Abstract
Objectives
Childhood abuse is associated with increased risks of adult psychiatric disorders and physical health conditions. Accumulating evidence documents associations of childhood abuse with sleep disturbances in adulthood. However, to date, no study has evaluated associations of childhood abuse and sleep disturbances among pregnant women.
Methods
This cross-sectional study included 634 pregnant Peruvian women. In-person interviews were conducted in early pregnancy to collect information regarding socio-demographic characteristics, history of childhood abuse, and complaints of sleep disturbances. Spanish language version of the Ford Insomnia Response to Stress Test (FIRST-S) and the Pittsburgh Sleep Quality Index (PSQI-S) were used to assess stress-related sleep disturbance and sleep quality, respectively. Logistic regression was used to estimate adjusted odds ratios (aOR) and 95% confidence intervals (95% CIs).
Results
Women who experienced any childhood abuse had a 1.65-fold increased odds of stress-related sleep disturbance (aOR=1.65; 95% CI: 1.15–2.38) and 2.11-fold increased odds of poor sleep quality during early pregnancy (aOR=2.11; 95% CI: 1.35–3.30) as compared with women who reported no abuse. Compared with women who reported no childhood abuse, those who reported both physical and sexual abuse during childhood were more than twice as likely to suffer from stress-related sleep disturbance (aOR=2.26; 95% CI:1.44–3.53) and poor sleep quality (aOR=2.43; 95% CI:1.45–4.09).
Conclusions
A history of childhood abuse is associated with increased odds of stress-related sleep disturbance and poor sleep quality during pregnancy. These findings, if replicated, should be used to inform the development of trauma-informed care for such sleep disturbances induced by childhood trauma.
Keywords: childhood abuse, sleep disturbance, pregnancy, stress, life course
BACKGROUND
Pregnancy is a period characterized by multiple physiologic changes, including variations in energy and sleep demands, often leading to sleep disturbances.1 Available evidence suggests that sleep disturbances during pregnancy are associated with adverse perinatal outcomes, including maternal depression, preeclampsia, and preterm birth.2–4 For example, investigators have reported that short sleep duration (6 or fewer nightly hours) in early pregnancy is associated with elevated trimester-specific blood pressures, 3 increased risks of preeclampsia 3 and spontaneous preterm birth.4 Given the adverse maternal and perinatal health outcomes associated with disturbed sleep during pregnancy, it is important to identify factors associated with disturbed sleep that may serve as clinically useful screening indicators for poor sleep health.
Evidence from studies conducted during the past two decades suggest that exposure to childhood abuse is associated with an increased risk of sleep disorders in adulthood.5 As many as 27 studies have documented statistically significant associations of sleep disorders with a history of childhood adversity, which includes physical, sexual, or emotional abuse, and physical or emotional neglect.5 Many studies have measured sleep disturbances using the Pittsburgh Sleep Quality Index (PSQI), a widely used self-assessment of sleep quality and disturbances, in which higher scores indicate poor sleep quality.6 Notably, results from some studies suggest that women with childhood histories of sexual, physical and emotional abuse are more likely to experience poor sleep quality (PSQI>5) when compared with women without an abuse history7. Furthermore, there is evidence to suggest that the association between childhood abuse and sleep disturbances is stronger among women than men, though this is inconclusive.5, 8, 9
Despite the evident association between childhood abuse and sleep disorders among adult women and the perinatal risks associated with sleep disorders during pregnancy, no studies to date have evaluated the association between childhood abuse and sleep disturbances among pregnant women. To fill this gap in the literature, we examined the extent to which, if at all, women’s early childhood experience of physical and/or sexual abuse is associated with stress-related sleep disturbance or sleep quality during early pregnancy. As a secondary exploratory analysis, we examined whether antepartum depression and exposure to physical and/or sexual abuse as an adult mediate observed associations between childhood abuse and sleep disturbances in pregnancy. An understanding of these relationships is of particular interest among low-income Peruvian women given the high burden of gender-based violence and associated adverse mental and physical health outcomes in this population.10, 11
Study Population
We analyzed data from the Pregnancy Outcomes, Maternal and Infant Study (PrOMIS) Cohort, an ongoing prospective cohort study of pregnant women enrolled in prenatal care clinics at the Instituto Nacional Materno Perinatal (INMP) in Lima, Peru.12 The INMP is one of the primary referral hospitals for maternal and perinatal care in Lima, Peru. The study population for this investigation was drawn from women who had their first prenatal care visit at the INMP between October 2013 and February 2014. Women who initiated prenatal care before 16 weeks gestation, who were 18–49 years of age, and who spoke and understood Spanish were eligible to participate. Written informed consent was obtained from all participants prior to interview. All study personnel were trained on interviewing skills, contents of the questionnaire, and ethical conduct of violence research (including issues of safety and confidentiality). Interviewers were trained to refer participants found to be in physically dangerous situations and/or in immediate need for counseling to psychologists at local women’s organizations, hospital psychiatrists, and battered women’s shelters. The Institutional Review Boards from the INMP and the Human Research Administration Office at the Harvard T.H. Chan School of Public Health approved all procedures used in this study.
Data Collection and Variable Specification
Using a structured questionnaire, participants were interviewed by trained research personnel in a private setting. Information regarding maternal socio-demographic and lifestyle characteristics, medical and reproductive history, childhood abuse, intimate partner violence, and sleep problems was collected. The analytical population for this present study was derived from 652 participants enrolled in the PrOMIS Cohort. For the purposes of the present study 22 participants with missing information on childhood abuse and sleep problems were excluded from analysis. Hence, a total of 630 participants remained for analysis.
Childhood Abuse
We used the Childhood Physical and Sexual Abuse Questionnaire to elicit information concerning participants’ experiences with childhood physical and sexual abuse 13. Participants were categorized as having experienced childhood physical abuse if, before the age of 18 years, they reported that an older person hit, kicked, pushed, or beat them often and/or their life was seriously threatened. Participants were categorized as having experienced childhood sexual abuse if, before the age of 18 years, they reported that an older person touched them, they were made to touch someone else in a sexual way, or someone attempted or completed intercourse with them. Participants who responded “no” to all questions regarding childhood sexual and physical abuse were categorized as “no abuse”. Participants who experienced “any childhood physical or sexual abuse” were further classified into three groups: “childhood physical abuse only” if they only endorsed physical abuse questions, “childhood sexual abuse only” if they only endorsed sexual abuse questions, or “both childhood physical and sexual abuse” if they endorsed both physical abuse and sexual abuse questions. Furthermore the frequency of childhood abuse events was assessed by summing responses to individual abuse questions and creating the following response categories: “0,” “1,” “2,” or “≥3”
Intimate Partner Violence
Questions pertaining to intimate partner violence were adapted from the protocol of Demographic Health Survey Questionnaires and Modules: Domestic Violence Module 14 and the World Health Organization (WHO) Multi-Country Study on Violence Against Women 15. Participants were assessed for several physical and/or sexual coercive acts used against them by a current or former spouse or intimate partner during the 12 months before the index pregnancy. A participant was classified as having experienced physical violence if she endorsed any of the following acts: being slapped or having something thrown at her; being pushed, shoved, or having her hair pulled; being hit; being kicked, dragged, or beaten up; being choked or burnt on purpose; and being threatened or hurt with a weapon (such as a gun or knife). A participant was classified as having experienced sexual violence if she endorsed any of the following acts: being physically forced to have sexual intercourse; having had unwanted sexual intercourse because of fear of what the partner might do; or being forced to perform other sexual acts that she found degrading or humiliating. In the present analysis, we categorized participants as having experienced either “no physical and sexual violence” or “any physical or sexual violence” during the 12 months before the index pregnancy.
Ford Insomnia Response to Stress Test (FIRST)
The FIRST is a standardized questionnaire with high test-retest reliability (0.92) and has been validated as a sensitive measure of vulnerability to sleep disturbance in normal non-insomniac individuals using polysomnographic assessment.16 The FIRST includes nine items designed to query participants about the likelihood of having sleep disruption due to specific stressful situations and more broadly-described periods of stress occurring during the day or evening. The nine situations are: 1) before an important meeting the next day; 2) after a stressful experience during the day; 3) after a stressful experience in the evening; 4) after getting bad news during the day; 5) after watching a frightening movie or television show; 6) after having a bad day at work; 7) after an argument; 8) before having to speak in public; and 9) before going on vacation the next day. Participants were asked to rate how likely it is for them to have difficulty in sleeping when they have recently experienced these stressful situations16. Response categories are “not likely,” “somewhat likely,” “moderately likely,” and “very likely,” scored as 1, 2, 3, and 4, respectively. The total score ranges from 9 to 36. High scores on the FIRST indicate greater vulnerability to stress-related sleep disturbance.17 Consistent with prior studies, we used the median FIRST score (median = 12) to characterize participants according to high and low likelihood of susceptibility to stress-related sleep disturbance.16, 18
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a 19-item, self-rated questionnaire designed to measure sleep quality and disturbance over the past month.6 The PSQI has seven sleep components: sleep duration, disturbance, latency, habitual sleep efficiency, use of sleep medicine, daytime dysfunction due to sleepiness, and overall quality of sleep. Each component produced a score ranging from 0 to 3, where a score of 3 indicates the highest level of dysfunction. The sleep component scores are summed to get a total score ranging from 0 to 21 with the higher total score (referred to as global score) indicating worse sleep quality. Participants with global scores that exceed 5 are classified as poor sleepers.6 Those with a score of 5 or less were classified as good sleepers. This classification system is consistent with prior studies including those conducted in Peru.19
Patient health questionnaire-9 (PHQ-9)
The PHQ-9 was used to evaluate antepartum depression. 20 The PHQ-9 is a 9-item questionnaire with demonstrated reliability and validity for assessing depressive disorders among a diverse group of obstetrics-gynecology patients 21 and in Spanish-speaking women. 22, 23 The PHQ-9 instrument asks respondents to rate the relevancy of each statement comprising emotional, cognitive, and functional somatic symptoms over the past two weeks on a four-point scale never; b) several days; c) more than half the days; or d) nearly every day. The PHQ-9 total score is the sum of scores for the nine items for each woman, and ranged from 0–27. Women were assigned to one of five depressive symptom categories based on total PHQ-9 score, (a) no depressive symptoms (0–4), (b) mild (5–9), (b) moderate (10–14), (c) moderately severe (15–19) and (d) severe (20–27) depressive symptoms. For the purpose of this study, we defined presence of antepartum depression based upon total PHQ-9 score, (a) no depressive symptoms (0–9) and (b) antepartum depression (10–27). 20 A meta-analysis of 14 studies support the use of a PHQ-9 score of ≥10 to classify subjects with major depressive disorder. 24
Other Covariates
Participant age was categorized as follows: 18–19, 20–29, 30–34, and ≥35 years. Other socio-demographic variables were categorized as follows: educational attainment (≤6, 7–12, and >12 completed years of schooling); maternal ethnicity (Mestizo vs. other); marital status (married or living with partner vs. other); employment status (employed vs. not employed); access to basic foods (hard vs. not very hard); parity (nulliparous vs. multiparous); planned pregnancy (yes vs. no); and early pregnancy body mass index (BMI) (<18.5 kg/m2, 18.5–24.9 kg/m2, 25–29.9 kg/m2, and ≥30 kg/m2).
Statistical Analysis
We examined the frequency distribution of maternal socio-demographic characteristics and reproductive history. Based on childhood abuse status, women were classified into four groups: no abuse, physical abuse only, sexual abuse only, and both physical and sexual abuse. Across these four groups, we conducted the Chi-square test for categorical variables and the one-way analysis of variance (ANOVA) for continuous variables to determine whether there were statistically significant differences in the distribution of socio-demographic and reproductive characteristics. We used binary and multinomial logistic regression to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) of stress-related sleep disturbance and sleep quality in the first trimester in relation to the history of childhood abuse. We included potential confounders of a priori interest (i.e., maternal age at interview and maternal ethnicity) in multivariable adjusted logistic regression models on the bases of their hypothesized relationship between exposure (history of childhood abuse) and outcome (sleep disturbances). In addition, we conducted exploratory mediation analysis to assess whether the relation between childhood abuse and sleep disturbances could be partially explained through the indirect effects of the hypothesized mediators, we followed the four steps in establishing mediation recommended by Baron and Kenny.25 We considered antepartum depression and intimate partner violence during the 12 months before the index pregnancy as potential mediators as these variables may be on the causal pathway between childhood abuse and adulthood sleep disturbances. First, we assessed the relation between childhood abuse and sleep disturbances (the direct effect). Second, we evaluated the relation between childhood abuse and the mediators. Third, we examined the relation between the hypothesized mediators and sleep disturbances. Finally, we investigated the extent to which these factors mediated the relation between childhood abuse and sleep disturbances, adjusting for maternal age at interview and maternal ethnicity. The mediation analysis was performed using the binary_mediation command in Stata version 13.0 (StataCorp, College Station, TX, USA) 26–28 All other statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). The level of statistical significance was set at P < 0.05, and all tests were two-sided.
RESULTS
Table 1 shows the socio-demographic and reproductive characteristics of the study population. The mean age of participants was 28.8 years (standard deviation = 6.6 years); the majority of participants were married or living with a partner (79.7%) and had at least seven years of education (95.7%) while half (49.8%) reported that they were employed during pregnancy. Approximately 48% of participants reported having difficulty paying for basics such as food items. The average gestational age of participants at interview was 9.1 weeks (standard deviation = 3.6 weeks) and 46.2% were nulliparous. Nearly half of the participants (50.5%) were overweight or obese (early pregnancy BMI ≥25 kg/m2). Characteristics of the study sample according to childhood abuse groups are also presented in Table 1. Access to basics was statistically significantly associated with maternal history of childhood abuse (P- value <0.0001). The study groups were otherwise similar for all other characteristics.
Table 1.
Socio-demographic and reproductive characteristics of the study population by types of childhood abuse in Lima, Peru (N=630)
| Characteristics | All participants (N=630) |
No abuse (N = 161) |
Physical abuse only (N = 259) |
Sexual abuse only (N = 47) |
Physical and sexual abuse (N = 163) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | P-value | |
| Age (years)* | 28.8 ± 6.6 | 28.8 ± 6.3 | 28.5 ± 6.5 | 27.6 ± 7.0 | 29.6 ± 6.8 | 0.30 | |||||
| Age (years) | |||||||||||
| 18–20 | 19 | 3.0 | 1 | 0.6 | 7 | 2.7 | 4 | 8.5 | 7 | 4.3 | 0.10 |
| 20–29 | 335 | 53.2 | 91 | 56.5 | 143 | 55.2 | 26 | 55.3 | 75 | 46.0 | |
| 30–34 | 141 | 22.4 | 36 | 22.4 | 53 | 20.5 | 7 | 14.9 | 45 | 27.6 | |
| ≥35 | 135 | 21.4 | 33 | 20.5 | 56 | 21.6 | 10 | 21.3 | 36 | 22.1 | |
| Education (years) | |||||||||||
| ≤6 | 26 | 4.1 | 6 | 3.7 | 12 | 4.6 | 1 | 2.1 | 7 | 4.3 | 0.33 |
| 7–12 | 324 | 51.4 | 92 | 57.1 | 137 | 52.9 | 22 | 46.8 | 73 | 44.8 | |
| >12 | 279 | 44.3 | 62 | 38.5 | 110 | 42.5 | 24 | 51.1 | 83 | 50.9 | |
| Mestizo ethnicity | 468 | 74.3 | 118 | 73.3 | 184 | 71.0 | 37 | 78.7 | 129 | 79.1 | 0.26 |
| Married/living with a partner | 502 | 79.7 | 135 | 83.9 | 209 | 80.7 | 35 | 74.5 | 123 | 75.5 | 0.20 |
| Employed | 314 | 49.8 | 87 | 54.0 | 117 | 45.2 | 22 | 46.8 | 88 | 54.0 | 0.20 |
| Access to basic foods | |||||||||||
| Hard | 305 | 48.4 | 55 | 34.2 | 126 | 48.6 | 25 | 53.2 | 99 | 60.7 | <0.0001 |
| Not very hard | 325 | 51.6 | 106 | 65.8 | 133 | 51.4 | 22 | 46.8 | 64 | 39.3 | |
| Nulliparous | 291 | 46.2 | 79 | 49.1 | 114 | 44.0 | 25 | 53.2 | 73 | 44.8 | 0.62 |
| Planned pregnancy | 258 | 41.0 | 70 | 43.5 | 106 | 40.9 | 21 | 44.7 | 61 | 37.4 | 0.70 |
| Gestational age at interview* | 9.1 ± 3.6 | 9.0 ± 3.3 | 9.2 ± 3.5 | 9.1 ± 3.7 | 9.1 ± 3.9 | 0.92 | |||||
| Early pregnancy body mass | |||||||||||
| index (kg/m2) | |||||||||||
| <18.5 | 15 | 2.4 | 2 | 1.2 | 8 | 3.1 | 2 | 4.3 | 3 | 1.8 | 0.68 |
| 18.5–24.9 | 286 | 45.4 | 71 | 44.1 | 112 | 43.2 | 25 | 53.2 | 78 | 47.9 | |
| 25–29.9 | 232 | 36.8 | 58 | 36.0 | 102 | 39.4 | 13 | 27.7 | 59 | 36.2 | |
| ≥30 | 86 | 13.7 | 26 | 16.1 | 36 | 13.9 | 5 | 10.6 | 19 | 11.7 | |
Due to missing data, percentages may not add up to 100%.
mean ± SD (standard deviation); for continuous variables, P-value was calculated using the Kruskal-Wallis test; for categorical variables, P-value was calculated using the Chi-square test.
The association between maternal history of childhood abuse and stress-related sleep disturbance is presented in Table 2. Compared with women reporting no history of childhood abuse, those who experienced any childhood abuse had an increased odds of stress-related sleep disturbance (aOR=1.65; 95% CI: 1.15–2.38). Those who experienced both physical and sexual abuse during childhood had a 2.3-fold increased odds (aOR=2.26; 95% CI: 1.44–3.53) of stress-related sleep disturbance compared with women who reported experiencing no abuse in childhood. Women who experienced physical abuse only as a child had a 1.5-fold increased odds of stress-related sleep disturbance, as compared with those who reported no abuse in childhood, though the association did not reach statistical significance (aOR=1.47; 95% CI: 0.99–2.2). We observed no strong evidence of an association between childhood of sexual abuse only and stress-related sleep disturbance (aOR=1.05; 95% CI: 0.54–2.05).
Table 2.
Association between childhood abuse and stress-related sleep disturbance assessed by the Spanish-language version of the Ford Insomnia Response to Stress Test (FIRST-S) during pregnancy (N=630)
| Low FIRST scores (FIRST ≤ 12) (N = 319) |
High FIRST scores (FIRST > 12) (N = 311) |
||||||
|---|---|---|---|---|---|---|---|
| Childhood abuse | n | % | n | % | Unadjusted OR (95% CI) |
Adjusted OR (95% CI)* |
Adjusted OR (95% CI)** |
| No abuse | 96 | 30.1 | 65 | 20.9 | Reference | Reference | Reference |
| Any abuse | 223 | 69.9 | 246 | 79.1 | 1.63 (1.13, 2.34) | 1.65 (1.15, 2.38) | 1.58 (1.10, 2.29) |
| Types of abuse | |||||||
| No abuse | 96 | 30.1 | 65 | 20.9 | Reference | Reference | Reference |
| Physical abuse only | 130 | 40.8 | 129 | 41.5 | 1.47 (0.98, 2.18) | 1.47 (0.99, 2.20) | 1.46 (0.97, 2.18) |
| Sexual abuse only | 28 | 8.8 | 19 | 6.1 | 1.00 (0.52, 1.94) | 1.05 (0.54, 2.05) | 0.95 (0.48, 1.89) |
| Physical & sexual abuse | 65 | 20.4 | 98 | 31.5 | 2.23 (1.43, 3.47) | 2.26 (1.44, 3.53) | 2.10 (1.33, 3.30) |
Low and high FIRST-S scores were defined based on the median score (12) of the FIRST at interview 1 among this study population.
Abbreviations: OR, odds ratio; CI, confidence interval
Adjusted for maternal age (years) at interview and race (Mestizo vs. other)
Adjusted for maternal age (years) at interview, race (Mestizo vs. other), and intimate partner violence 12 months before pregnancy (any physical abuse or sexual abuse vs. no abuse)
We next assessed maternal history of childhood abuse with odds of poor sleep quality in early pregnancy (Table 3). Women reporting any abuse during childhood had a 2.1-fold increased odds of poor sleep quality during pregnancy as compared with women who reported no childhood abuse (aOR=2.11; 95% CI: 1.35–3.30). With respect to specific types of childhood abuse, physical and sexual abuse (aOR=2.43; 95% CI: 1.45–4.09) and physical abuse only (aOR=1.95; 95% CI: 1.20–3.16) were each found to be statistically significantly associated with poor sleep quality in early pregnancy. The association for sexual abuse only (aOR=1.96; 95% CI: 0.93–4.13), however, did not reach statistical significance.
Table 3.
Association between childhood abuse and sleep quality assessed by the Pittsburgh Sleep Quality Index (PSQI) during pregnancy (N=630)
| Good sleep quality (PSQI ≤ 5) (N = 453) |
Poor sleep quality (PSQI > 5) (N = 177) |
||||||
|---|---|---|---|---|---|---|---|
| Childhood abuse | n | % | n | % | Unadjusted OR (95% CI) |
Adjusted OR (95% CI)* |
Adjusted OR (95% CI)** |
| No abuse | 132 | 29.1 | 29 | 16.4 | Reference | Reference | Reference |
| Any abuse | 321 | 70.9 | 148 | 83.6 | 2.10 (1.34, 3.28) | 2.11 (1.35, 3.30) | 1.98 (1.26, 3.12) |
| Types of abuse | |||||||
| No abuse | 132 | 29.1 | 29 | 16.4 | Reference | Reference | Reference |
| Physical abuse only | 181 | 40.0 | 78 | 44.1 | 1.96 (1.21, 3.18) | 1.95 (1.20, 3.16) | 1.92 (1.18, 3.13) |
| Sexual abuse only | 33 | 7.3 | 14 | 7.9 | 1.93 (0.92, 406) | 1.96 (0.93, 4.13) | 1.69 (0.79, 3.65) |
| Physical & sexual abuse | 107 | 23.6 | 56 | 31.6 | 2.38 (1.42, 3.99) | 2.43 (1.45, 4.09) | 2.18 (1.29, 3.69) |
Abbreviations: OR, odds ratio; CI, confidence interval
Adjusted for maternal age (years) at interview and race (Mestizo vs. other)
Adjusted for maternal age (years) at interview, race (Mestizo vs. other), and intimate partner violence 12 months before pregnancy (any physical abuse or sexual abuse vs. no abuse)
Given that antepartum depression and recent experience of intimate partner violence may be on the causal pathway between childhood abuse and sleep disturbances during pregnancy, we explored the extent to which antepartum depression and recent abuse by an intimate partner (experienced during the 12 months before the pregnancy) are mediators of the association of childhood abuse with sleep disturbance and poor sleep quality in early pregnancy (Figures 1 and 2). From these analyses, we found that antepartum depression accounted for 64% of the indirect effect while intimate partner violence accounted for 17% of the indirect effect of the relation between childhood abuse and stress-related sleep disturbance (Figure 1). Similarly, we found that antepartum depression accounted for 54% of the indirect effect while intimate partner violence accounted for 17% of the indirect effect of the relation between childhood abuse and poor sleep quality (Figure 2).
Figure 1. Relation between childhood abuse, intimate partner violence 12 months prior to pregnancy and stress-related sleep disturbance assessed by the Ford Insomnia Response to Stress Test (FIRST-S) during the first trimester of pregnancy (N=624).
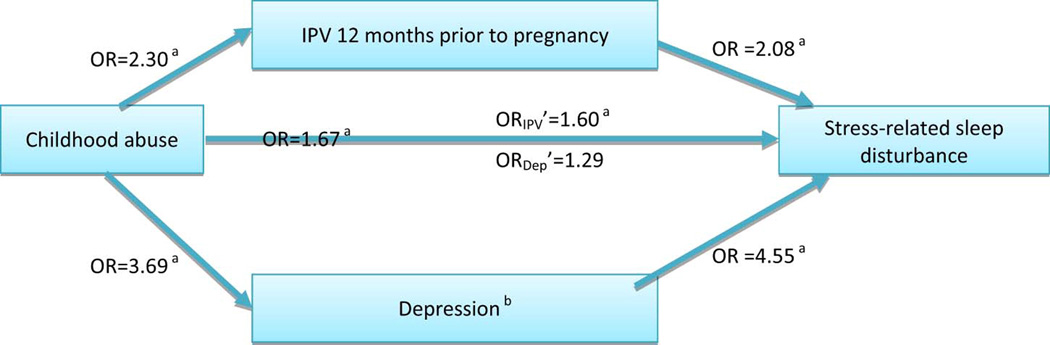
Six women were excluded due to missing information on IPV 12 months prior to pregnancy (n=3) and the PHQ-8 (n=3).
Abbreviation: OR, odds ratio; IPV, intimate partner violence; PHQ-8, Patient Health Questionnaire −8
OR’ represents the OR for the mediated path.
All models adjust for maternal age (years) and ethnicity (Mestizo vs. other).
a P-value < 0.05
b Depression is defined as the PHQ-9 ≥10.
Figure 2. Relation between childhood abuse, intimate partner violence 12 months prior to pregnancy and sleep quality assessed by the Pittsburgh Sleep Quality Index (PSQI) during the first trimester of pregnancy (N=624).
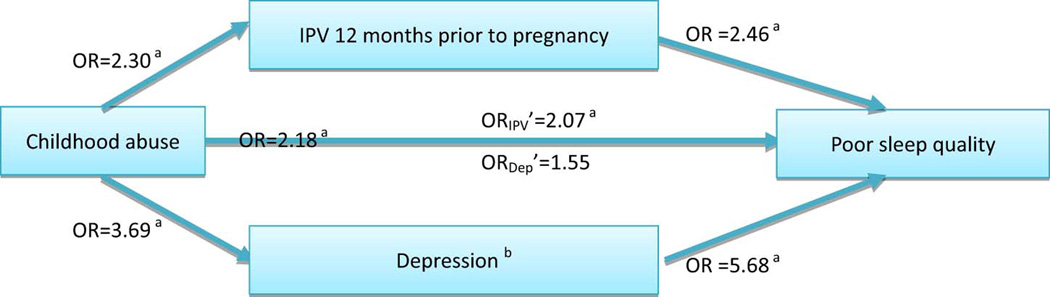
Six women were excluded due to missing information on IPV 12 months prior to pregnancy (n=3) and the PHQ-8 (n=3).
Abbreviation: OR, odds ratio; IPV, intimate partner violence; PHQ-8, Patient Health Questionnaire −8 OR’ represents the OR for the mediated path.
All models adjust for maternal age (years) and ethnicity (Mestizo vs. other).
a P-value < 0.05
b Depression is defined as the PHQ-9 ≥10.
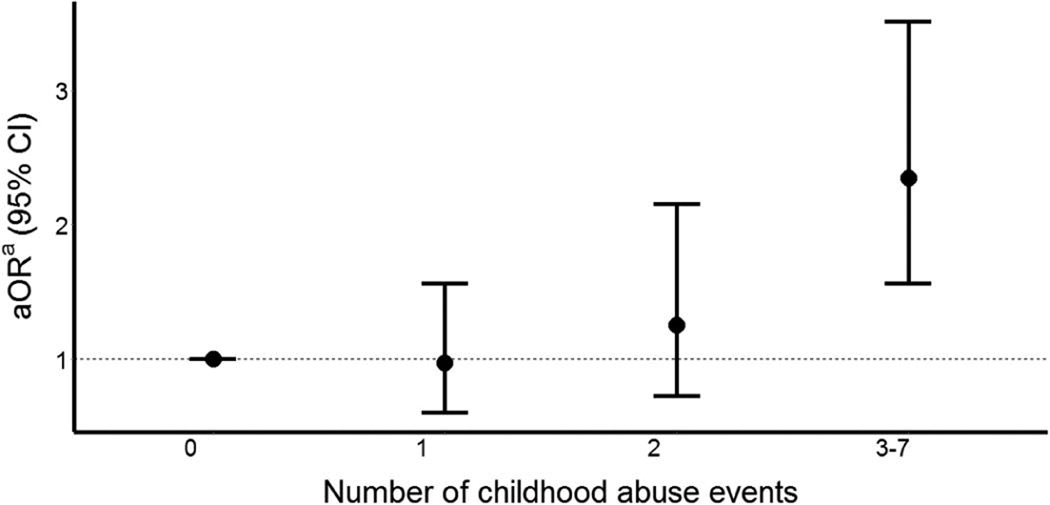
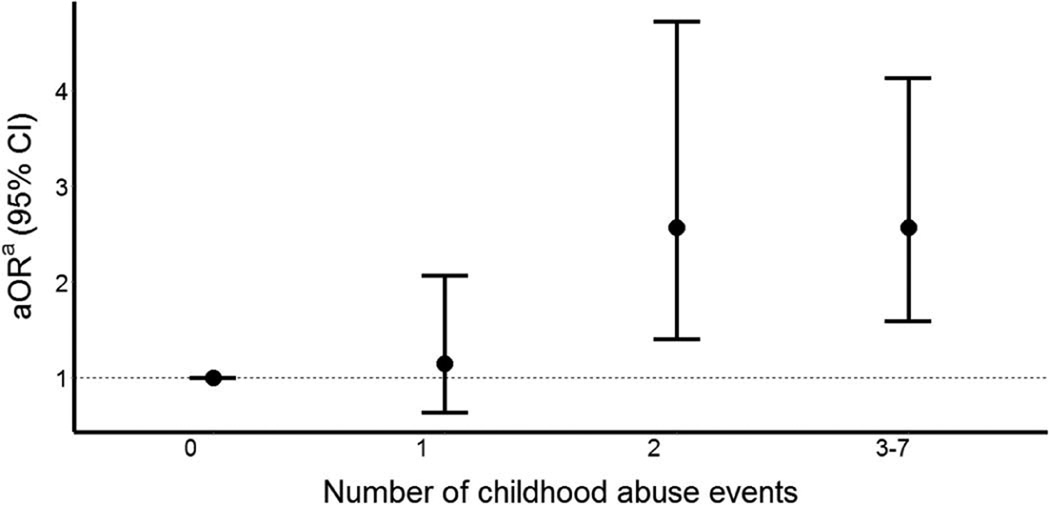
Finally, as shown in Figures 3 and 4, compared with women who reported no childhood abuse, those who reported three or more different types of childhood abuse had higher likelihood of experiencing stress-related sleep disturbance (OR=2.35 95% CI:1.57, 3.51) and poor sleep quality (OR=2.57; 95%CI:1.59, 4.13).
Figure 3. Association between number of childhood abuse events and stress-related sleep disturbance assessed by the Ford Insomnia Response to Stress Test (FIRST-S) during pregnancy (N = 630).
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval
a Adjusted for maternal age (years) at interview and maternal ethnicity (Mestizo vs. other)
P-value for linear trend is <0.0001.
Figure 4. Association between number of childhood abuse events and sleep quality assessed by the Pittsburgh Sleep Quality Index (PSQI) during pregnancy (N = 630).
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval
a Adjusted for maternal age (years) at interview and maternal ethnicity (Mestizo vs. other)
P-value for linear trend is <0.0001.
DISCUSSION
Our study extends the literature by documenting increased odds of stress-related sleep disturbance and poor sleep quality among pregnant women with a history of childhood abuse. Childhood abuse was associated with higher odds of stress-related sleep disturbance (aOR=1.65; 95% CI: 1.15–2.38) and with poor sleep quality (aOR=2.11; 95% CI: 1.35–3.30) during early pregnancy; and these associations were only partially explained by antepartum depression. Recent abuse by an intimate partner was not found to be an important mediator of hypothesized associations.
This study is the first to assess early pregnancy stress-related sleep disturbance and poor sleep quality in relation to history of childhood abuse as characterized by type and frequency of abuse. Our findings are largely similar, however, to reports from studies that have previously assessed associations of childhood abuse with self-reported sleep disturbances among men and non-pregnant women. For instance, in a longitudinal study conducted among 147 non-pregnant women referred by protective service agencies in Washington, D.C., Noll and colleagues documented a statistically significant association of sleep disturbances with childhood sexual abuse that occurred ten years earlier (β = 0.24, p < 0.05).29 In an Israel-based segment of the World Mental Health Survey, Gal et al. found that compared with participants without history of childhood abuse, those with experiences of childhood sexual abuse (OR = 1.7; 95% CI = 1.1–2.7), childhood physical abuse (OR = 2.5; 95% CI = 1.5–4.1), and general childhood abuse (OR = 2.0; 95% CI = 1.5–2.8) had increased odds of self-reported sleep disturbances. 30–33 These observations were corroborated by other investigators who found statistically significant associations of childhood abuse with sleep disturbances.30–33 Our study extends these previous findings by documenting statistically significant associations of childhood abuse with stress-related sleep disturbance among pregnant women, a population known to be particularly vulnerable to sleep disturbances given pregnancy-related physiological changes.1
A substantial body of literature supports increased risks of poor sleep quality (as assessed using the PSQI) among men and non-pregnant women with a history of abuse in childhood.7, 34, 35 For instance Greenfield et al. 7 using data from the National Survey of Midlife Development study found that compared with adults with no abuse history those who experienced frequent physical and emotional with sexual abuse (OR = 3.7; 95% CI = 1.8–7.6), frequent physical and emotional without sexual abuse (OR = 3.3; 95% CI = 1.8–5.9), and occasional physical and emotional with sexual abuse (OR = 1.7; 95% CI = 1.1–2.7) were more likely to experience poor sleep quality (global PSQI score > 5). Similarly in their study of US college students Ramsawh et al. 35 found that mean Childhood Trauma Questionnaire (CTQ) scores were positively associated with PSQI scores (β = 0.26, P < 0.001). Our results are in agreement with these studies. However, our results did not corroborate the findings reported by some investigators. In their study of 63 military veterans, Insana et al. 36 reported that early life trauma, assessed using the Trauma History Questionnaire (THQ), was not statistically significantly associated with sleep quality assessed using the PSQI. Similarly Bader et al. 37 in their study of 59 Swiss adults with primary insomnia found that participants who reported moderate to severe childhood abuse vs. low or no childhood abuse were not statistically significantly different with regards to their PSQI scores (9.9 vs. 9.3, P = 0.437). Discordance in study findings may be attributable, in part, to differences in populations studied, variations in methods of ascertainment and classification of childhood abuse, differences in instruments used to ascertain and define poor sleep quality, and varying degrees of control for confounding factors. On balance, when taken together with our findings, the extant literature suggests that childhood abuse is a risk factor for poor sleep quality in adulthood, including during pregnancy.
Findings from our mediation analyses provided evidence that depressive symptomatology may partially explain the mechanism how childhood abuse could influence adulthood sleep disturbances. There are multiple shared biopsychosocial mechanisms to explain the observed associations between childhood abuse and adult sleep disturbances including corticotropin-releasing hormone concentration and hyperactivity of the hypothalamic-pituitary-adrenal axis.38, 39 Another plausible biological mechanism is that of early exposure to abuse leading to impairments in brain development.40 These developmental deficits may result in mood and anxiety disorders of which sleep disturbance is a symptom.5, 40 However, previous studies have identified significant associations between childhood abuse and adult sleep disorders even after adjusting for mental health status.29, 33, 41–43
In addition, there are social mechanisms that may explain the observed associations. One such social mechanism is that of family chaos or household disruption leading to the failed development of a healthy sleep schedule.5, 7 Another social mechanism that is partly evidenced by our mediation analyses involves the role of violence revictimization in adulthood. Young girls who survive abuse in childhood are more likely to experience further abuse in adulthood12,44, 45 and studies have identified a relationship between adult abuse and sleep disturbance. 29, 46 For example, in their longitudinal study of 147 adult women in the U.S., Noll et al. 29 found that sleep disturbances were associated with recent abuse rates regardless of childhood sexual abuse (β = 0.25, P < 0.01). This evidence suggests a plausible mechanism for the association between childhood abuse and adult sleep disorders, though our results suggest that this does not fully explain the observed associations.
The present study has several strengths, namely the large sample size and the sizeable prevalence of sleep disturbances, giving us ample statistical power to study the associations of interest. We employed a rigorous analytic approach that accounted for potential confounding socio-demographic factors as well as experiences of adulthood abuse. Additionally, our use of multiple measures for sleep disturbances recognizes the multi-faceted nature of sleep health. Some important study limitations, however, must be considered when interpreting the results of our study. The first primary limitation is experience of childhood abuse was assessed based on self-report in this cross-sectional study. Therefore, these measures may be subjected to non-systematic errors in recall, as well as systematic non-disclosure leading to misclassification. Investigators have noted that individuals are likely to minimize experiences of past abuse rather than suggest that they had experienced abuse in their lifetime.47 Such errors in recall may have led to an underestimation of reported odds ratios. To help mitigate the likelihood of systematic reporting errors, well-trained interviewers used a standard questionnaire to collect information from all study participants.48 In addition, neither the interviewers nor study participants were aware of any of the specific study hypotheses. Furthermore, our use of self-reported data for subjective measures of sleep disturbances and other covariates may have introduced some degree of measurement error. Although we used multivariable logistic regression procedures to adjust for putative confounders, we cannot exclude the possibility of residual confounding. Finally, the participants in this study were pregnant women living in Lima, Peru and thus, the results may not be generalizable to other obstetric populations.
Childhood abuse is a pervasive human rights and public health problem with enduring adverse outcomes across the life course.49–51 We found that a history of childhood abuse is associated with increased odds of stress-related sleep disturbance and poor sleep quality during pregnancy. This novel evidence, if replicated, should be used to inform the development of trauma-informed care for such sleep disturbances in pregnancy. Additionally, more research is needed to fully understand the behavioral, neurobiological, and environmental mechanisms that mediate the association of history of childhood abuse and sleep disturbances among pregnant women.
Highlights.
History of childhood abuse (CA) is associated with sleep disturbances during pregnancy
CA was associated with 1.65-fold increased odds of stress-related sleep disturbance
CA was associated with 2.11-fold increased odds of poor sleep quality
The odds of sleep disturbances was much stronger for those who experienced higher number of CA events
Trauma-informed care for sleep disturbances induced by childhood trauma are needed
Acknowledgments
This research was supported by awards from the National Institutes of Health (R01-HD-059835, T37-MD000149 and K01MH100428). The NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. The authors wish to thank the dedicated staff members of Asociacion Civil Proyectos en Salud (PROESA), Peru and Instituto Materno Perinatal, Peru for their expert technical assistance with this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None Declared
References
- 1.Chang JJ, Pien GW, Duntley SP, Macones GA. Sleep deprivation during pregnancy and maternal and fetal outcomes: is there a relationship? Sleep Medicine Reviews. 2010;14:107–114. doi: 10.1016/j.smrv.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skouteris H, Germano C, Wertheim EH, Paxton SJ, Milgrom J. Sleep quality and depression during pregnancy: a prospective study. Journal Of Sleep Research. 2008;17:217–220. doi: 10.1111/j.1365-2869.2008.00655.x. [DOI] [PubMed] [Google Scholar]
- 3.Williams MA, Miller RS, Qiu C, Cripe SM, Gelaye B, Enquobahrie D. Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. Sleep. 2010;33:1363–1371. doi: 10.1093/sleep/33.10.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kajeepeta S, Sanchez SE, Gelaye B, et al. Sleep duration, vital exhaustion, and odds of spontaneous preterm birth: a case-control study. BMC Pregnancy and Childbirth. 2014;14:337. doi: 10.1186/1471-2393-14-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Medicine. 2015 doi: 10.1016/j.sleep.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 7.Greenfield EA, Lee C, Friedman EL, Springer KW. Childhood abuse as a risk factor for sleep problems in adulthood: evidence from a U.S. national study. Annals of Behavioral Medicine. 2011;42:245–256. doi: 10.1007/s12160-011-9285-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heath V, Bean R, Feinauer L. Severity of childhood sexual abuse: Symptom differences between men and women. American Journal of Family Therapy. 1996;24:305–314. [Google Scholar]
- 9.Koskenvuo K, Hublin C, Partinen M, Paunio T, Koskenvuo M. Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Med. 2010;11:17–22. doi: 10.1016/j.sleep.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 10.Barrios YV, Sanchez SE, Nicolaidis C, et al. Childhood abuse and early menarche among peruvian women. Journal of Adolescent Health. 2015;56:197–202. doi: 10.1016/j.jadohealth.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomez-Beloz A, Williams MA, Sanchez SE, Lam N. Intimate partner violence and risk for depression among postpartum women in Lima, Peru. Violence and Victims. 2009;24:380–398. doi: 10.1891/0886-6708.24.3.380. [DOI] [PubMed] [Google Scholar]
- 12.Barrios YV, Gelaye B, Zhong Q, et al. Association of childhood physical and sexual abuse with intimate partner violence, poor general health and depressive symptoms among Pregnant women. PloS One. 2015;10:e0116609. doi: 10.1371/journal.pone.0116609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Felitti M, Vincent J, Anda M, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 14.DHS. [Accessed on May 22, 2015];Demographic Health Survey questionnaires and modules: Domestic violence module. Available at : http://www.measuredhs.com/aboutsurveys/dhs/modulesarchive.cfm.
- 15.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: Findings from the WHO multi-country Study on women’s health and domestic violence. Lancet. 2006;368:1260–1269. doi: 10.1186/1471-2458-11-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep. 2004;27:285–291. doi: 10.1093/sleep/27.2.285. [DOI] [PubMed] [Google Scholar]
- 17.Drake CL, Scofield H, Roth T. Vulnerability to insomnia: the role of familial aggregation. Sleep Med. 2008;9:297–302. doi: 10.1016/j.sleep.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakajima S, Okajima I, Sasai T, et al. Validation of the Japanese version of the Ford Insomnia Response to Stress Test and the association of sleep reactivity with trait anxiety and insomnia. Sleep Medicine. 2014;15:196–202. doi: 10.1016/j.sleep.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez S, Martinez C, Oriol R, et al. Sleep quality, sleep patterns and consumption of energy drinks and other caffeinated beverages among Peruvian college students. Health. 2013;5:26–35. doi: 10.4236/health.2013.58A2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J. Obstet. Gynecol. 2000;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 22.Wulsin L, Somoza E, Heck J. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Prim Care Companion J Clin Psychiatry. 2002;4:191. doi: 10.4088/pcc.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhong Q, Gelaye B, Fann JR, Sanchez SE, Williams MA. Cross-cultural validity of the Spanish version of PHQ-9 among pregnant Peruvian women: A Rasch item response theory analysis. J. Affect. Disord. 2014;158:148–153. doi: 10.1016/j.jad.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen. Intern. Med. 2007;22:1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 26.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- 27.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- 28.Hicks R, Tingley D. MEDIATION: Stata module for causal mediation analysis and sensitivity analysis. S457294 ed: Boston College Department of Economics. 2011 [Google Scholar]
- 29.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. Journal of Pediatric Psychology. 2006;31:469–480. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- 30.Chambers E, Belicki K. Using sleep dysfunction to explore the nature of resilience in adult survivors of childhood abuse or trauma. Child Abuse & Neglect. 1998;22:753–758. doi: 10.1016/s0145-2134(98)00059-3. [DOI] [PubMed] [Google Scholar]
- 31.Chapman DP, Wheaton AG, Anda RF, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12:773–779. doi: 10.1016/j.sleep.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 32.Duval M, McDuff P, Zadra A. Nightmare frequency, nightmare distress, and psychopathology in female victims of childhood maltreatment. J Nerv Ment Dis. 2013;201:767–772. doi: 10.1097/NMD.0b013e3182a214a1. [DOI] [PubMed] [Google Scholar]
- 33.Gal G, Levav I, Gross R. Psychopathology among adults abused during childhood or adolescence: results from the Israel-based World Mental Health Survey. J Nerv Ment Dis. 2011;199:222–229. doi: 10.1097/NMD.0b013e31820c7543. [DOI] [PubMed] [Google Scholar]
- 34.Heitkemper MM, Cain KC, Burr RL, Jun SE, Jarrett ME. Is childhood abuse or neglect associated with symptom reports and physiological measures in women with irritable bowel syndrome? Biol Res Nurs. 2011;13:399–408. doi: 10.1177/1099800410393274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramsawh HJ, Ancoli-Israel S, Sullivan SG, Hitchcock CA, Stein MB. Neuroticism mediates the relationship between childhood adversity and adult sleep quality. Behav Sleep Med. 2011;9:130–143. doi: 10.1080/15402002.2011.583895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Insana SP, Kolko DJ, Germain A. Early-life trauma is associated with rapid eye movement sleep fragmentation among military veterans. Biol Psychol. 2012;89:570–579. doi: 10.1016/j.biopsycho.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bader K, Schafer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res. 2007;16:285–296. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- 38.Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005;90:3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 39.Vgontzas AN, Bixler EO, Lin HM, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. T J Clin Endocrinol Metab. 2001;86:3787–3794. doi: 10.1210/jcem.86.8.7778. [DOI] [PubMed] [Google Scholar]
- 40.Sher L. The concept of post-traumatic mood disorder and its implications for adolescent suicidal behavior. Minerva Pediatrica. 2008;60:1393–1399. [PubMed] [Google Scholar]
- 41.Bader K, Schafer V, Schenkel M, Nissen L, Kuhl HC, Schwander J. Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. J Nerv Ment Dis. 2007;195:588–595. doi: 10.1097/NMD.0b013e318093ed00. [DOI] [PubMed] [Google Scholar]
- 42.Brower KJ, Wojnar M, Sliwerska E, Armitage R, Burmeister M. PER3 polymorphism and insomnia severity in alcohol dependence. Sleep. 2012;35:571–577. doi: 10.5665/sleep.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chapman DP, Liu Y, Presley-Cantrell LR, et al. Adverse childhood experiences frequent insufficient sleep in 5 U.S. States, 2009: a retrospective cohort study. BMC Public Health. 2013;13:3. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCauley J, Kern DE, Kolodner K, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. 1997;277:1362–1368. [PubMed] [Google Scholar]
- 45.Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse & Neglect. 2003;27:1247–1258. doi: 10.1016/j.chiabu.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 46.Chu JA. The revictimization of adult women with histories of childhood abuse. J Psychother Pract. 1992;1:259–269. [PMC free article] [PubMed] [Google Scholar]
- 47.Ellsberg MC, Winkvist A, Pena R, Stenlund H. Women’s strategic responses to violence in Nicaragua. J Epidemiol Community Heal. 2001;55:547–555. doi: 10.1136/jech.55.8.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 49.Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health. 2014;59:359–372. doi: 10.1007/s00038-013-0519-5. [DOI] [PubMed] [Google Scholar]
- 50.Rich-Edwards JW, Mason S, Rexrode K, et al. Physical and sexual abuse in childhood as predictors of early-onset cardiovascular events in women. Circulation. 2012;126:920–927. doi: 10.1161/CIRCULATIONAHA.111.076877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stein DJ, Scott K, Haro Abad JM, et al. Early childhood adversity and later hypertension: data from the World Mental Health Survey. Ann Clin Psychiatr. 2010;22:19–28. [PMC free article] [PubMed] [Google Scholar]