Abstract
To determine the incidence and risk factors of retinopathy of prematurity (ROP) among new-born Chinese infants of multiple gestations.
A retrospective review of medical records was performed for all neonates of multiple gestations screened for ROP between January 2007 and December 2012 in 2 neonatal intensive care units in Hong Kong. Screening was offered to very low birth weight (VLBW; ≤1500 g) and/or preterm (gestation ≤32 weeks) neonates using the Royal College of Ophthalmologists ROP guideline and the International Classification of ROP by 3 pediatric ophthalmologists. Maternal and neonatal covariates were analyzed using univariate and multivariate regression analyses for both ROP and Type 1 ROP.
A total of 153 Chinese infants of multiple gestations were included in the study. The mean gestational age (GA) was 30.8 ± 2.4 weeks and the mean birth weight (BW) was 1284.8 ± 267.4 g. The incidence of ROP and Type 1 ROP was 11.8% and 3.9%, respectively. On univariate analysis, younger GA, lighter birth weight, postnatal hypotension, inotropes use, bronchopulmonary disease, and intraventricular hemorrhage were common independent risk factors for the development of ROP and Type 1 ROP (all P ≤ 0.04). On multivariate analysis, younger GA, surfactant use, invasive mechanical ventilation, higher mean oxygen concentration, thrombocytopenia, intraventricular hemorrahage, total parental nutrition, and hypoglycemia were significant risk factors for ROP. For Type 1 ROP, there were no significant dependent risk factors.
In preterm Chinese infants born from multiple gestations, prematurity, lighter weight, postnatal hypotension, inotropes use, bronchopulmonary dysplasia, and an intraventricular hemorrhage were common independent risk factors for the development of ROP and Type 1 ROP.
INTRODUCTION
Retinopathy of prematurity (ROP) is a vaso-proliferative retinal disease targeting low birth weight, preterm neonates.1 ROP is one of the leading causes of childhood blindness worldwide.2 Over the last decades, there has been a dramatic increase in the rate of multiple gestation possibly related to the increased use of assisted reproduction in those with advanced maternal age, infertility, or subfertility.3,5–7 Previous studies showed that multiple gestation is related to low birth weight and preterm delivery.4,6,8 However, the association of multiple gestation with ROP development is still controversial. Bossie et al found that multiple births are associated with higher risk of ROP compared to singleton while others have demonstrated the same or even lower risk of severe ROP in newborns of multiple gestations.9–15 Literature in this area is particularly lacking for the Chinese population. Thus, aim of this study was to analyze the potential risk factors for the development of ROP and Type 1 ROP in Chinese newborns belonging to multiple gestations.
PATIENTS AND METHODS
The study was approved by the institutional review board of the Hospital Authority of Hong Kong. The study was conducted in accordance with the Declaration of Helsinki, and no patient personal data were disclosed in the study. The authors declare no financial or proprietary interests. This was a nonfunded study.
This was a retrospective study conducted at Caritas Medical Centre, Hong Kong Special Administrative Region, China, which provides ophthalmological service to 2 Neonatal Intensive Care Units (NICU) for a population of 1.8 million. Parts of the methodology of this study have been described in early publications by the same authors.16–18
Medical records for consecutive newborns from multiple gestations that were screened for ROP between January 2007 and December 2012 were retrieved using the Clinical Data Record System of the Hospital Authority of Hong Kong.
ROP SCREENING CRITERION
The criterion for ROP screening was previously described in early publications by the same authors.16–18 All preterm babies admitted to these 2 NICUs with a birth weight (BW) ≤1500 g and/or gestational age (GA) ≤32 weeks were referred to a pediatric ophthalmologist for evaluation. All eligible preterms were examined according to the screening protocol recommended by the Royal College of Ophthalmologists and United Kingdom-ROP (UK-ROP) guidelines.19,20 Subjects were first screened at 4 to 8 weeks of postnatal age (≥30 week GA) and were examined weekly to bi-weekly, until retinal vascularization reached zone 3 or feature of established ROP regression.19 Treatment of diode laser was implemented when the disease progressed to Type 1 ROP as per the early treatment for retinopathy of prematurity (ETROP) study.21 The staging of ROP was recorded according to the revised International Classification of ROP, including the extent, zone, and the presence or absence of “plus” disease.19
All examinations were performed by 3 experienced pediatric ophthalmologists (SKY, TYT, and CYC). Each infant was screened by an indirect ophthalmoscope using a 30-dioptre (D) lens after full pharmacological pupil dilatation with tropicamide 0.5% and phenylephrine 1% eye drops. A lid speculum with scleral indentation after topical anesthesia (amethocaine) was routinely used. All screening was performed under oxygen saturation monitoring, and the screening was temporarily withheld in the case of desaturations.
The inclusion criteria included all preterm Chinese infants of multiple pregnancies irrespective of their ultimate development of ROP or Type 1 ROP. Neonates with incomplete clinical data or those that were deceased before the completion of ROP screening were excluded.
Some of the clinical parameters used as the primary outcome measures in this study have been previously described in early publications by the same authors in investigating different infant subgroups.16–18The primary outcome measures included: the severity of ROP (the extent, zone, and presence or absence of “plus” disease) as well as the 34 risk factors (both maternal and neonatal) for the development of ROP as follows:
Antenatal Maternal Risk Factors
Maternal diseases: pre-eclampsia (PET), gestational diabetes mellitus (GDM)
In-vitro fertilization (IVF)
Use of antenatal steroid (ANS) (Table 1)
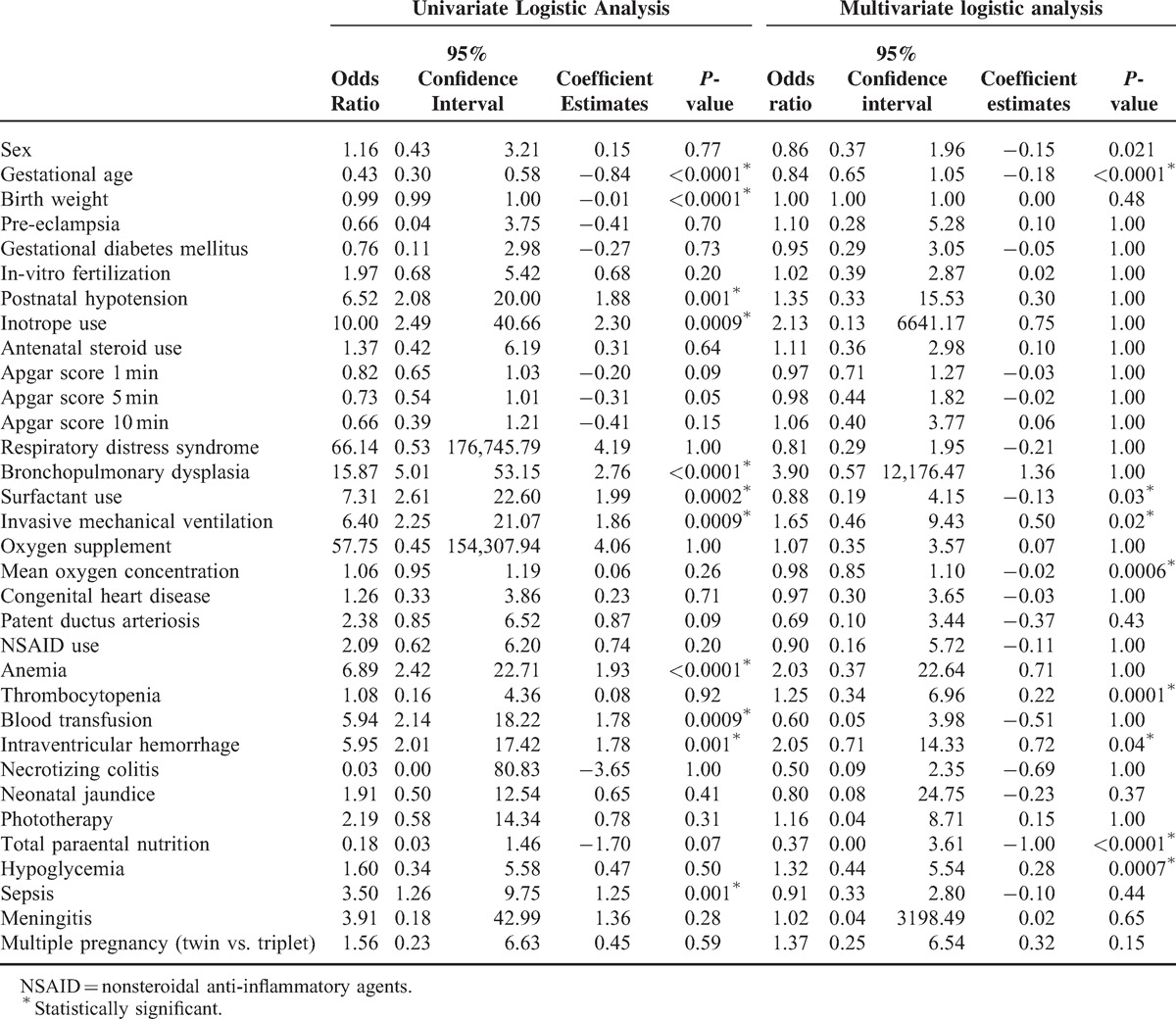
TABLE 1.
Univariate and Multivariate Analysis of Maternal and Natal Covariates for ROP Development in Preterm Infants of Multiple Gestations
Neonatal Risk Factors
Demographic information (GA, BW, gender)
Apgar scores at 1, 5, and 10 min
Postnatal interventions: surfactant administration; mechanical ventilation; use of supplementary oxygen; maintenance supplementary oxygen concentration (mean oxygen concentration); use of nonsteroidal anti-inflammatory agents (NSAID) for patent ductus arteriosus (PDA) closure; blood transfusion; and total parental nutrition (TPN)
Neonatal diseases: respiratory distress syndrome (RDS); bronchopulmonary dysplasia; hypotension; congenital heart disease; PDA; anemia (defined as hemoglobin <110 g/l, hematocrit <25%); thrombocytopenia; neonatal jaundice (NNJ), phototherapy, intraventricular hemorrhage (IVH); necrotizing enterocolitis (NEC); hypoglycemia; sepsis (culture positive or use antibiotics for more than 7 days);and meningitis
Type of multiple pregnancy (twin versus triplets) (Table 1)
Statistical Analysis
The correlation of the 34 covariates with the development of ROP and Type 1 ROP were analyzed separately using univariate and multiple logistic regression analyses as implemented in the R Programming Language.22 Most of the covariates were either binary or continuous. The responses and the nonresponses in the data were completely separated by predicators. Owing to the phenomenon of separation as described by Heinze and Schemper,23 the penalized maximum likelihood estimation method was implemented to reduce bias for related parameters as described by both Firth et al and Heinze et al.24,25A stepwise forward selection was used for choosing covariates for the multivariable analysis. Correlations were expressed in coefficients and odds ratio (OR) and a P-value less than 0.05 was considered as statistically significant. All means were expressed as mean ± standard deviation.
RESULTS
During the study period, a total of 168 preterm infants of multiple gestations were screened. Out of the 168 screened infants, 8 (4.8%) were non-Chinese ethnicity, 2 (1.2%) did not survive before completion of ROP screening and 5 (2.9%) had insufficient clinical information; these 15 (8.9%) cases were excluded. The remaining 153 eligible infants of multiple gestations were included for analysis (Figure 1).
FIGURE 1.
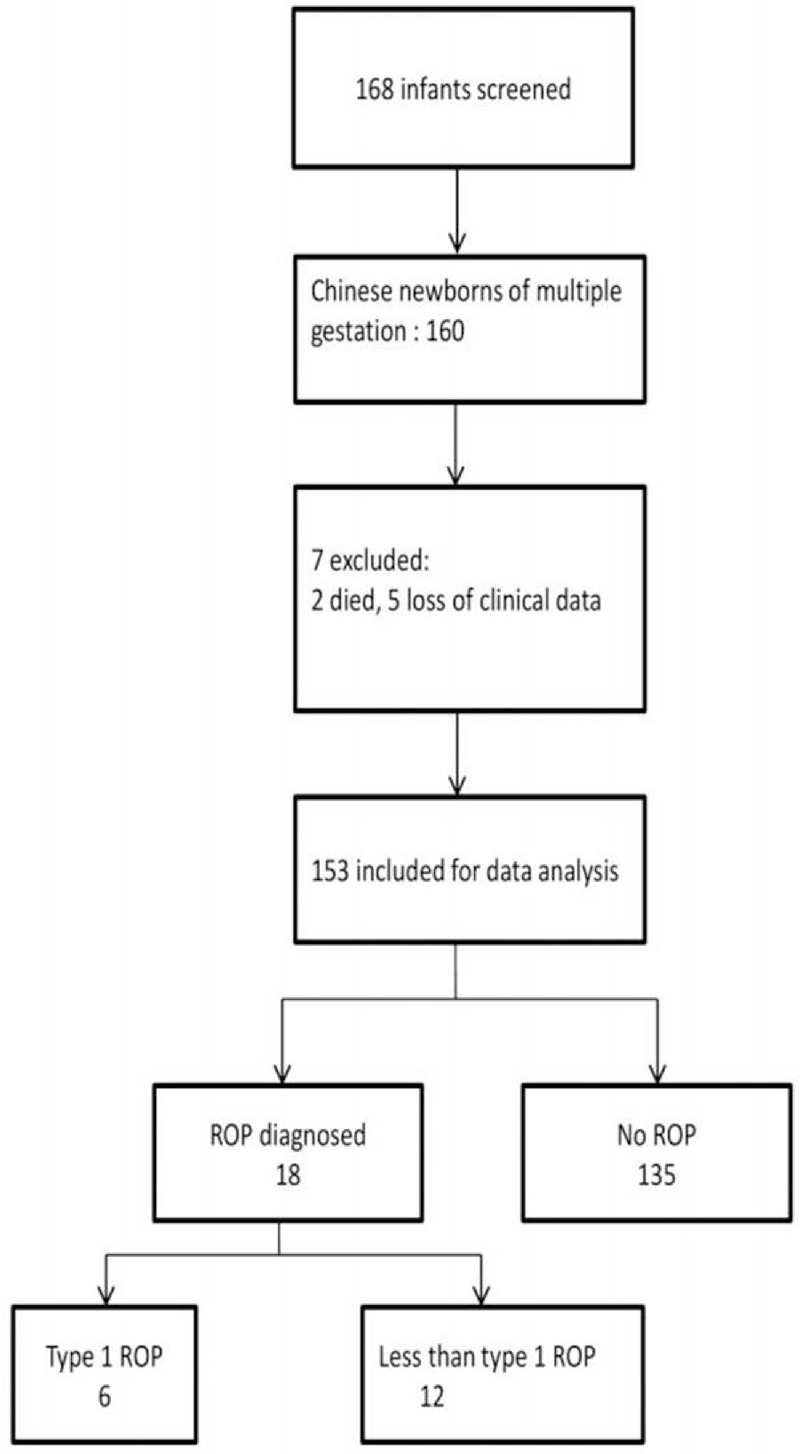
Schematic diagram of the distribution of infants belonging to multiple gestations.
DEMOGRAPHICS
Of these 153 infants included in the study, 141 (92.2%) were twins and 12 (7.8%) were triplets. Forty (26.1%) of the infants were born after IVF. All were of Chinese ethnicity. There were 80 male (52.3%) and 73 female (47.7%) subjects. The mean GA was 30.8 ± 2.4 weeks (range 24.0–36.3 weeks) and the mean BW was 1284.8 ± 267.4 g (range 470.0–2245.0 g). ROP of any stage developed in 18 infants (11.8%) and Type 1 ROP developed in 6 (3.9%) infants.
Risk Factors for ROP
Using univariate analysis, the following were significant independent risk factors for ROP development: lighter BW, younger GA, postnatal hypotension, inotropes use, bronchopulmonary dysplasia, surfactant use, invasive mechanical ventilation, higher mean oxygen concentration, anemia, blood transfusion, intraventricular hemorrhage, and sepsis (all P ≤ 0.001) (Table 1).
When using multivariate analysis, a smaller GA, surfactant use, invasive mechanical ventilation, higher mean oxygen concentration, thrombocytopenia, intraventricular hemorrhage, sepsis, total parental nutrition, and hypoglycemia were risk factors for ROP development (all P ≤ 0.04) (Table 1).
Risk Factors Type 1 ROP
Using univariate analysis, the following were significant independent risk factors for Type 1 ROP: a lighter BW, smaller GA, IVF, postnatal hypotension, inotropes use, bronchopulmonary dysplasia, and intraventricular hemorrhage (all P ≤ 0.04) (Table 2).
Table 2.
Univariate and Multivariate Analysis of Maternal and Natal Covariates for Type 1 ROP Development in Preterm Infants of Multiple Gestations
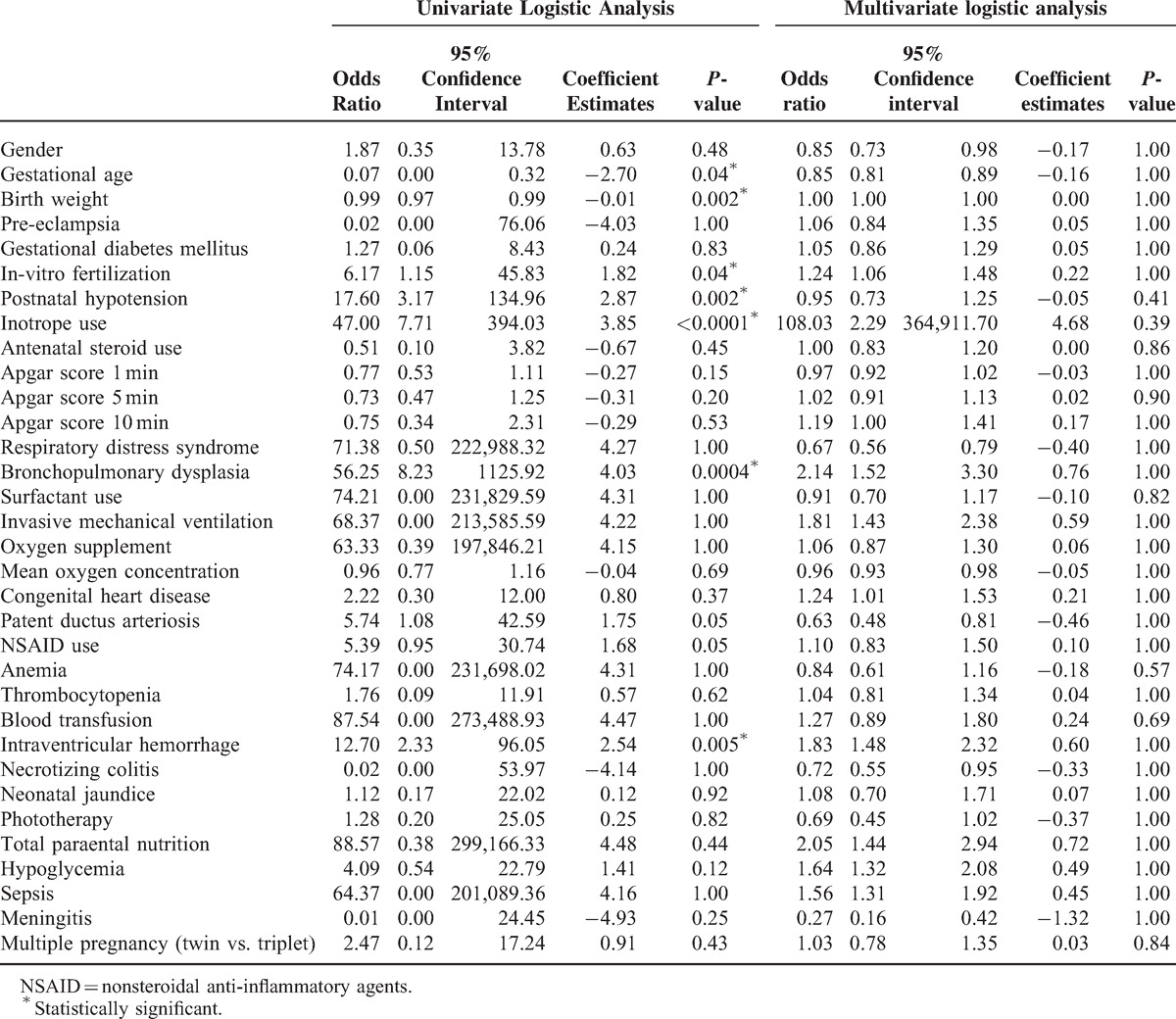
When using multivariate analysis, none of the covariates reached a level of statistical significance (Table 2).
DISCUSSION
The higher rate of perinatal mortality and morbidity among infants of multiple gestations has been shown to be related to a lower birth weight and more preterm delivery in this group of infants.4,11 The aim of this study was to explore the other maternal and neonatal associations for developing ROP and Type 1 ROP among preterm infants of multiple gestations in Chinese.
In our study, 26.1% of infants were born from IVF, which is similar to a series by Friling et al where 27.0 % of multiple pregnancies were products of IVF.25
While IVF is an effective for various causes of subfertility and infertility it also leads to higher risk of multiple pregnancies.26 From the univariate analysis, when compared to natural conception, IVF was identified as an independent risk factor for Type 1 ROP (OR = 6.17; CI: 1.15–45.83; P = 0.04). This was in agreement with Chan et al27 who has reported that assisted reproductive technology was associated with an increased risk of severe ROP requiring treatment (OR = 4.70, CI 1.52–14.57; P = 0.007). On the other hand, Friling et al reported that IVF was not a significant risk factor for ROP development nor a predictor for ROP severity.25
As reported by the Census and Statistics Department of Hong Kong, women nowadays have higher educational qualifications and more active participation in the work force, leading to more advanced maternal age during the delivery of their first child. The median maternal age for the first child was shifted by 4.9 years to 30.0 years of age in 2008 as compared to 1981. This may be one of the important reasons contributing to the increased infertility rates in Hong Kong and the greater reliance on assisted reproduction.28
Schaffer et al reported the association between threshold ROP and lighter birth weight, younger GA, multiple gestations, and Caucasian race in the Cryotherapy for Retinopathy of Prematurity Study.29 Younger GA and lower birth weight are likewise independent risk factors for Type 1 ROP in our population of infants born from multiple gestations. For ROP development, a younger GA, surfactant use, invasive mechanical ventilation, and intracranial hemorrhage were the 4 risk factors that were consistently significant on both univariable and multivariable analysis (all P ≤ 0.02).
To our best knowledge, this is the first study, reporting the incidence and risk factors of ROP and Type 1 ROP in Chinese infants born from multiple gestations. This study serves as a platform for future prospective and multicenter studies in this area as we anticipates that the number of IVF will likely continue to grow together with the number of preterm infants born from multiple gestations.
Our study had its limitations including inconsistencies in data due to the retrospective nature of the study and potential inter-observer variability from the different ROP screening ophthalmologists. To minimize the impact of these limitations, incomplete clinical data was excluded and the 3 screening pediatric ophthalmologists followed a strict ROP screening guideline. Nevertheless, this study implements the use of more updated and stricter ROP screening guidelines in providing data on the incidence and risk factors of ROP in the preterm Chinese infants born from multiple gestations. The findings from this study, however, may not be generalizable for other populations.
CONCLUSION
In preterm Chinese infants born from multiple gestations, prematurity, lighter weight, postnatal hypotension, inotropes use, brochopulmonary dysplasia, and intraventicular hemorrhage were common independent risk factors for the development of ROP and Type 1 ROP.
Footnotes
Abbreviations: BW = body weight, ETROP = early treatment for retinopathy of prematurity, GA = gestational age, IVF = in-vitro fertilization, IVH = intraventricular haemorrhage, NEC = necrotizing enterocolitis, NNJ = neonatal jaundice, NSAID = nonsteroidal anti-inflammatory agents, PDA = patent ductus arteriosis, RDS = respiratory distress syndrome, ROP = retinopathy of prematurity, TPN = total parental nutrition, VLBW = very low birth weight.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Terry TL. Retrolental fibroplasia in premature infants. Further studies on fibrolastic overgrowth of tunica vasculosa lentis. Arch Ophthalmol 1945; 33:203–208. [PMC free article] [PubMed] [Google Scholar]
- 2.Steinkuller PG, Du L, Gilbert C, et al. Childhood blindness. J AAPOS 1999; 3:26–32. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Contribution of assisted reproduction technology and ovulation—inducing drugs to triplet and higher-order multiple births—United States, 1980–1997. JAMA 2000; 284:299–300. [PubMed] [Google Scholar]
- 4.Barr S, Poggi S, Keszler M. Triplet morbidity and mortality in a large case series. J Perinatol 2003; 23:368–371. [DOI] [PubMed] [Google Scholar]
- 5.Oleszczuk JJ, Keith DM, Keith LG, et al. Projections of population-based twinning rates through the year 2100. J Reprod Med 1999; 44:913–921. [PubMed] [Google Scholar]
- 6.Kaufman GE, Malone FD, Harvey-Wilkes KB, et al. Neonatal morbidity and mortality associated with triplet pregnancy. Obstet Gynecol 1998; 91:342–348. [DOI] [PubMed] [Google Scholar]
- 7.Keith LG, Oleszczuk JJ, Keith DM. Multiple gestation: reflections on epidemiology, causes, and consequences. Int J Fertil Womens Med 2000; 45:206–214. [PubMed] [Google Scholar]
- 8.Luke B. The changing pattern of multiple births in the United States: maternal and infant characteristics, 1973 and 1990. Obstet Gynecol 1994; 84:10l–16l. [PubMed] [Google Scholar]
- 9.MRC Working Party on children conceived by in-vitro fertilization. Births in Great Britain resulting from assisted conception, 1978–1987. BMJ 1990; 300:1229–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dos Santos Motta MM, Fortes Filho JB, Coblentz J, et al. Multiple pregnancies and its relationship with the development of retinopathy of prematurity (ROP). Clin Ophthalmol 2011; 5:1783–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friling R, Rosen SD, Monos T, et al. Retinopathy of prematurity in multiple-gestation, very low birth weight infants. J Pediatr Ophthalmol Strabismus 1997; 34:96–100. [DOI] [PubMed] [Google Scholar]
- 12.Blumenfeld LC, Siatkowski RM, Johnson RA, et al. Retinopathy of prematurity in multiple-gestation pregnancies. Am J Ophthalmol 1998; 125:197–203. [DOI] [PubMed] [Google Scholar]
- 13.Kaufman GE, Malone FD, Harvey-Wilkes KB, et al. Neonatal morbidity and mortality associated with triplet pregnancy. Obstet Gynecol 1998; 91:342–348. [DOI] [PubMed] [Google Scholar]
- 14.Watts P, Adams GG. In vitro fertilisation and stage 3 retinopathy of prematurity. Eye (Lond) 2000; 14:330–333. [DOI] [PubMed] [Google Scholar]
- 15.Bossi E, Koerner F. Influence of statistical methodology and composition of patient populations on the correlation of risk factors with retinopathy of prematurity. Ocular Circ Neovasc 1987; 141–146.(Documenta Ophthalmologica Proceedings Series Volume 50). [Google Scholar]
- 16.Yau GSK, Lee JWY, Tam VTY, et al. Incidence and risk factors for retinopathy of prematurity in extreme low birth weight Chinese infants. Int Ophthalmol 2014; http://www.ncbi.nlm.nih.gov/pubmed/24898774 (DOI 10.1007/s10792-014-9956-2). [DOI] [PubMed] [Google Scholar]
- 17.Yau GSK, Lee JWY, Tam VTY, et al. Differences in risk factors for retinopathy of prematurity development in paired twins: a Chinese population study. Sci World J 2014; 10.1155/2014/212183Article ID 212183, 7 pages, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yau GSK, Lee JWY, Tam VTY, et al. Risk factors for retinopathy of prematurity in extreme preterm Chinese infants. Medicine (Baltimore) 2014; 93:e314. 10.1097/MD.0000000000000314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Royal College of Paediatrics and Child Health. Guideline for the Screening and Treatment of Retinopathy of Prematurity. 2013; 〈http://www.rcpch.ac.uk〉(accessed on November 2, 2013).. [Google Scholar]
- 20.The Royal College of Ophthalmologist; British Association of Perinatal Medicine. Report of a Joint Working Party. The Royal College of Ophthalmologist, British Association of Perinatal Medicine: Retinopathy of Prematurity: guidelines forscreening and treatment. Early Human Dev 1996; 46:239–258. [PubMed] [Google Scholar]
- 21.Early Treatment for Retinopathy of Prematurity Cooperative G. Revised indications for the treatment of retinopathy of prematurity: Results of the Early Treatment for Retinopathy of Prematurity randomized trial. Arch Ophthalmol 2003; 121:1684–1694. [DOI] [PubMed] [Google Scholar]
- 22.R Core Team. R: a language and environment for statistical computing. 2014; Vienna, Austria: R Foundation for Statistical Computing, 〈http://www.R-project.org/〉 (accessed May 18, 2014). [Google Scholar]
- 23.Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med 2002; 21:2409–2419. [DOI] [PubMed] [Google Scholar]
- 24.Heinze G, Meinhard P, Dunkler D, et al. logistf: Firth's bias reduced logistic regression. R package version 1.21 2013; 〈http://CRAN.R-project.org/package=logistf〉 (accessed May 18, 2014). [Google Scholar]
- 25.Friling R, Axer-Siegel R, Hersocovici Z, et al. Retinopathy of prematurity in assisted versus natural conception and singleton versus multiple births. Ophthalmology 2007; 114:321–324. [DOI] [PubMed] [Google Scholar]
- 26.Chai J, Yeung TW, Lee VC, et al. Live birth rate, multiple pregnancy rate, and obstetric outcomes of elective single and double embryo transfers: Hong Kong experience. Hong Kong Med J 2014; 20:102–106. 10.12809/hkmj134065 [DOI] [PubMed] [Google Scholar]
- 27.Chan RV, Yonekawa Y, Morrison MA, et al. Association between assisted reproductive technology and advanced retinopathy of prematurity. Clin Ophthalmol 2010; 4:1385–1390. 10.2147/OPTH.S15587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Census and Statistics Department. Demographic trends in Hong Kong 1981–2011. 2014; Hong Kong Special Administrative Region: Census and Statistics Department, 〈http://www.statistics.gov.hk/pub/B1120017032012XXXXB0100.pdf〉 (accessed on April 29, 2014). [Google Scholar]
- 29.Schaffer DB, Palmer EA, Plotsky DF, et al. Prognostic factors in the natural course of retinopathy of prematurity. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology 1993; 100:230–237. [DOI] [PubMed] [Google Scholar]


