Abstract
Background
Stress can cause psychological and physiological changes. Many studies revealed that massage can decrease stress. However, traditional Thai massage has not been well researched in this regard. The purpose of this study was to investigate the immediate effects of traditional Thai massage (TTM) on salivary alpha-amylase levels (sAA), heart rate variability (HRV), autonomic nervous system (ANS) function, and plasma renin activity (PRA).
Material/Methods
Twenty-nine healthy participants were randomly allocated into either a traditional Thai massage (TTM) group or Control (C) group, after which they were switched to the other group with a 2-week wash-out period. Each of them was given a 10-minute mental arithmetic test to induce psychological stress before a 1-hour session of TTM or rest.
Results
Within-groups comparison revealed that sAA was significantly decreased (p<0.05) in the TTM group but not in the C group. HRV and ANS function were significantly increased (p<0.05) and PRA was significantly decreased (p<0.05) in both groups. However, low frequency per high frequency ratio (LF/HF ratio) and ANS balance status were not changed. Only sAA was found to be significantly different between groups (p<0.05).
Conclusions
We conclude that both TTM and rest can reduce psychological stress, as indicated by decreased sAA levels, increased parasympathetic activity, decreased sympathetic activity, and decreased PRA. However, TTM may have a modest effect on stress reduction as indicated by a reduced sAA.
MeSH Keywords: Adaptation, Psychological; Salivary alpha-Amylases; Severe Dengue
Background
Stress affects all body systems (e.g., cardiovascular, respiratory, neuromuscular, and endocrine), resulting in psychological and physiological changes. During stress, the cerebral cortex sends signals to the autonomic nervous system. The sympathetic nervous system becomes activated and sympathetic activity increases, resulting in increased HR and changes in HRV [1–5], decreasing peripheral blood flow and renal blood flow, and increased blood pressure and vascular resistance [6–10]. Moreover, preganglionic nerves of the sympathetic nervous system send signals to epithelial acinar cells in the salivary gland, leading to increases saliva secretion and sAA levels [11–13].
Furthermore, in the stress condition many sympathetic nerve signals into the kidney increase renal sympathetic nerve activity (RSNA), which consequently and complexly leads to a decreased blood circulation to the kidney. Increased RSNA leads to glomerular afferent arteriole contraction and results in increased vascular resistance. This also stimulates the rennin-angiotensin-aldosterone system (RAAS) to release renin, because since rennin hydrolyzes angiotensinogen released from the liver and then converts it to angiotensin I (AI). AI is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE), which is released from the lung. AII causes glomerular afferent arteriole contraction, resulting in increased BP and decreased blood circulation [14,15]. In addition, previous studies also found that mental stress can decrease renal blood flow (RBF) [6–10].
The main treatments of stress include psychiatric treatment and pharmacotherapy. Another choice that has been suggested to reduce stress is massage [16,17]. Traditional Thai massage (TTM) is an alternative treatment using the thumbs to apply deep massage, often combined with muscle stretching at the end of the session. The benefits of massage have been found to include increased skin temperature and blood flow [18–20], decreased anxiety [21–24], decreased depression [24], increased RBF [25], decreased sympathetic activity and increased parasympathetic activity [22,26,27], and decreased cortisol levels [26,28]. It has been suggested that the mechanism by which massage causes these physiological changes is the gentle mechanical pressure applied during massage, which may increase muscle compliance, blood flow, muscle temperature, and parasympathetic activity, and decrease neuromuscular excitability, anxiety, and stress hormone level, thus, resulting in a relaxation response [29].
Although many studies reported the effects of massage on physiological mechanisms, none have explored the effects of massage on plasma renin activity, which may be associated with changes in psychological stress. The current study aimed to determine whether TTM decreases sAA levels, increases HRV, increases ANS function, decreases stress, and decreases plasma renin activity.
Material and Methods
Study design and participants
This study was a crossover randomized controlled trial, which was approved by the ethics committee of Khon Kaen University, Thailand (HE561485). Thirty participants were recruited in this study; 1 participant dropped out at the beginning of the study because of personal obligations, leaving 29 healthy participants (male=7, female=22), average age 35.17±6.35 years old, and they participated in and completed all procedures. Each signed informed consent to participate. All of the participants had mild stress levels (21.72±1.41) as assessed by the Suanprung Stress Test-20. The participants were advised to refrain from eating, drinking alcohol, smoking, and consuming caffeine for at least 2 hours before participating in this study. The participants were excluded from this study if during the study they had any kind of medication or other medical treatments, moderate to severe of muscle or joint pain, impaired skin sensation or hypersensitivity to massage, history of serious disease that must be treated by a doctor, or who had moderate-to-severe stress recently as assessed by the Suanprung Stress Test-20, or menopause.
Procedure and protocol
Twenty-nine healthy participants were randomly allocated into either traditional the Thai massage (TTM) group or the Control (C) group, after which they were switched to the other group, with a 2-week wash-out period (Figure 1). They were given a 10-minute mental arithmetic test to induce mental stress before a 1-hour session of TTM or rest. Immediately after mental arithmetic and TTM or rest, we measured the participants’ HR, SDNN, RMSSD, HF, LF, LF/HF ratio, ANS activity, ANS balance status, stress index, stress resistance, mental stress, and PRA and sAA levels.
Figure 1.
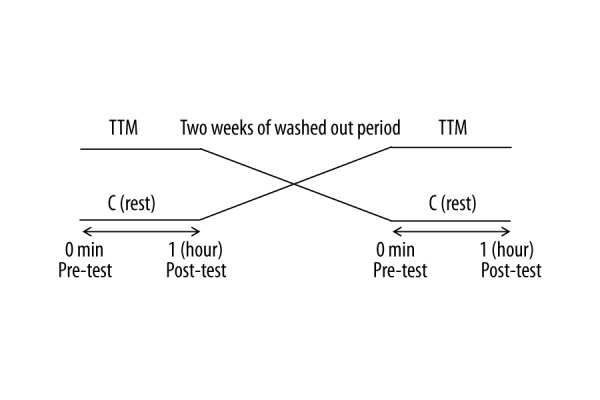
Diagram on crossover design used in this study. TTM and C group: 1 hour for each protocol, 1 trial per protocols, and 2 weeks of wash out period. TTM: traditional Thai massage, C: Control or rest.
Salivary alpha-amylase (sAA) levels assessment
The participants were asked to spit before assessment in order to get newly-produced saliva. Then after chewing cotton wool for 1 minute to induce excretion of saliva, participants put the edge of the test strip (saliva-collecting paper) into the mouth, and left it underneath the tongue (sublingual) for 2 minutes. After that, the test strip was fit into the handle sleeve and slid into the Cocoro meter (NiproCo., LTD., Japan). The outcome appeared as a numerical display on the screen, with the unit of measurement in KU/L.
Heart rate variability (HRV), autonomic nervous system (ANS) function and stress assessment
The participants sat on a comfortable chair with a backrest, with eyes opened and breathing normally throughout the 5 minutes of data collection. The HRV parameters were measured by use of a SA-3000P device (Medicore Co., LTD., Korea) and the measurement procedures followed the SA-3000P Operation Manual Version 2.8. HR, SDNN, RMSSD, HF, LF, and LF/HF ratio were used to evaluate HRV. ANS activity, ANS balance status, stress resistance, and stress index were used to reflect ANS function and stress, respectively. Psychological stress was measured by Faces Rating Scale, which consisted of 10 scales.
Plasma renin activity (PRA) assessment
The participants lay on the bed for 5 minutes, after which 5 ml of blood was drawn from the median cubital vein. The blood sample was delivered for measurement of plasma renin activity and was tested at a standard laboratory center at King Chulalongkorn Memorial Hospital.
Traditional Thai massage (TTM) and rest
The participants received a 1-hour session of the TTM or rest in the control experimental room (25–26°C). Moderate thumb and palm pressure of the TTM was applied along the meridian lines on all parts of the body, including lower limbs, back, neck, head, and upper limbs. The massage was performed in supine, lying on the left side, and lying on the right side (Figure 2). At the end of the massage for each part, the participants had passive stretches for the corresponding muscle groups. In the C group, the participants lay on the bed in supine or side-lying positions, based on their preferences.
Figure 2.
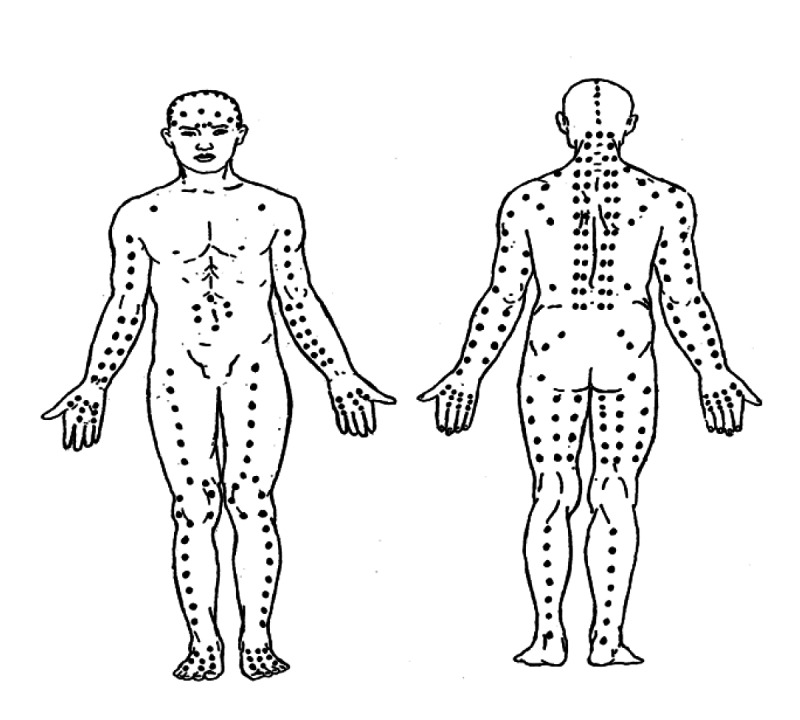
The points on the meridian lines massage of TTM as depicted by Wichai Eungpinichpong [32].
Statistical analysis
The data were presented as mean ±SD. Shapiro-Wilk test was used to evaluate for normal distribution. Crossover study design analysis was used to compare the mean within group and between groups. ANCOVA using baseline as covariate was calculated to compare between groups in case of carry over effect (HR and mental stress). Statistical significance was set at the p≤0.05.
Results
Table 1 shows within-groups comparison, showing that sAA was significantly decreased (p<0.05) in the TTM group but not in the C group. SDNN, RMSSD, HF, LF, stress resistance, and ANS activity were significantly increased (p<0.05), whereas HR, stress index, psychological stress, and PRA were significantly decreased (p<0.05) in both groups. However, low frequency per high frequency ratio (LF/HF ratio) and ANS balance status were not changed. When comparing the outcomes between groups, we found that only sAA was significantly different (p<0.05) and other variables showed no significant differences between the comparison groups (Table 2).
Table 1.
Comparison on the outcome measures within each group (compare between immediately after mental arithmetic test and after each protocol).
| Outcome | TTM group (n=29) | Control group (n=29) | ||
|---|---|---|---|---|
| After test | After TTM | After test | After rest | |
| sAA levels (KU/L) | 5.00±1.95 | 3.69±2.35** | 4.41±1.24 | 4.9±1.26 |
| HR (bpm) | 78.28±9.94 | 73.9±9.56** | 78.1±11.6 | 74.03±9.93** |
| SDNN (ms) | 42.28±23.65 | 51.67±20.09** | 38.63±15.56 | 49.96±16.95** |
| RMSSD (ms) | 27.44±15.37 | 34.38±19.57** | 27.18±16.41 | 32.94±16.83** |
| HF (ms2) | 4.81±1.03 | 5.25±1.07** | 4.76±1.27 | 5.27±1.1** |
| LF (ms2) | 5.58±0.84 | 6.14±1.02** | 5.50±0.80 | 6.06±0.97** |
| LF/HF ratio | 2.84±2.2 | 3.69±3.48 | 3.15±3.27 | 3.46±3.73 |
| ANS activity | 95.48±19.51 | 104±15.28* | 93.28±15.24 | 103.62±14.86** |
| ANS balance | 57.14±39.4 | 65.86±40.84 | 52.28±43.22 | 56.76±46.13 |
| Stress index | 96.79±14.87 | 88.10±11.66** | 100.72±17.61 | 91.86±9.55** |
| Stress resistance | 96.66±17.1 | 105.28±16.37** | 92.00±14.85 | 103.03±13.87** |
| Mental stress | 4.9±1.84 | 1.1±1.57** | 4.62±1.92 | 1.66±1.42** |
| PRA (ng/ml/hr.) | 6.55±5.65 | 5.26±4.68* | 8.58±5.63 | 6.18±5.3** |
Data are expressed as mean ±SD. TTM – traditional Thai massage; sAA levels – salivary alpha-amylase levels; HR – heart rate; SDNN – the standard deviation of the normal-to normal intervals; RMSSD – the square root of the mean squared differences of successive normal R-R intervals; HF – high frequency; LF – low frequency; LF/HF ratio – low frequency per high frequency ratio; ANS activity – autonomic nervous system activity; ANS balance – autonomic nervous system balance; PRA – plasma renin activity. Significant change within group,
p<0.05,
p<0.01.
Table 2.
Comparison on the outcome measures between the groups (compare between immediately after mental arithmetic test and the protocols).
| Outcome | Compared after test | Compared after protocols | ||
|---|---|---|---|---|
| TTM (n=29) | Rest (n=29) | TTM (n=29) | Rest (n=29) | |
| sAA levels (KU/L) | 5.00±1.95 | 4.41±1.24 | 3.69±2.35 | 4.9±1.26* |
| HR (bpm) | 78.28±9.94 | 78.1±11.6 | 73.9±9.56 | 74.03±9.93 |
| SDNN (ms) | 42.28±23.65 | 38.63±15.56 | 51.67±20.09 | 49.96±16.95 |
| RMSSD (ms) | 27.44±15.37 | 27.18±16.41 | 34.38±19.57 | 32.94±16.83 |
| HF (ms2) | 4.81±1.03 | 4.76±1.27 | 5.25±1.07 | 5.27±1.1 |
| LF (ms2) | 5.58±0.84 | 5.50±0.80 | 6.14±1.02 | 6.06±0.97 |
| LF/HF ratio | 2.84±2.2 | 3.15±3.27 | 3.69±3.48 | 3.46±3.73 |
| ANS activity | 95.48±19.51 | 93.28±15.24 | 104±15.28 | 103.62±14.86 |
| ANS balance | 57.14±39.4 | 52.28±43.22 | 65.86±40.84 | 56.76±46.13 |
| Stress index | 96.79±14.87 | 100.72±17.61 | 88.10±11.66 | 91.86±9.55 |
| Stress resistance | 96.66±17.1 | 92.00±14.85 | 105.28±16.37 | 103.03±13.87 |
| Mental stress | 4.9±1.84 | 4.62±1.92 | 1.1±1.57 | 1.66±1.42 |
| PRA (ng/ml/hr.) | 6.55±5.65 | 8.58±5.63 | 5.26±4.68 | 6.18±5.3 |
Data are expressed as mean ±SD. TTM – traditional Thai massage; sAA levels – salivary alpha-amylase levels; HR – heart rate; SDNN – the standard deviation of the normal-to normal intervals; RMSSD – the square root of the mean squared differences of successive normal R-R intervals; HF – high frequency; LF – low frequency; LF/HF ratio – low frequency per high frequency ratio; ANS activity – autonomic nervous system activity; ANS balance – autonomic nervous system balance; PRA – plasma renin activity.
Significant difference between the groups (p<0.05).
Discussion
Stress stimulates sympathetic activity and causes increased HR and HRV changes [1–5]. In addition, it can increase blood pressure, increase vascular resistance, decrease renal blood flow [6–10], and sAA levels [11–13]. This study showed that TTM can significantly reduce psychological stress, as well as decrease sAA levels, increase HRV, increase ANS activity, and decrease plasma renin activity (Table 1).
Salivary glands respond to stress by increasing saliva secretion from stimulation of the sympathetic nervous system. The present study showed that sAA was significantly decreased after TTM. Although the decreased sAA was also found in the C group, the between-group comparison revealed that the decrease of sAA was also significantly different. It is possible that TTM can decrease stress and sympathetic activity and lead to decreased sAA levels.
Previous studies have shown that massage can increase ANS activity [21], decrease sympathetic activity, and increase parasympathetic activity [22,26,27]. The results found in the current study, although we used a different type of massage, were in line with those found in previous studies, which can be seen from the decreased HR, and increased SDNN, RMSSD, HF, and ANS activity. These results indicate that TTM can increase parasympathetic activity and decrease sympathetic activity. Although LF was shown to be significantly increased after TTM, it des not measure sympathetic activity directly, but the increase in LF represents the increased baroreflex function [30,31]. The LF/HF ratio and ANS balance status were not significantly changed, but they were slightly increased after TTM. This could be because both variables increased to maintain the balance between sympathetic and parasympathetic activity.
This study found that stress index and psychological stress were decreased and stress resistance was increased after TTM. Stress resistance is the adaptability of the body against stress, whereas the stress index is the level of stress in the body. Thus, TTM could increase parasympathetic activity, leading to relaxation and reduced stress.
Stress affects the renal sympathetic activity, stimulating rennin-angiotensin-aldosterone system (RAAS) to release rennin. Renin is an important substrate to increase AII, which causes an increase in blood pressure and decreased blood circulation [14,15]. The present study found that TTM can decrease stress and sympathetic activity and increase parasympathetic activity, resulting in decreased PRA.
Although many variables were found significantly changed after TTM, only sAA was found to be significantly different from the C group. When compared between groups, TTM seemed to have better effects than rest. We calculated the sample size from salivary cortisol, which was similar to salivary alpha-amylase, thus, only the sAA levels showed a significant difference between the comparison groups. The current study focused on the immediate effects of massage, and we do not know whether long-term and cumulative effects of TTM would alter these parameters. Therefore, studies in the future should verify the long-term effects of TTM on HRV, ANS function, mental stress, and PRA. If TTM has these long-term effects, it may be useful as a complementary therapy for patients who have chronic stress, anxiety, and depressive disorders.
Conclusions
The current study has demonstrated that TTM can reduce psychological stress, as indicated by decreased sAA levels. We also found that TTM can increase HRV, as indicated by the increase of SDNN, RMSSD, HF, and LF. The increase in ANS function was indicated by increased ANS activity and stress resistance, and decreased stress index and plasma rennin activity. Further studies should focus on long-term effects of TTM on these parameters.
Acknowledgments
We thank the volunteers who participated in the study. Our special thanks to the Thai Traditional Medical Knowledge Fund, Research Center in Back, Neck, Other Joint Pain and Human Performance, Khon Kaen University, and Graduate School of Khon Kaen University, for funding this study.
Footnotes
Source of support: Departmental sources
References
- 1.Chandola T, Heraclides A, Kumari M. Psychophysiological biomarkers of workplace stressors. Neurosci Biobehav Rev. 2010;35(1):51–57. doi: 10.1016/j.neubiorev.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Z, Snieder H, Su S, et al. A longitudinal study in youth of heart rate variability at rest and in response to stress. Int J Psychophysiol. 2009;73(3):212–17. doi: 10.1016/j.ijpsycho.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X, Ding X, Su S, et al. Genetic influences on heart rate variability at rest and during stress. Psychophysiology. 2009;46(3):458–65. doi: 10.1111/j.1469-8986.2009.00793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schubert C, Lambertz M, Nelesen RA, et al. Effects of stress on heart rate complexity – a comparison between short-term and chronic stress. Biol Psychol. 2009;80(3):325–32. doi: 10.1016/j.biopsycho.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orsila R, Virtanen M, Luukkaala T, et al. Perceived mental stress and reactions in heart rate variability – a pilot study among employees of an electronics company. Int J Occup Saf Ergon. 2008;14(3):275–83. doi: 10.1080/10803548.2008.11076767. [DOI] [PubMed] [Google Scholar]
- 6.Kuipers NT, Sauder CL, Carter JR, et al. Neurovascular responses to mental stress in the supine and upright postures. J Appl Physiol. 2008;104(4):1129–36. doi: 10.1152/japplphysiol.01285.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayashi N, Someya N, Endo MY, et al. Vasoconstriction and blood flow responses in visceral arteries to mental task in humans. Exp Physiol. 2006;91(1):215–20. doi: 10.1113/expphysiol.2005.031971. [DOI] [PubMed] [Google Scholar]
- 8.Middlekauff HR, Nguyen AH, Negrao CE, et al. Impact of acute mental stress on sympathetic nerve activity and regional blood flow in advanced heart failure: implications for “triggering” adverse cardiac events. Circulation. 1997;96(6):1835–42. doi: 10.1161/01.cir.96.6.1835. [DOI] [PubMed] [Google Scholar]
- 9.Castellani S, Ungar A, La Cava G, et al. Renal adaptation to stress: a possible role of endothelin release and prostaglandin modulation in the human subject. J Lab Clin Med. 1997;129(4):462–69. doi: 10.1016/s0022-2143(97)90080-9. [DOI] [PubMed] [Google Scholar]
- 10.Tidgren B, Hjemdahl P. Renal responses to mental stress and epinephrine in humans. Am J Physiol. 1989;257(4 Pt 2):F682–89. doi: 10.1152/ajprenal.1989.257.4.F682. [DOI] [PubMed] [Google Scholar]
- 11.Maruyama Y, Kawano A, Okamoto S, et al. Differences in salivary alpha-amylase and cortisol responsiveness following exposure to electrical stimulation versus the Trier Social Stress Tests. PLoS One. 2012;7(7):e39375. doi: 10.1371/journal.pone.0039375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buchanan TW, Bibas D, Adolphs R. Salivary α-amylase levels as a biomarker of experienced fear. Commun Integr Biol. 2010;3(6):525–27. doi: 10.4161/cib.3.6.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosch JA, Brand HS, Ligtenberg TJ, et al. Psychological stress as a determinant of protein levels and salivary-induced aggregation of Streptococcus gordonii in human whole saliva. Psychosom Med. 1996;58(4):374–82. doi: 10.1097/00006842-199607000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Jirakul-somchok D, Roysommut S, Wannanon P, et al. Renal physiology, electolytes and acid-base disorders. 4th ed. Khon Kaen: Klung Nana Wittaya Press; 2011. [Google Scholar]
- 15.Eiam-ong S, Praditpornsilpa K, Sitthisook S. Renin-angiotensin-aldosterone system inhibitor. Bankok: Text and Journal; 2008. [Google Scholar]
- 16.Hodgson NA, Lafferty D. Reflexology versus Swedish massage to reduce physiologic stress and pain and improve mood in nursing home residents with cancer: A pilot trial. Evid Based Complement Alternat Med. 2012;2012 doi: 10.1155/2012/456897. Article ID 456897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thanakiatpinyo T, Suwannatrai S, Suwannatrai U, et al. The efficacy of traditional Thai massage in decreasing spasticity in elderly stroke patients. Clin Interv Aging. 2014;9:1311–9. doi: 10.2147/CIA.S66416. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang W, Takahashi S, Miki T, et al. A pilot study exploring the effects of reflexology on cold intolerance. J Acupunct Meridian Stud. 2010;3(1):43–48. doi: 10.1016/S2005-2901(10)60007-6. [DOI] [PubMed] [Google Scholar]
- 19.Hinds T, McEwan I, Perkes J, et al. Effects of massage on limb and skin blood flow after quadriceps exercise. Med Sci Sports Exerc. 2004;36(8):1308–13. doi: 10.1249/01.mss.0000135789.47716.db. [DOI] [PubMed] [Google Scholar]
- 20.Mori H, Ohsawa H, Tanaka TH, et al. Effect of massage on blood flow and muscle fatigue following isometric lumbar exercise. Med Sci Monit. 2004;10(5):CR173–78. [PubMed] [Google Scholar]
- 21.Kunikata H, Watanabe K, Miyoshi M, et al. The effects measurement of hand massage by the autonomic activity and psychological indicators. J Med Invest. 2012;59(1–2):206–12. doi: 10.2152/jmi.59.206. [DOI] [PubMed] [Google Scholar]
- 22.Buttagat V, Eungpinichpong W, Chatchawan U, et al. The immediate effects of traditional Thai massage on heart rate variability and stress-related parameters in patients with back pain associated with myofascial trigger points. J Bodyw Mov Ther. 2011;15(1):15–23. doi: 10.1016/j.jbmt.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 23.Castro-Sánchez AM, Matarán-Peñarrocha GA, Granero-Molina J, et al. Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. 2011;2011 doi: 10.1155/2011/561753. Article ID 561753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sherman KJ, Ludman EJ, Cook AJ, et al. Effectiveness of therapeutic massage for generalized anxiety disorder: a randomized controlled trial. Depress Anxiety. 2010;27(5):441–50. doi: 10.1002/da.20671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sudmeier I, Bodner G, Egger I, et al. Changes of renal blood flow during organ-associated foot reflexology measured by color Doppler sonography. Forsch Komplementarmed. 1999;6(3):129–34. doi: 10.1159/000021238. [DOI] [PubMed] [Google Scholar]
- 26.Lindgren L, Rundgren S, Winsö O, et al. Physiological responses to touch massage in healthy volunteers. Auton Neurosci. 2010;158(1–2):105–10. doi: 10.1016/j.autneu.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 27.Pishbin T, Firoozabadi SM, Jafarnia Dabanlo N, et al. Effect of physical contact (Hand-Holding) on heart rate variability. Int J Adv Comput Sci. 2012;2(12):452–56. [Google Scholar]
- 28.Lee YH, Park BN, Kim SH. The effects of heat and massage application on autonomic nervous system. Yonsei Med J. 2011;52(6):982–89. doi: 10.3349/ymj.2011.52.6.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35(3):235–56. doi: 10.2165/00007256-200535030-00004. [DOI] [PubMed] [Google Scholar]
- 30.Goldstein DS, Bentho O, Park MY, et al. Lowfrequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp Physiol. 2011;96:1255–61. doi: 10.1113/expphysiol.2010.056259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rahman F, Pechnik S, Gross D, et al. Low frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Clin Auton Res. 2011;21:133–41. doi: 10.1007/s10286-010-0098-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eungpinichpong W. Therapeutic thai massage. Bankok: Suweeriyasarn Printing Press; 2008. [Google Scholar]


