Abstract
Transpedicular screw (TPS) fixation in unstable thoracic and lumbar (TL) spine fractures remains technically difficult because of destroyed anatomical landmarks, unstable gross segments, and discrepancies in anatomic orientation using conventional anatomic landmarks, fluoroscopic guidance, or computed tomography (CT)-based navigation. In this study, we evaluated the safety and accuracy of TPS placement under intraoperative computed tomography (iCT) navigation in managing unstable TL spine fractures.
From 2010 to 2013, we retrospectively reviewed the Spine Operation Registry records of patients who underwent posterior instrumented fusion to treat unstable TL spine fractures via the iCT navigation system. An unstable spine fracture was identified as AO/Magerl classification type B or type C.
In all, 316 screws in 37 patients with unstable TL spine fractures were evaluated and involved 7 thoracic, 23 thoracolumbar junctional, and 7 lumbar fractures. The accuracy of TPS positioning in the pedicle without breach was 98% (310/316). The average number of iCT scans per patient was 2.1 (range 2–3). The average total radiation dose to patients was 15.8 mSv; the dose per single level exposure was 2.7 mSv. The TPS intraoperative revision rate was 0.6% (2/316) and no neurovascular sequela was observed. TPS fixation using the iCT navigation system obtained a 98% accuracy in stabilizing unstable TL spine fractures. A malplaced TPS could be revised during real-time confirmation of the TPS position, and no secondary operation was required to revise malplaced screws.
The iCT navigation system provides accurate and safe management of unstable TL spine fractures. In addition, operating room personnel, including surgeons and nurses, did not need to wear heavy lead aprons as they were not exposed to radiation.
INTRODUCTION
Image-guided navigation using 2-dimensional (2-D) fluoroscopic guidance, 3-dimensional (3-D) fluoroscopic navigation, and computed tomography (CT)-based navigation have shown high accuracy and increased safety in transpedicular screw (TPS) insertion for various spine disorders.1 According to Magerl classification, unstable spinal fractures include distraction (type B) or torsion injuries (type C), which lead to the destruction of posterior elements as well as to the anterior column.2 Posterior instrumentation with TPS placement becomes more technically difficult; however, when using conventional methods such as anatomic landmarks, the open laminar approach, and fluoroscopic assistance because unstable thoracic and lumbar (TL) spine fractures often include the destruction of the posterior elements such as the lamina and facets, as well as pedicle fractures. However, few studies have focused on the integration of CT-based navigation with TPS fixation for unstable TL spine fractures. Gross segmental instability in spine fractures leads to discrepancies in anatomic orientation during the change in patients’ positioning between preoperative CT scanning and intraoperative surgical navigation, which reduces the accuracy of TPS fixation.
Intraoperative computed tomography (iCT) navigation provides real-time 3-D images, which can be acquired after the well-prepared surgical field of posterior spinal elements is scanned by the iCT, eliminating anatomic discrepancies related to the patients’ changing position. In this study, we utilized the iCT navigation system to guide TPS fixation in the treatment of unstable TL spine fractures and evaluated the safety and accuracy of TPS placement.
METHODS
Patients
Institutional Review Board Approval for this study was obtained from the Ethics Committee and Institutional Review Board of the authors’ institution (No. 102-5254B).
From 2010 to 2013, we performed a retrospective review of records of the Spine Operation Registry at the authors’ institution to identify patients who underwent posterior instrumented fusion to treat unstable TL spine fractures via the iCT navigation system. The inclusion criterion involved type B or type C injury using the AO/Magerl classification. Type A injuries (vertebral body compression injuries) were excluded.
Patients with suspected spine injuries presented through the emergency department and met the Advanced Trauma Life Support guidelines. A trauma X-ray series was performed. When chest or abdominal blunt trauma occurred, a CT scan of chest, abdomen, or pelvis was performed. Magnetic resonance imaging was obtained after diagnostic plain films of the affected region of the spine were completed. Emergent surgical decompression followed by posterior instrumented fusion was performed when a patient sustained a spinal cord injury or had cauda equina syndrome, and early surgical fixation within 72 hours was performed in patients with normal neural function and stable medical condition.
Surgical Technique
Surgical treatment included posterior instrumentation with pedicle screws and rods, and posterior/posterolateral fusion with or without decompressive laminectomy. Placement of pedicle screws was assisted by an iCT navigation system (Spine & Trauma iCT; BrainLab AG, Feldkirchen, Germany). The navigation system was composed of a sliding gantry 24-slice CT scanner (Somatom Sensation Open, Siemens Healthcare, Forchheim, Germany) and a frameless infrared-based navigation workstation (BrainLab, VectorVision sky; BrainLab AG, Feldkirchen, Germany). The patient was placed in the prone position on the Jackson table by the log-rolling maneuver after general anesthesia with intubation was completed. A posterior midline incision with paraspinal muscle stripping was performed to expose the posterior elements of the affected spinal region. A reference array was securely fixed to the selected stable vertebra intended for instrumentation by tightly clamping the cortical bone of the spinous process. The stable vertebra (to which a reference array was clamped) was selected either cranially or caudally adjacent to the fractured vertebrae. Over-tight clamping and interspinous placement of the reference array should be avoided to prevent fracture of the spinous process and unstable reference fixation. The reference array was then gently pulled on to check that fixation was secure before a registration CT scan was performed.
Images from the registration CT scan were transferred to the navigation workstation. After the accuracy of the registration was confirmed by verifying the targeted bony landmarks, the CT image was used to guide screw insertion. A drill guide with a 2.7 mm-diameter drill bit was tracked, and the drilling length was adjusted to 35 mm for lumbar vertebrae and to 25 mm for thoracic vertebrae. After the entry point was identified by the register pointer and prepared with a cylindrical burr, the surgeon used the drill guide on the prepared entry point, checking the accuracy of the trajectory through the axial, sagittal, and coronal views displayed by the navigation system. At the same time, the length, and diameter of a pedicular screw were measured under iCT navigation. The length of the screw was selected from the entry point to inner wall of the vertebral anterior cortex. The diameter of the screw is selected to be as large as possible according to the simulated TPS fitting into the pedicle using the iCT navigation system (Figure 1). The transpedicular track tunnel was prepared via drilling through the trajectory-selected drill guide. The surgeon checked the prepared screw hole with a ball-tipped probe. A length/diameter-appropriate pedicular screw was then placed into the prepared transpedicular track tunnel. A confirmation CT scan was immediately performed after all pedicular screws were placed (Figures 2 and 3).
FIGURE 1.
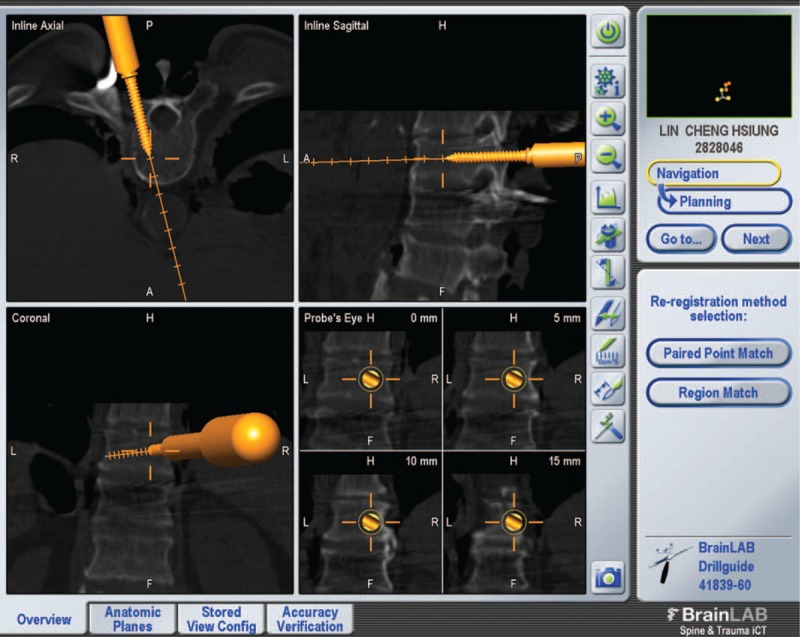
The diameter of the screw is selected to be as large as possible according to the simulated TPS fitting into the pedicle using the iCT navigation system. iCT = intraoperative computed tomography, TPS = transpedicular screw.
FIGURE 2.
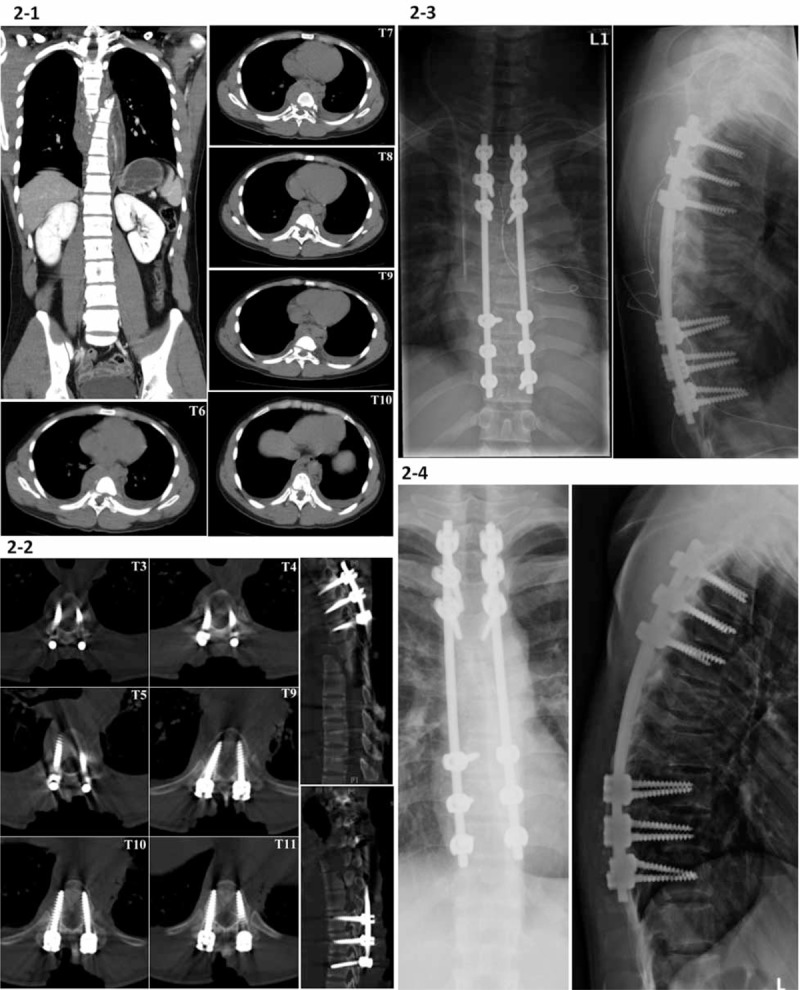
A 23-year-old male patient sustained a complete fracture-dislocation of T6 to T10 (AO type C1) with spontaneous neurological decompression. (2-1) The preoperative chest and abdominal CT images were obtained at a regional hospital. We performed posterior instrumentation of T3 to T9 using TPS fixation under iCT navigation, except for the excessively displaced T6 to T8 vertebral bodies. (2-2) A confirmation CT scan shows good positioning of all pedicle screws. The posterior laminae from T3 to T9 were decorticated and fused with autogenous iliac cancellous bone graft and bone graft substitutes. (2-3) The postoperative radiographs show posterior instrumentation of T3 to T9 for the complete fracture-dislocation of T6 to T10. (2-4) Radiographs demonstrate good stability of the affected thoracic spine without kyphotic change or implant failure at 1-year follow-up. CT = computed tomography, iCT = intraoperative computed tomography, TPS = transpedicular screw.
FIGURE 3.
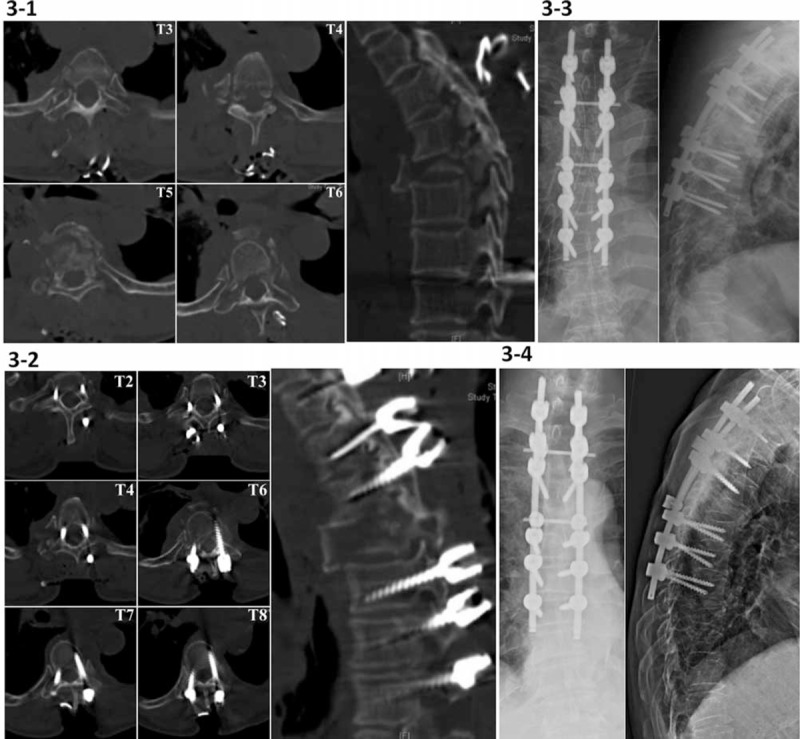
(3-1) Intraoperative spinal CT scan shows a fracture-distraction and torsion injury of T5 and multiple rib fractures and bilateral pedicle and lamina fractures involving T3 to T6 (AO type C2) in a 70-year-old female patient with ASIA grade C. TPS fixation 3 levels above and below the T5 level is guided under the iCT navigation. (3-2) The confirmation CT scan shows a grade I lateral cortical breach of right T3 TPS (1.3 mm), which did not require revision due to an acceptable screw position. After a decompression laminectomy at the T5 level, autogenous bone chips and bone substitutes were placed on the decorticated laminae from T2 to T8 for posterior fusion. (3-3) The postoperative radiographs show posterior instrumentation of T2 to T8 for the complete fracture-distraction of T3 to T6. (3-4) There is no kyphotic collapse at the 1-year follow-up radiographic examination. ASIA = American Spinal Injury Association, CT = computed tomography, iCT = intraoperative computed tomography, TPS = transpedicular screw.
Intraoperative assessment of TPS position was accomplished using the confirmation CT scan by any 2 spine surgeons (CYL, TJH, YYL, CCC, and MHW) and the intraoperative radiologic technician (CHH), and an acceptable screw position was defined as cortical breach of less than or equal to 2 mm.3–5 A misplaced pedicular screw could be corrected when cortical breach of the pedicle was more than 2 mm as measured by confirmation CT images. Then, CT scanning for the corrected level was immediately performed to ensure that the replaced screw was in an appropriate position (Figure 4). After insertion of all pedicular screws was completed, laminectomy was then carried out for the decompression of the affected neural elements if neurologic deficit was preoperatively examined. Thoracic posterior fusion or lumbar posterolateral fusion with autogenous bone chips and bone substitutes was performed.
FIGURE 4.

(4-1) Preoperative radiographs show a Chance fracture of T12 (AO type B2) in a 72-year-old male patient. (4-2) A confirmation CT scan demonstrates grade II lateral cortical breach of the right T9 pedicular screw (3.5 mm) after TPS fixation of T9-L. (4-3) A postrevision CT scan of T9 shows the position of the revised screw. CT = computed tomography, TPS = transpedicular screw.
Data Assessment
Medical records and collected data were reviewed for neurological status, thoracolumbar injury classification system (TLICS) scores,6 estimated blood loss, operative time, and number of iCT scans. Neurological status was evaluated preoperatively and postoperatively using the American Spinal Injury Association (ASIA) standards.7 ASIA grade (A to E) was converted into a numerical score (1–5) for statistical analysis. The TL spine fracture morphology was classified according to AO/Magerl Spine classification.2
In this study, the effective dose of radiation exposure for each patient was calculated from the dose length product (DLP) using a conversion factor of 0.018 (which was the DLP average of 0.019 for the chest and 0.017 for the abdomen).8–10 The pedicular screw position was classified into 4 grades: grade 0, screw in the pedicle without cortical breach; grade 1, cortical breach <2 mm; grade 2, cortical breach 2 to 4 mm; and grade 3, cortical breach >4 mm.3 The location of perforation was classified as medial, lateral, superior, or inferior to the pedicle.
RESULTS
Patient demographic data are summarized in Table 1. A total of 37 patients (average age, 60.1 years; range 23–75 years) with unstable TL spine fractures and an average follow-up period of 14.6 months (range 12–24 months) were included in this study. In all, 316 screws in 37 patients with unstable TL spine fractures were evaluated and included 7 thoracic, 23 thoracolumbar junctional, and 7 lumbar fractures. Patients had 28 AO type B fractures and 9 type C fractures.
TABLE 1.
Demographic Data
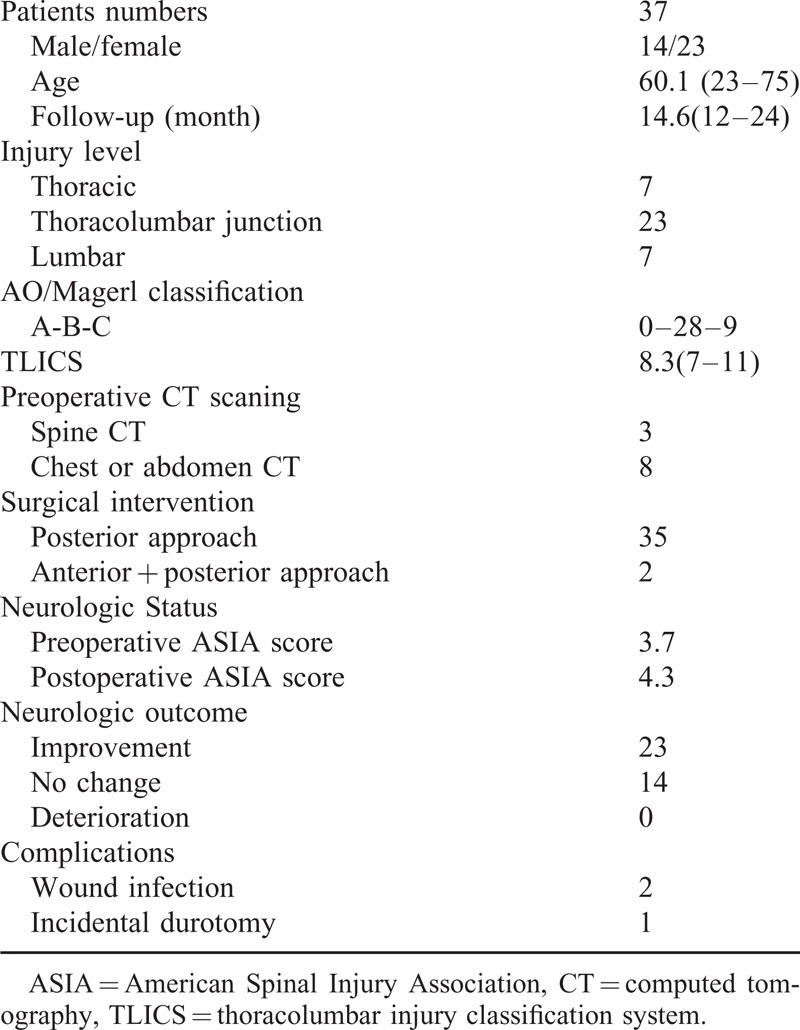
A preoperative CT scan was not routinely performed, except for 8 CT scans of the chest or abdomen performed for blunt chest or abdominal trauma, respectively, and 3 CT scans of the TL spine from outside facilities. The mean TLICS score was 8.3 (7–11). Single posterior surgery was performed in 35 patients and staged anterior reconstruction was performed in 2 patients 1 week after posterior instrumentation surgery. Twenty-three patients had postoperative neurological improvement of at least 1 ASIA grade, and none sustained postoperative neurological deterioration.
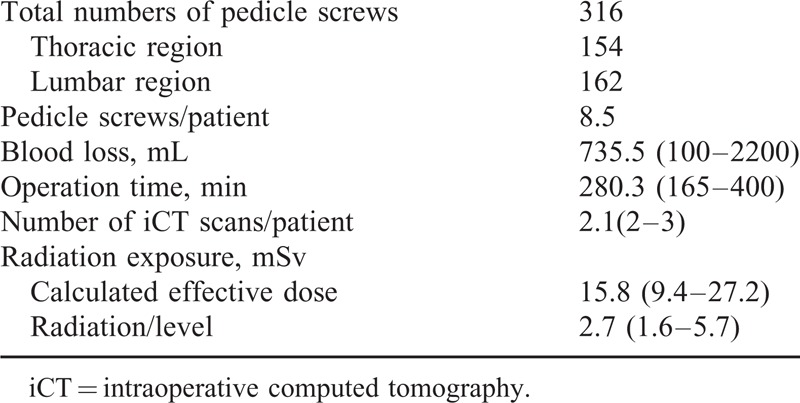
Intraoperative parameters are shown in Table 2. A total of 316 screws including 154 thoracic and 162 lumbar screws were placed. The mean estimated blood loss was 735.5 mL (range 100–2200 mL) and the average operative time was 280.3 min (range 165–400 min). Regardless of the number of instrumented levels within TL spine, only 2 CT scans, including 1 registration scan and 1 confirmation scan, were required. The mean number of iCT scans per patient was 2.1 (2–3). Most patients underwent 2 iCT scans including registration and confirmation scans except 2 patients who had an additional CT scan for a revised pedicular screw. The mean dose of patient radiation exposure was 15.8 mSv (range 9.4–27.2 mSv) and the mean radiation dose per single level exposure was 2.7 mSv (range 1.6–5.7 mSv).
TABLE 2.
Intraoperative Data
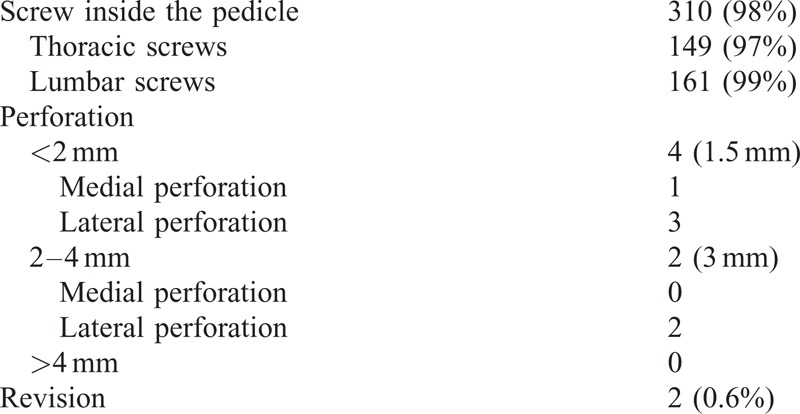
The accuracy of the TPS placement is summarized in Table 3. A total of 310 screws (98%) were positioned in the pedicle without cortical breach, including 149 thoracic screws (97%) and 161 lumbar screws (99%). Breach grade 1 occurred in 4 pedicle screws with an average breach distance of 1.5 mm, including 3 thoracic screws (all lateral breach) and 1 lumbar screw (medial breach). Breach grade 2 occurred in 2 thoracic pedicle screws with an average breach distance of 3 mm; both were lateral breach and revised. The TPS revision rate was 0.6% (2/316) without any neurovascular sequela. There was no superior or inferior breach.
TABLE 3.
Accuracy of Transpedicular Screw Insertion
DISCUSSION
In this study, the overall accuracy of TPS fixation under iCT navigation for the treatment of unstable TL spine fractures was 98%, including a 97% accuracy for thoracic and a 99% accuracy for lumbar TPS placement. Fisher et al5 reported that 68 screws (33.8%) violated the pedicle wall of 201 thoracic pedicle screws inserted with anatomic landmarks in the treatment of unstable thoracic fractures. Beck et al11 reported 78% accuracy of 414 screws inserted by reference to the dorsal anatomical structures and simultaneous fluoroscopic guidance in 95 patients with traumatic unstable fractures of the TL spine; 91 screws (22%) penetrated the pedicle walls. In another study of 40 patients with thoracic spinal fractures, 84 screws penetrated the pedicles up to 2 mm and 4 penetrated up to 3 mm in a total 204 thoracic pedicle screws using the conventional open technique, for a malpositioning rate of 43.1%.12
In spite of the gross segmental instability and disoriented anatomy associated with changing the patient's position when using CT-based navigation to treat unstable TL spinal fractures, Wang et al reported 96.4% accuracy of the TPS placement via CT-based navigation with separate reference clamp and registration.13 Compared to reports of accuracy of the TPS placement using conventional open technique or CT-based guidance of 56.9%, 66.2%, 78%, and 96.4%,5,11–13 the iCT navigation resulted in more precise positioning of TPS in unstable TL spinal fractures. In addition, the iCT navigation required only 1 registration for the selected spinal region, which may reduce contamination which can occur during separate reference clamp and repeat registration.
All navigation-guided techniques reduce the breach rate of TPS placement, but cannot eliminate the possibility of malpositioning. Intraoperative portable X-ray and image intensifier examinations such as fluoroscope and 3-D scan do not offer the same diagnosis of false TPS position as the CT scan. The false positioning of the TPS results in revision rates of 2.8–6.6%, which leads to a secondary operative revision.11,14 CT imaging has long been the gold standard for exact determination of TPS position.15 The iCT navigation system contains a CT station to provide an immediate confirmation CT scan to check TPS position. Although safe zones of reported medial cortical breach were less than 4 mm and reported lateral cortical perforation were less than 6 mm,16,17 we corrected any malplaced screw violating the cortex by more than 2 mm to avoid irritation of the neural elements and to enhance pull-out strength of the screws.3,18,19 In this study, the intraoperative correction rate was 0.6% and no secondary operation for revision was required. In a 2009 study of confirmation of the classification of TPS position using intraoperative 3-D scan and postoperative CT scan, the secondary operative revision rate was 2.1% due to 2.2% false classification of TPS position in intraoperative 3-D scanning.11 Hence, posterior instrumentation using iCT navigation to treat unstable TL spine fractures can provide a real-time confirmation of the TPS position and reduce the need for a secondary operation for revision of malplaced screws.
Radiation exposure in spine surgery under image-guided navigation is of great concern. The relevant advantages of the iCT navigation system and intraoperative 3-D fluoroscopic navigation are lack of radiation exposure to the surgeons or nurses and no need for bulky lead aprons for shielding. However, use of the iCT or intraoperative 3-D fluoroscopic navigation does expose the patient to a higher effective dose of radiation during the performance of 2 scans including registration and confirmation scans.
In this study, the average dose of radiation exposure to each patient was 15.8 mSv and the radiation dose per single level exposure was 2.7 mSv. The iCT navigation system involved no intraoperative fluoroscopic radiation exposure to patients and no postoperative CT scanning. From the literature, the radiation dose per single level exposure (2-pedicle insertion) of 2-D fluoroscopic guidance was estimated as 0.6 to 1.08 mSv.20,21 Bronsard et al22 reported that a total effective radiation dose of intraoperative fluoroscopy and postoperative CT scan in the conventional open TPS insertion and in the percutaneous TPS fixation was 10.5 and 12.2 mSv, respectively. Hence, compared to 2-D fluoroscopic guidance, the effective radiation dose to a patient was relatively higher in the iCT navigation system. However, the relevant advantages of the iCT navigation system are lack of radiation exposure to the surgeons or nurses and no need for bulky lead aprons for shielding.
According to published effective doses of radiation estimated by O’Donnell et al, the total effective dose to 5 vertebral segments from navigation and confirmation scans using 3-D fluoroscopic navigation (O-arm) was 14.58 mSv.23,24 Two-leveled TPS fixation above and below fractured levels is demanded in unstable TL spine fractures. Effective dose of radiation may be higher when using 3-D fluoroscopic navigation compared with the iCT navigation because 3 to 4 vertebral segments are visualized within 1 single scan of 3-D fluoroscopic navigation and more than 2 scans will be needed for multiple TL fractured levels. The CT-based navigation requires not only preoperative CT scanning but also intraoperative fluoroscopic assistance, especially when conducting a separate registration. In this study, it was unnecessary to obtain a preoperative CT scan of the affected spine, except for 3 patients who had spine CT scans before being transferred to our institute, and 8 patients who received chest or abdominal CT scans because of blunt chest or abdominal trauma. The annual maximum permissible dose, recommended by the International Commission on Radiological Protection (ICRP), is 50 mSv for the whole body, head, neck, trunk, eyes, bone marrow, and gonads.25 Hence, the radiation exposure of patients using the iCT navigation for TPS placement is within guidelines, because such patients would not require the additional radiation exposure of intra-operative fluoroscopy and postoperative CT scanning.
There were 3 main contributing factors that reduced navigation accuracy causing TPS misplacement under the iCT navigation, including mobilization of the reference frame, spine mobility between the frame and the instrumented vertebrae, and related technical problems. To eliminate mobilization of the reference frame, a reference array is fixed on the spinous process by clamping the cortical bone; putting traction on the reference frame by a suction tube or wires for cauterization is forbidden.26 Complete exposure of the surgical field with self-retaining skin retractor for TPS fixation should be performed before the CT registration scan because dissecting soft tissue and retracting the wound will result in the movement of the spinal anatomy. All of the transpedicular track tunnels on the instrumented vertebrae should be prepared by drilling under iCT navigation prior to TPS placement since navigational accuracy will be best immediately after CT registration and spine mobility may occur when a pedicle screw is inserted.
In this study, most of 6 malpositioned pedicle screws were lateral cortical breach (83%), including 2 revised screws. Although the transpedicular track tunnel was drilled with guidance from the iCT navigation system and was checked by a ball-tipped probe, the pedicle screw was driven into the prepared tunnel by the freehand method. Insertion of a pedicle screw tends to be deflected laterally away from the trajectory of the prepared transpedicular tunnel when the surgeon fears to violate the medial pedicular cortex and, thus, damage the spinal thecal sac. Hence, this bias would contribute to the finding that the majority of cortical breaches were lateral breaches in our study. In order to overcome this bias, we have started to integrate navigation in driving the pedicle screw with a reference attached to a screw driver, and so that the trajectory of the screw will be in accordance with that of the prepared transpedicular tunnel.
Our study had several limitations. First, the number of the patients was small because we have only integrated the iCT navigation system into spinal surgeries at our hospital since 2010. Second, since this study was a case series without the control groups, further studies are needed to analyze the different methods of image-guided navigation. Third, the establishment of the iCT navigation system requires considerable monetary investment and enough space for a CT scanner and a navigation workstation in the operating room. Finally, our short-term study could only provide immediate perioperative radiographic and neurologic data, and long-term results should be investigated in future studies.
CONCLUSIONS
TPS fixation using the iCT navigation system resulted in 98% accuracy in stabilizing unstable TL spine fractures. A malplaced TPS could be immediately corrected during real-time confirmation of the TPS position, and no secondary operation was required for revision of malplaced screws. The iCT navigation system provided an accurate and safe alternative for management of unstable TL spine fractures. In addition, the operating room personnel, including the surgeons and nurses, did not have to wear cumbersome lead aprons and were not exposed to radiation.
Acknowledgments
The authors thank the Research Committee of Chang Gung Memorial Hospital, Taiwan for assistance (No. CMRPG6A0211-2) in the Spine Operation Registry. The authors also thank Miss Yi-Fang Tsai for her assistance in statistical analyses and digital illustrations.
Footnotes
Abbreviations: ASIA = American Spinal Injury Association, CT = computed tomography, 2-D = two-dimensional, 3-D = three-dimensional, DLP = dose length product, iCT = intraoperative computed tomography, TL = thoracic and lumbar, TLICS = thoracolumbar injury classification system, TPS = transpedicular screw.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Tian NF, Xu HZ. Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop 2009; 33:895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 1994; 3:184–201. [DOI] [PubMed] [Google Scholar]
- 3.Belmont PJ, Jr, Klemme WR, Dhawan A, et al. In vivo accuracy of thoracic pedicle screws. Spine (Phila Pa 1976) 2001; 26:2340–2346. [DOI] [PubMed] [Google Scholar]
- 4.Belmont PJ, Jr, Klemme WR, Robinson M, et al. Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine (Phila Pa 1976) 2002; 27:1558–1566. [DOI] [PubMed] [Google Scholar]
- 5.Fisher CG, Sahajpal V, Keynan O, et al. Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine 2006; 5:520–526. [DOI] [PubMed] [Google Scholar]
- 6.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 2005; 30:2325–2333. [DOI] [PubMed] [Google Scholar]
- 7.Maynard FM, Jr, Bracken MB, Creasey G, et al. International standards for neurological and functional classification of spinal cord injury. Am Spinal Injury Assoc Spinal Cord 1997; 35:266–274. [DOI] [PubMed] [Google Scholar]
- 8.Bongartz G GS, Jurik AG, Leonardi M, et al. European guidelines for multislice computed tomography. Funded by the European Commission. March 2004;Contract number FIGMCT2000-20078-CT-TIP. [Google Scholar]
- 9.Abul-Kasim K. Low-dose spine CT: optimisation and clinical implementation. Radiat Prot Dosimetry 2010; 139:169–172. [DOI] [PubMed] [Google Scholar]
- 10.Abul-Kasim K, Overgaard A, Maly P, et al. Low-dose helical computed tomography (CT) in the perioperative workup of adolescent idiopathic scoliosis. Eur Radiol 2009; 19:610–618. [DOI] [PubMed] [Google Scholar]
- 11.Beck M, Mittlmeier T, Gierer P, et al. Benefit and accuracy of intraoperative 3D-imaging after pedicle screw placement: a prospective study in stabilizing thoracolumbar fractures. Eur Spine J 2009; 18:1469–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beck M, Rotter R, Gradl G, et al. Reliability and consequences of intraoperative 3D imaging to control positions of thoracic pedicle screws. Arch Orthop Trauma Surg 2012; 132:1371–1377. [DOI] [PubMed] [Google Scholar]
- 13.Wang HC, Yang YL, Lin WC, et al. Computer-assisted pedicle screw placement for thoracolumbar spine fracture with separate spinal reference clamp placement and registration. Surg Neurol 2008; 69:597–601.discussion 601. [DOI] [PubMed] [Google Scholar]
- 14.Schizas C, Michel J, Kosmopoulos V, et al. Computer tomography assessment of pedicle screw insertion in percutaneous posterior transpedicular stabilization. Eur Spine J 2007; 16:613–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laine T, Makitalo K, Schlenzka D, et al. Accuracy of pedicle screw insertion: a prospective CT study in 30 low back patients. Eur Spine J 1997; 6:402–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990; 15:11–14. [DOI] [PubMed] [Google Scholar]
- 17.Dvorak M, MacDonald S, Gurr KR, et al. An anatomic, radiographic, and biomechanical assessment of extrapedicular screw fixation in the thoracic spine. Spine (Phila Pa 1976) 1993; 18:1689–1694. [DOI] [PubMed] [Google Scholar]
- 18.Brasiliense LB, Theodore N, Lazaro BC, et al. Quantitative analysis of misplaced pedicle screws in the thoracic spine: how much pullout strength is lost?: presented at the 2009 Joint Spine Section Meeting. J Neurosurg Spine 2010; 12:503–508. [DOI] [PubMed] [Google Scholar]
- 19.White KK, Oka R, Mahar AT, et al. Pullout strength of thoracic pedicle screw instrumentation: comparison of the transpedicular and extrapedicular techniques. Spine (Phila Pa 1976) 2006; 31:E355–358. [DOI] [PubMed] [Google Scholar]
- 20.Jones DP, Robertson PA, Lunt B, et al. Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine (Phila Pa 1976) 2000; 25:1538–1541. [DOI] [PubMed] [Google Scholar]
- 21.Perisinakis K, Theocharopoulos N, Damilakis J, et al. Estimation of patient dose and associated radiogenic risks from fluoroscopically guided pedicle screw insertion. Spine (Phila Pa 1976) 2004; 29:1555–1560. [DOI] [PubMed] [Google Scholar]
- 22.Bronsard N, Boli T, Challali M, et al. Comparison between percutaneous and traditional fixation of lumbar spine fracture: intraoperative radiation exposure levels and outcomes. Orthop Traumatol Surg Res 2013; 99:162–168. [DOI] [PubMed] [Google Scholar]
- 23.O’Donnell C, Maertens A, Bompadre V, et al. Comparative radiation exposure using standard fluoroscopy versus cone-beam computed tomography for posterior instrumented fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2014; 39:E850–855. [DOI] [PubMed] [Google Scholar]
- 24.Van de Kelft E, Costa F, Van der Planken D, et al. A prospective multicenter registry on the accuracy of pedicle screw placement in the thoracic, lumbar, and sacral levels with the use of the O-arm imaging system and StealthStation Navigation. Spine (Phila Pa 1976) 2012; 37:E1580–1587. [DOI] [PubMed] [Google Scholar]
- 25.Green P. The response of the International Commission on Radiological Protection to calls for a reduction in the dose limits for radiation workers and members of the public. Int J Radiat Biol Relat Stud Phys Chem Med 1988; 53:679–682. [DOI] [PubMed] [Google Scholar]
- 26.Rahmathulla G, Nottmeier EW, Pirris SM, et al. Intraoperative image-guided spinal navigation: technical pitfalls and their avoidance. Neurosurg Focus 2014; 36:E3. [DOI] [PubMed] [Google Scholar]


