neurol. 2011;11:1. doi: 10.1186/1471-2377-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen H, Manning AK, Dupuis J. A method of moments estimator for random effect multivariate meta-analysis. Biometrics. 2012;68:1278–84. doi: 10.1111/j.1541-0420.2012.01761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson D, White IR, Riley RD. Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat Med. 2012;31:3805–20. doi: 10.1002/sim.5453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peters JL, Sutton AJ, Jones DR, et al. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295:676–80. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 25.Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2005;28:123–37. doi: 10.1002/gepi.20048. [DOI] [PubMed] [Google Scholar]
- 26.Song F, Altman DG, Glenny AM, Deeks JJ. Validity of indirect comparison for estimating efficacy of competing interventions: empirical evidence from published meta-analyses. BMJ. 2003;326:472. doi: 10.1136/bmj.326.7387.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White IR, Barrett JK, Jackson D, Higgins J. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Research Synthesis Methods. 2012;3:111–25. doi: 10.1002/jrsm.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abramo A, Kopylov P, Geijer M, Tagil M. Open reduction and internal fixation compared to closed reduction and external fixation in distal radial fractures: a randomized study of 50 patients. Acta Orthop. 2009;80:478–85. doi: 10.3109/17453670903171875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aktekin CN, Altay M, Gursoy Z, et al. Comparison between external fixation and cast treatment in the management of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 2010;35:736–42. doi: 10.1016/j.jhsa.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 31.Atroshi I, Brogren E, Larsson GU, et al. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77:445–53. doi: 10.1080/17453670610046389. [DOI] [PubMed] [Google Scholar]
- 32.Jeudy J, Steiger V, Boyer P, et al. Treatment of complex fractures of the distal radius: a prospective randomised comparison of external fixation ‘versus’ locked volar plating. Injury. 2012;43:174–79. doi: 10.1016/j.injury.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 33.Leung F, Tu YK, Chew WY, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures. A randomized study. J Bone Joint Surg Am. 2008;90:16–22. doi: 10.2106/JBJS.F.01581. [DOI] [PubMed] [Google Scholar]
- 34.McQueen MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 1996;78:404–9. [PubMed] [Google Scholar]
- 35.Schmelzer-Schmied N, Wieloch P, Martini AK, Daecke W. Comparison of external fixation, locking and non-locking palmar plating for unstable distal radius fractures in the elderly. Int Orthop. 2009;33:773–78. doi: 10.1007/s00264-007-0504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Westphal T, Piatek S, Schubert S, Winckler S. Outcome after surgery of distal radius fractures: no differences between external fixation and ORIF. Arch Orthop Trauma Surg. 2005;125:507–14. doi: 10.1007/s00402-005-0023-3. [DOI] [PubMed] [Google Scholar]
- 37.Chen AC, Lin YH, Kuo HN, et al. Design optimisation and experimental evaluation of dorsal double plating fixation for distal radius fracture. Injury. 2013;44:527–34. doi: 10.1016/j.injury.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 38.Florin M, Arzdorf M, Linke B, Auer JA. Assessment of stiffness and strength of 4 different implants available for equine fracture treatment: a study on a 20 degrees oblique long-bone fracture model using a bone substitute. Vet Surg. 2005;34:231–38. doi: 10.1111/j.1532.950X.2005.00035.x. [DOI] [PubMed] [Google Scholar]
- 39.Matzon JL, Kenniston J, Beredjiklian PK. Hardware-related complications after dorsal plating for displaced distal radius fractures. Orthopedics. 2014;37:e978–82. doi: 10.3928/01477447-20141023-54. [DOI] [PubMed] [Google Scholar]
- 40.Yu YR, Makhni MC, Tabrizi S, et al. Complications of low-profile dorsal versus volar locking plates in the distal radius: a comparative study. J Hand Surg Am. 2011;36:1135–41. doi: 10.1016/j.jhsa.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 41.Jupiter JB, Marent-Huber M, Group LCPS. Operative management of distal radial fractures with 2.4-millimeter locking plates: a multicenter prospective case series. Surgical technique. J Bone Joint Surg Am. 2010;92(Suppl 1 Pt 1):96–106. doi: 10.2106/JBJS.I.01340. [DOI] [PubMed] [Google Scholar]