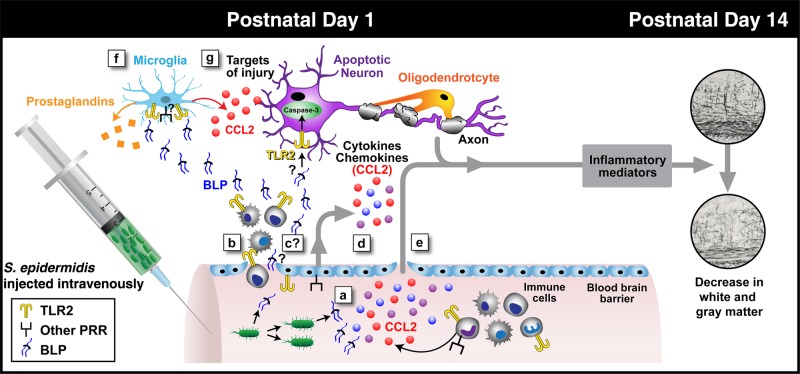
Figure 7.
Schematic diagram of possible steps leading to brain injury after initiation of Staphylococcus epidermidis bacteremia in mice on postnatal day 1 (PND1). The current study, interpreted in the context of published literature, suggests that S. epidermidis bacteremia at PND1 can trigger inflammation in both the bloodstream and central nervous system (CNS) that culminates in brain injury without entry of bacteria into the cerebrospinal fluid (CSF). Injection of S. epidermidis results in early (within 6 hours) generation of systemic cytokines in the bloodstream via both Toll-like receptor 2 (TLR2; yellow dimers) and other pattern-recognition receptors (PRRs; generically depicted as black/square receptors; a), associated entry into the CNS of white blood cells (WBCs; b), potential entry of dead bacteria and/or bacterial products such as bacterial lipoproteins (BLPs) into the CNS (this is under question, given the lack of direct evidence in the literature; c), potential entry of endothelium-derived cytokines (d) and/or systemic cytokines (e) into the CNS, and potential local (brain) generation of inflammatory mediators (eg, CCL2 detected in blood and brain and prostaglandins synthesized by the enzyme PTGS2, which was upregulated in the brain at the RNA level; f), culminating in early (within 6 hours) TLR2-dependent caspase-3 activation and late (PND14) brain injury (g), which can occur in a TLR2-independent manner that manifests as reduced gray and white matter volume.