Abstract
Background:
Occupational health has never been a priority for policy makers in India, despite 63% of the Indian population being in the economically productive age group.
Objectives:
The study was designed to find out the morbidity as a result of long-term exposure to pesticides among professional pesticide sprayers in a rural block in Tamil Nadu.
Subjects and Methods:
A cross-sectional study was done in Kaniyambadi block of Vellore district, Tamil Nadu, during July to October 2013. A total of 70 professional pesticide sprayers and 66 people engaged in other occupations were enrolled into the study. The participants were administered a standardized questionnaire apart from measuring pulmonary function and peripheral sensations. Venous blood samples were collected for measuring serum cholinesterase.
Results:
The pesticide sprayers had higher prevalence of breathlessness on activities of daily living (odds ratio [OR]: 3.14, 95% confidence interval [CI]: 1.22–8.07), chronic cough/phlegm (OR: 3.53, 95% CI: 1.09–11.46), symptoms of peripheral sensory neuropathy (OR: 6.66, 95% CI: 2.53–17.51) and recurrent abdominal pain (OR: 3.05, 95% CI: 1.03–9.01), when compared to people engaged in other occupations. Pesticide sprayers also had significantly lower mean peak expiratory low rates and poor peripheral sensations. The serum cholinesterase levels were not statistically different between the groups.
Conclusion:
The pesticide sprayers had a higher morbidity when compared to people engaged in other occupations, and further research is needed to find out methods to prevent the same. Serum cholinesterase may not be a good marker for quantifying exposure to pesticide among sprayers, during a spraying season.
Keywords: Cholinesterase, exposure, pesticides, sprayers, toxicity
INTRODUCTION
Agricultural productivity has tremendously increased globally over the past 50 years mainly due to the Green revolution; but this comes with huge costs to the community in terms of ill effects on human, animal and plant life due with increased use of agrochemicals such as pesticides and fertilizers.[1] Although environmental contamination with pesticides has been widely reported from all major water sources and aquifers throughout the world, lack of comprehensive pesticide movement models severely limit scientific assessments of their direct impact on human health.[2,3] The World Health Organization (WHO) has classified pesticides based on their toxicity to humans as, Class 1A - Extremely hazardous, Class 1B - Highly hazardous, Class 2 - Moderately hazardous, Class 3 - Slightly hazardous and Class U - Unlikely to present any hazard. The WHO classification is primarily based on animal experiments and the oral lethal dose 50 in rats, which is the amount needed to cause death in 50% of the exposed rats in case of an acute exposure. This system of classification using oral and dermal toxicity to rats is a standard method followed in toxicology.[3]
Long-term, high-level exposure to pesticides is usually observed in workers from manufacturing factories, pesticide applicators and agricultural workers who work in places where intensive farming practices are followed. The exposure is generally occupational and does not get the required attention from public health professionals, labor organizations or government regulators as the adverse health effects are initially subtle. The health adverse effects of such exposures are very similar to short-term very high exposure but less dramatic in presentation.[4] A study done among pesticide factory workers in China showed reduced sperm motility and increased chances of sperm aneuploidy among pesticide factory workers when compared to workers from nearby textile factory.[5] A study of reproductive hormone profile among pesticide factory workers in eastern United States showed increased levels on follicle stimulating hormone and decreased testosterone among the participants. The sperm counts and sperm concentrations were also decreased in the workers, which the investigators attributed to hormonal imbalance secondary to testicular damage.[6] Another problem faced by the pesticide factory workers is the prospect of genetic damage which can be harmful for them even after the exposure is stopped. The genetic damages can be carried over to the next generation too, potentially affecting the health of the generations. A study done in Pakistan used the technique of agar gel electrophoresis assay to find out the DNA damage as a result of working in a pesticide factory. The blood leucocytes among the pesticide factory workers had significantly longer comet tail lengths (which is a marker for autosomal DNA damage) when compared to the control population.[7] A study done in Hyderabad among pesticide factory workers, by the Indian Institute of Chemical Technology using similar techniques, also found a similar trend of DNA damage, with signs of genotoxicities having carcinogenic potential. Multivariate analysis of the data showed that exposure to pesticide and smoking were significant risk factors in inducing DNA damage.[8] Abnormal glucose regulation is another area of interest which has been explored. A cross-sectional study done in China showed that 29.3% of the workers from pesticide factories had impaired glucose tolerance or diabetes mellitus as compared to 21.3% in controls. The adjusted prevalence odds ratio (OR) was 1.48 (95% confidence interval [CI] =1.24–1.77).[9] Almost a third of India's economic output is contributed by the agricultural sector, and it employs around 66% of the total workforce. 99% of the workers engaged in agriculture and allied work are unorganized and has very less in terms of healthcare and social security.[10] Pesticide sprayers/applicators form such a group, which is one of the most vulnerable in terms of income, healthcare and social support, yet being in an occupation which involves multiple potential hazards.[11] The study is relevant in the context of the State of Tamil Nadu being the largest user of agricultural pesticides in India with an annual consumption of 12,500 metric tons a year[11] and an agricultural productivity in the range of INR 32,000–INR 47,000/hectare/year in most districts.[12]
SUBJECTS AND METHODS
The study was conducted in Kaniyambadi block, a rural block in Vellore district of Tamil Nadu state consisting of a total population of around 110,000 residing in 82 villages. The Community Health Department of the Christian Medical College (CMC), Vellore, provides community-based integrated health and social development services to the population through the Community Health and Development (CHAD) program. The CHAD program has established a health information system for the block, which is updated through periodic population census and an active morbidity and vital events reporting system. The initial details of diseases and vital events are collected by the local health workers, which is in turn verified and entered into the health information system.[13,14,15] A quantitative study was conducted among active professional pesticide sprayers of Kaniyambadi block of Vellore district, during the period of July to October 2013, which is an active agricultural season in this part of the country due to adequate precipitation and temperature conditions. The identification of participants was done through CHAD health information system and the local health care workers. A total of 70 professional pesticide sprayers and 70 people in the comparison group were identified and approached for the study. The potential participants were contacted and appropriate time for interview and examination was sought and the interview was conducted in the presence of a local health worker. An informed consent was sought if the participant qualified the inclusion and exclusion criteria. Four of the potential participants, among the persons engaged in other occupations, refused to participate. The study was conducted using a local language translation of an interviewer administered semi-structured questionnaire, which had queries on sociodemographic details, occupational exposures, use of personal protection equipment (PPE) and health status. Another questionnaire was administered to age, sex and neighborhood matched people, who were involved in professions other than pesticide spraying, to assess their health status for comparison. Furthermore, the participants were clinically examined for peripheral sensory neuropathy using monofilaments, pulmonary function was assessed by measuring peak expiratory flow rates using a peak flow meter, and around 10 ml of venous blood was collected for estimating random blood sugar and serum cholinesterase levels. The blood sample was transported in vaccine carriers to the lab and was frozen at − 15°C. The biochemical tests were conducted at the clinical biochemistry laboratory of CMC, Vellore. Data entry was done using Epi-info 7.0 (CDC, Atlanta, USA) and analyzed using SPSS version 17.0 (IBM Inc., Chicago, IL, USA).
RESULTS
The mean (standard deviation [SD]) age of the pesticide sprayers who were recruited into the study was 45.7 (10.6) years with an age range of 18–69 years. Among persons engaged in other occupations, the mean (SD) age was 44.9 (10.3) years with an age range of 23–73 years. Eight (12.1%) of the persons engaged in other occupations had an education of intermediate/posthigh school diploma or above, while only 4 (5.7%) of the pesticide sprayers received a similar level of education. The mean (SD) family income of the sprayers was INR 3920 (4003)/month and the incomes ranged from INR 900/month to INR 27,000/month. Similarly, among the persons engaged in other occupations the mean (SD) family income was INR 5242 (4226), and it ranged from INR 1000 to INR 20,000. Among the pesticide sprayers, the maximum number of participants (52.9%) was from the upper lower class, while among the persons engaged in other occupations; maximum number (42.4%) was from the lower middle class, when assessed using Kuppuswamy's scale, modified in 2012.[16] 58 (82.8%) of the pesticide sprayers belonged to the lower and upper lower socioeconomic status (SES) as compared to 32 (48.8%) nonsprayers in this study and this finding was statistically significant with a Chi-square value = 17.9, P < 0.05 [Table 1].
Table 1.
Characteristics of the study participants
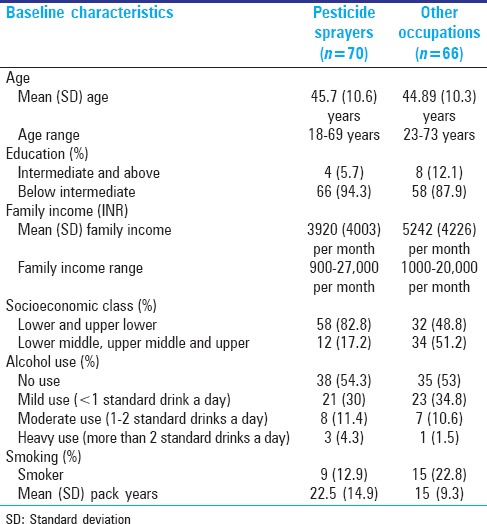
Among the pesticide sprayers, 38 (54.3%) did not report consuming alcohol in the previous 1-month, 21 (30%) reported mild usage, 8 (11.4%) had moderate usage and 3 (4.3%) admitted heavy use of alcohol. Of the persons engaged in other professions, 35 (53%) did not use alcohol in the last 1-month, 23 (47%) admitted to mild use, 7 (10.6%) had moderate intake and 1 (1.5%) reported heavy alcohol use. Among the pesticide sprayers, 9 (12.9%) were smokers while, among the persons engaged in other professions, 15 (22.8%) admitted to smoking. All the pesticide sprayers were smoking beedis, and the mean (SD) duration of smoking as a habit was 22.5 (14.9) years. Among the persons engaged in other occupations, 11 were smoking beedis, and 4 were using cigarettes and the mean (SD) duration was 15 (9.3) years [Table 1].
Eight (11.4%) pesticide sprayers reported to have at least one earlier diagnosed co-morbidity while 13 (19.7%) of the persons engaged in other occupations reported the same. Among the pesticide sprayers, 4 (5.7%) had diabetes mellitus, and 2 (2.9%) had hypertension. Among persons engaged in other occupations, 7 (10.6%) were diagnosed cases of diabetes mellitus, 2 (3%) had hypertension, 1 (1.5%) had Ischemic heart disease and 1 (1.5%) had bronchial asthma/chronic obstructive pulmonary disease.
Among the 70 pesticide sprayers who were participants in the study, 44 (62.9%) were engaged in the spraying profession up to 10 years, 18 (25.7%) between 11 and 20 years and 8 (11.4%) more than 20 years. The mean (SD) duration of exposure was 11.5 (9.9) years with a range of 1–40 years. Pesticides spraying being a highly seasonal occupation, the sprayers are involved in other income generating activities such as agricultural labor, casual labor, handicrafts, etc., for the rest of the year. Of the sprayers in the study, 36 (51.4%) were engaged in spraying activity up to 60 days a year, 25 (35.7%) between 61 and 120 days and 9 (12.9%) were involved in spraying for more than 120 days in a year. The mean (SD) duration of pesticide spraying in a year was 86.1 (44) days and the mean (SD) duration of spraying activities per day was 2.2 (1.1) h. Sixty-one (87.1%) of the pesticide sprayers was satisfied with their current income and 63 (90%) were satisfied with their occupation. Of the 7 participants who expressed dissatisfaction about their occupation, 5 gave low income as the reason and 2 said that health problems are the reason for their dissatisfaction.
Majority (90%) of the sprayers were aware of some of the health problems due to long-term exposure to pesticides. A total of 33 (47.1%) participants were aware of respiratory illnesses and 16 (22.9%) said that exposure can cause giddiness. 31 (44%) of the sprayers were aware of various other adverse effects of pesticide exposure. The pesticide sprayers had multiple sources of information on type of pesticides for each crop, timing of sprays, interval between sprays, etc. 57 (81.4%) sprayers got information on pesticides from the local pesticide sellers, 23 (32.8%) received information from the local agricultural office and their field officers and 4 (5.7%) said they got information from fellow sprayers.
Pesticide procurement, handling and storage practices
All of the participants (100%) procured pesticides from local pesticide retail outlets in and around their villages. A few of them (21.4%) also procured the pesticides from local agricultural co-operative societies. Interestingly, none of the participants received any supply of pesticides from the government. More than half (57.1%) of the sprayers did not store pesticides after buying them, as they buy only the quantity needed for a day's use. However, 28 (40%) of the pesticide sprayers store pesticides at their homes and 2 (2.9%) said they store it in the fields.
All the pesticide sprayers were mixing the pesticide manually, usually using long sticks available at the time of mixing. The mixing of pesticides with water was usually done in large plastic containers measuring more than 20 L. The disposal of empty pesticide containers was done by various methods, 52 (74.4%) threw away the containers after usage at the site of mixing itself, 17 (24.2%) said that the containers are given to rag pickers, while 1 (1.4%) person used it for storage of farm produce and ration supplies. All the participants were using machine sprayers powered by kerosene or petrol. The spraying apparatus was carried on the shoulder as knapsacks, and the nozzle was directed with their hands. Of the 70 pesticide sprayers, 45 (64.3%) used at least one PPE all the time, while 4 (5.7%) used it most of the times, 9 (12.9%) used it sometimes and 3 (4.3%) use it rarely. A total of 9 (12.9%) participants, never used any PPE. Most of those using PPEs were using surgical face masks (and not respirators made for the purpose), with very few using gloves, goggles and protective overalls.
Perceived morbidity, pulmonary function and serum cholinesterase levels among the study participants
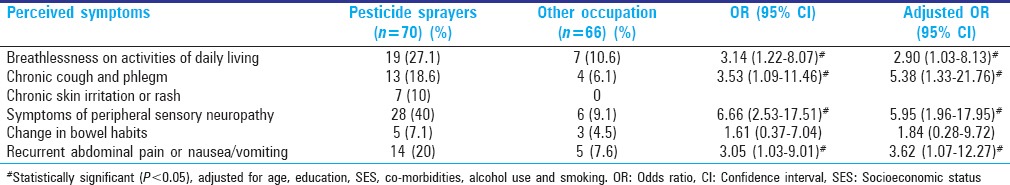
About 27% of the pesticide sprayers reported breathlessness on activities of daily living (ADL), while only 10.6% of persons engaged in other occupations had the complaint (OR = 3.14, 95% CI: 1.22–8.07). Those having chronic chough and phlegm were 18.6% among pesticide sprayers and 6.1% among persons engaged in other occupations (OR = 3.53, 95% CI: 1.09–11.46). Ten percent of the pesticide sprayers had chronic skin irritation or peeling/discoloration of the skin, but none of the persons engaged in other occupations had the problem. When queried about symptoms of peripheral sensory neuropathy in the form of tingling sensation, burning/pricking pain in hands or feet, 40% of the pesticide sprayers and 9.1% of persons engaged in other occupations, had these complaints (OR = 6.66, 95% CI: 2.53–17.51). Chronic abdominal pain, nausea/vomiting were other symptoms which were reported in a high proportion of pesticide sprayers (20% vs. 7.6%) OR = 3.05, 95% CI: 1.03–9.01). Furthermore, multivariate binary logistic regression was performed to look at the effect of age, education, SES, diabetes mellitus, alcohol use and smoking on different symptoms reported among the pesticide sprayers [Table 2].
Table 2.
Perceived symptoms of chronic pesticide toxicity among pesticide sprayers and persons engaged in other occupations
Blood pressures measured using a manual sphygmomanometer showed that only 2 (2.9%) of the pesticide sprayers and 5 (7.6%) of the persons engaged in other occupation had elevated blood pressures. Random plasma blood sugars were measured using a standardized glucometer at the time of participant interview. Four (5.7%) pesticide sprayers and 9 (13.2%) persons engaged in other occupations, showed random plasma blood sugar values of 200 mg/dL and above.
Peak expiratory flow rates were measured using a standardized peak flow meter, and best of three readings were taken for the study. The mean peak flow rate among pesticide sprayers was 346 L/min and that among persons engaged in other occupations was 390 L/min and the difference was statistically significant (P < 0.05). A total of 8 (11.4%) pesticide sprayers and 5 (7.6%) persons engaged in other occupation had impaired peak flow rate of < 300 L/min and this finding was not statistically significant. Peripheral sensory neuropathy was assessed through monofilament examination. Monofilament of various sizes was used, and absent/diminished sensation to 2 g monofilament was considered as a sign of peripheral sensory impairment. 15 (21.4%) pesticide sprayers and 2 (3%) persons engaged in other occupations had impaired absent/diminished sensation when tested with 2 g monofilaments and the difference was statistically significant (P < 0.05) [Table 3].
Table 3.
Clinical and laboratory findings of the study participants
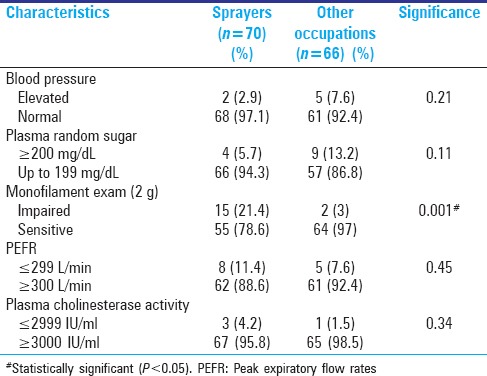
Three (4.2%) of the sprayers and 1 (1.5%) nonsprayer had cholinesterase level < 3000 U/L and the difference was not statistically significant (P <0.05). Among the pesticide sprayers, the mean Cholinesterase level was 7358 U/L and the median was 7640 U/L, with a minimum level of 1497 U/L and a maximum level of 12,163 U/L. Among the persons engaged in other professions, the mean cholinesterase level was 7844 U/L and the median was 8311 U/L, with a minimum level of 1028 and a maximum level of 11,811. The mean cholinesterase levels of pesticide sprayers and persons engaged in other occupations were not statistically different (P < 0.05). As agriculturists form a significant part of other occupations, they can also be exposed to pesticides, during farming activities, therefore the participants were further divided into sprayers, agriculturists and other professions, for analyzing serum cholinesterase levels among them. The mean cholinesterase level among agriculturists was 7366 IU/L, other professions were 8321 IU/L and among pesticide sprayers, it was 7358 IU/L and the differences were not statistically different on comparison using ANOVA technique (F = 2.03, P > 0.05).
No increase in the prevalence of perceived symptoms or signs were observed with was an increase in duration of exposure (in years) but chronic cough and phlegm (OR = 4.58, 95% CI: 1.13–3.59) and recurrent abdominal pain, nausea/vomiting (OR = 5.26, 95% CI: 1.31–20.97) was seen in a significantly higher proportion of pesticide sprayers who had exposure of more than 60 days of spraying in the last 1-year.
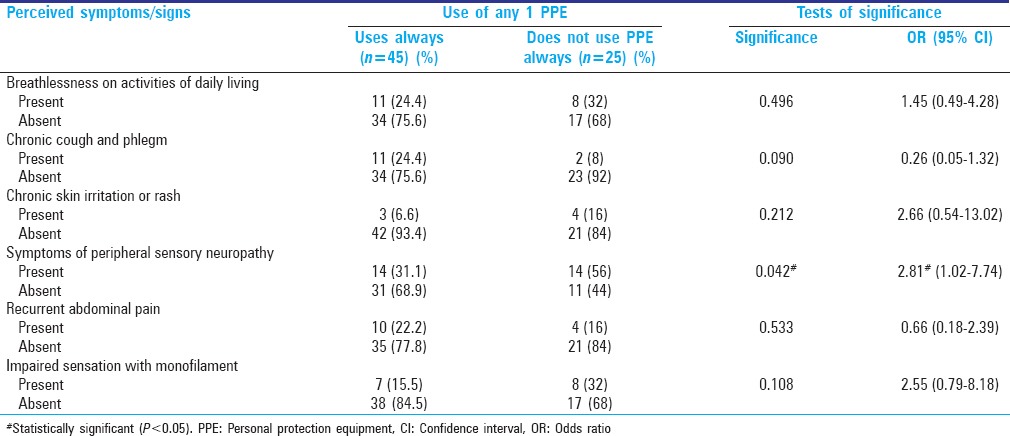
Furthermore, it was found that the use of PPEs did not affect the perceived symptoms/signs except symptoms of peripheral sensory neuropathy which was found to be significantly increased among pesticide sprayers who did not use PPE or used it sparingly, when compared to those sprayers who always use at least one PPE while spraying (OR = 2.81, 95% CI: 1.02–7.74) [Table 4].
Table 4.
Perceived symptoms and signs of chronic toxicity among pesticide sprayers and use of PPE
DISCUSSION
Pesticides are volatile and get aerosolized easily, so when breathed in, they can cause irritation and subsequent damage to airways which can result in symptoms of chronic bronchitis. Furthermore, some of the aerosols will reach the alveolar space and cause damage to the alveolar sacs and can cause breathlessness.[17] The significantly higher prevalence of breathlessness on ADL among the pesticide sprayers (27% vs. 10%) in this study suggests that pesticide sprayers are at an increased risk of having breathlessness on ADL, corroborates previous study reports from India and other parts of the world.[18,19] Similarly, 18.6% of the pesticide sprayers reported chronic cough and phlegm as compared to only 6.1% of the persons engaged in other occupations. Organophosphorus pesticides, when exposed to skin, can result in local symptoms due to irritation and allergy, as well as absorption into the blood stream due to its lipophilic nature.[20] In this study, 10% of the pesticide sprayers reported chronic skin irritation and skin rashes/discoloration while none of the persons engaged in other occupations had the problem. Symptoms of peripheral sensory neuropathy were also present among 28 (40%) of the pesticide sprayers, as compared to 6 (9.1%) of the persons engaged in other occupations. This is significantly higher than reports from previous studies which reported symptoms of peripheral sensory neuropathy to be 15–27%.[21] Furthermore, the pesticide sprayers had a higher prevalence (20%) of recurrent abdominal pain/nausea/vomiting, when compared to the persons engaged in other occupations (7.6%). There were no participants with symptoms of peripheral motor neuropathy or Parkinsonism. Multivariate analyses adjusting for other risk factors and confounders revealed that after adjusting for various risk factors, the sprayers had significantly higher burden of the perceived symptoms of exposure. Lung function was assessed using a peak flow meter as it is more portable and economical when compared to spirometers, and the peak flow rates obtained using peak flow meters are similar to the rates obtained using a spirometer.[22] The mean peak flow rate among pesticide sprayers (346 L/min) was significantly lower when compared to persons engaged in other occupations (390 L/min). A total of 8 (11.4%) pesticide sprayers and 5 (7.6%) persons engaged in other occupations had peak flow rates of < 300 L/min, the cut-off value to identify impaired lung function. This difference however was not statistically significant. Previously published studies have demonstrated that a significant proportion of pesticide sprayers had impaired lung function when compared to the general population.[17] This may be because of improper use of the peak flow meter as it requires training of participants for its proper use, making the results subjective in nature.
Monofilaments were used to assess for peripheral sensory neuropathy, as it offers similar sensitivity and specificity to vibration thresholds tested using biothesiometers, at minimal costs.[23] Fifteen (21.4%) pesticide sprayers and 2 (3%) persons engaged in other occupations had impaired peripheral sensation, when tested with a 2 g monofilament and the difference was significant on statistical analysis. This finding is in concordance with multiple other studies from across the world, which demonstrated the neurotoxicity of pesticides resulting in impaired peripheral sensations.[24,25] The mean cholinesterase level among pesticide sprayers was lower than the general population although not statistically significant.
Pesticide sprayers experience higher perceived and clinically estimated morbidity than the general population. Awareness and use of PPE are inadequate. Multiple strategies focusing on raising awareness and improving practices with usage of PPE along with regular, periodic health assessments by primary health care providers are needed to address this under-recognized public health problem in our communities.
ACKNOWLEDGMENTS
The authors would like to acknowledge the help and guidance of Drs. Kuryan George, and Vinohar Balraj from the Department of Community Health, Christian Medical College, Vellore, Tamil Nadu, India.
Footnotes
Source of Support: Fluid Researc Grant, Christian Medical College, Vellore
Conflict of Interest: None declared.
REFERENCES
- 1.Kookana RS, Baskaran S, Naidu R. Pesticide fate and behaviour in Australian soils in relation to contamination and management of soil and water: A review. Aust J Soil Res. 1999;36:715–64. [Google Scholar]
- 2.Akram K, Tung L. Mapping pesticide contamination potential. Environ Manage. 1989;13:233–42. [Google Scholar]
- 3.Geneva: WHO; 2009. International Program on Chemical Safety. The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification. [Google Scholar]
- 4.Palacios-Nava ME, Paz-Román P, Hernández-Robles S, Mendoza-Alvarado L. Persistent symptomatology in workers industrially exposed to organophosphate pesticides. Salud Publica Mex. 1999;41:55–61. [PubMed] [Google Scholar]
- 5.Padungtod C, Hassold TJ, Millie E, Ryan LM, Savitz DA, Christiani DC, et al. Sperm aneuploidy among Chinese pesticide factory workers: Scoring by the FISH method. Am J Ind Med. 1999;36:230–8. doi: 10.1002/(sici)1097-0274(199908)36:2<230::aid-ajim2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 6.Padungtod C, Lasley BL, Christiani DC, Ryan LM, Xu X. Reproductive hormone profile among pesticide factory workers. J Occup Environ Med. 1998;40:1038–47. doi: 10.1097/00043764-199812000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Bhalli JA, Khan QM, Nasim A. DNA damage in Pakistani pesticide-manufacturing workers assayed using the Comet assay. Environ Mol Mutagen. 2006;47:587–93. doi: 10.1002/em.20232. [DOI] [PubMed] [Google Scholar]
- 8.Grover P, Danadevi K, Mahboob M, Rozati R, Banu BS, Rahman MF. Evaluation of genetic damage in workers employed in pesticide production utilizing the Comet assay. Mutagenesis. 2003;18:201–5. doi: 10.1093/mutage/18.2.201. [DOI] [PubMed] [Google Scholar]
- 9.Wang J, Zhu Y, Cai X, Yu J, Yang X, Cheng J. Abnormal glucose regulation in pyrethroid pesticide factory workers. Chemosphere. 2011;82:1080–2. doi: 10.1016/j.chemosphere.2010.10.065. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Occupational Health. [Last accessed on 2013 Nov 20]. Available from: http://www.who.int/topics/occupational_health/en/
- 11.Joshi TK, Mittal A. WHO; 2012. Need for coherent pesticide policy in India. Intergovernmental Forum on Chemical Safety, Forum Standing Committee. [Google Scholar]
- 12.Ramesh C, Sanjeev G, Lalmani P. New Delhi: National Centre for Agricultural Economics and Policy Research; 2009. Regional Variations in Agricultural Productivity: A District Level Study. National Research Project. [Google Scholar]
- 13.Krishnakumar A. A century of service. Hindu. 1999;16:11. [Google Scholar]
- 14.Community Health and Development-CMC Vellore. [Last accessed on 2013 Nov 20]. Available from: http://www.accessh.org/CaseStudies_Pdf/Community%20Health%20and%20Development%20-%20CMC%20Vellore.pdf .
- 15.Mohan VR, Muliyil J. Mortality patterns and the effect of socioeconomic factors on mortality in rural Tamil Nadu, south India: A community-based cohort study. Trans R Soc Trop Med Hyg. 2009;103:801–6. doi: 10.1016/j.trstmh.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Mohan B, Meena R, Sandeep S. Modified kuppuswamy's socioeconomic scale: Social researcher should include updated income criteria. Indian J Community Med. 2013;38:185–6. doi: 10.4103/0970-0218.116358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fareed M, Pathak MK, Bihari V, Kamal R, Srivastava AK, Kesavachandran CN. Adverse respiratory health and hematological alterations among agricultural workers occupationally exposed to organophosphate pesticides: A cross-sectional study in North India. PLoS One. 2013;8:e69755. doi: 10.1371/journal.pone.0069755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mekonnen Y, Agonafir T. Lung function and respiratory symptoms of pesticide sprayers in state farms of Ethiopia. Ethiop Med J. 2004;42:261–6. [PubMed] [Google Scholar]
- 19.Pathak MK, Fareed M, Bihari V, Mathur N, Srivastava AK, Kuddus M, et al. Cholinesterase levels and morbidity in pesticide sprayers in North India. Occup Med (Lond) 2011;61:512–4. doi: 10.1093/occmed/kqr064. [DOI] [PubMed] [Google Scholar]
- 20.van der Merwe D, Brooks JD, Gehring R, Baynes RE, Monteiro-Riviere NA, Riviere JE. A physiologically based pharmacokinetic model of organophosphate dermal absorption. Toxicol Sci. 2006;89:188–204. doi: 10.1093/toxsci/kfj014. [DOI] [PubMed] [Google Scholar]
- 21.Kamel F, Engel LS, Gladen BC, Hoppin JA, Alavanja MC, Sandler DP. Neurologic symptoms in licensed pesticide applicators in the Agricultural Health Study. Hum Exp Toxicol. 2007;26:243–50. doi: 10.1177/0960327107070582. [DOI] [PubMed] [Google Scholar]
- 22.Pesola GR, O'Donnell P, Pesola HR, Saari AF. Comparison of peak flow meter versus spirometric peak flows in normal volunteers. B48 Pulmonary Diagnostic Studies and Cough. American Thoracic Society. 2011. [Last accessed on 2013 Dec 20]. p. A3128. Available from: http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2011.183.1_MeetingAbstracts.A3128 .
- 23.Olaleye D, Perkins BA, Bril V. Evaluation of three screening tests and a risk assessment model for diagnosing peripheral neuropathy in the diabetes clinic. Diabetes Res Clin Pract. 2001;54:115–28. doi: 10.1016/s0168-8227(01)00278-9. [DOI] [PubMed] [Google Scholar]
- 24.Stokes L, Stark A, Marshall E, Narang A. Neurotoxicity among pesticide applicators exposed to organophosphates. Occup Environ Med. 1995;52:648–53. doi: 10.1136/oem.52.10.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pilkington A, Buchanan D, Jamal GA, Gillham R, Hansen S, Kidd M, et al. An epidemiological study of the relations between exposure to organophosphate pesticides and indices of chronic peripheral neuropathy and neuropsychological abnormalities in sheep farmers and dippers. Occup Environ Med. 2001;58:702–10. doi: 10.1136/oem.58.11.702. [DOI] [PMC free article] [PubMed] [Google Scholar]


