Abstract
Religious coping is associated with health outcomes in adolescents with chronic disease. Identifying potentially modifiable spiritual factors is important for improving health outcomes. The purpose of this study was to determine if associations exist between rate of change in pulmonary function and subsequent religious coping by adolescents with cystic fibrosis (CF). Retrospective cohort design employing the Brief R-COPE and calculated decline in lung function over a three-year period were utilized. Data were obtained for 28 adolescents; median age 13.5 years. Use of pleading or negative religious coping was associated with a worse clinical trajectory. Pleading may be ineffective as disease progression is modifiable through adherence to evidence-based treatments. Given established relationships of religious coping with general coping, the effects of declining pulmonary function may be broader. Changes in pulmonary function suggest opportunities for chaplains to explore options to cognitively reframe negative religious coping.
Keywords: adolescence, coping, cystic fibrosis, rate of decline, spirituality
INTRODUCTION
Living with a chronic disease is stressful. The life-shortening nature of cystic fibrosis (CF), with its burdensome daily home treatments including airway clearance, nebulized medications, and enzyme replacement can be particularly stressful. Declining health status of CF patients, as measured by the rapid rate of decline in pulmonary function, is a significant issue. This may be especially true for adolescents, who have the largest CF-mediated decreases in pulmonary function (Liou et al., 2010). People respond to minimize or remove the stress of perceived threats by employing different forms of coping. Therefore, identifying factors associated with slowing disease progression, including coping styles of adolescents, can be an important step in improving health outcomes.
One form of coping which is important to many Americans is religious coping, which is defined as “a search for significance, in ways related to the sacred, in times of stress” (Pendleton, Cavalli, Pargament, & Nasr, 2002, p. 1). Religious coping has been shown to make unique contributions to outcomes above non-religious coping (Burker, Evon, Sedway, & Egan, 2005; Pargament et al., 1999). Religious coping may have different goals: to gain control over a stressor; to seek comfort with the sacred or with other people; or to construct a spiritual meaning for the stressor. Fourteen styles of religious coping have been described (Pargament, Koenig, & Perez, 2000). Styles used to gain control include: Collaboration (with the Divine), Passive Deferral, Active Surrender, Pleading for Divine Intervention, and Self-directed. Comfort-related styles include Seeking Spiritual Support, Seeking Spiritual Connection, and Spiritual Discontent, which manifests as a feeling of being abandoned by the Divine or by one’s faith community. Religious coping by constructing meaning may include reappraisals of Divine power or of the stressor as either Demonic or a Punishing God (Pargament, et al., 2000). Coping styles that sustain comfort, hope, and spiritual meaning are referred to as “positive religious coping,” while styles that challenge one’s comfort, hope, or meaning are referred to as “negative religious coping” (Pargament, 1997). Many adolescents have active spiritual lives (Boyatzis, Dollahite, & Marks, 2006; Fowler, 1981; Grossoehme, Cotton, & Leonard, 2007), and use of religious coping by adolescents previously has been reported in relation to sickle cell disease, asthma, and alcohol use (Benore, Pargament, & Pendleton, 2008; Cotton et al., 2009; Knight et al., 2007).
Religious coping styles have been associated with health outcomes. Negative relationships include the use of some coping styles with poorer treatment adherence by adolescents who are post renal transplant (Ratcliff, Blount, & Mee, 2010). In a study of treatment adherence by parents for their child’s CF, negative religious coping was associated with depressive symptoms, which was associated to self-efficacy and actual adherence to airway clearance treatments (Grossoehme et al., 2012). Pleading religious coping (a form of coping to gain control by seeking divine intervention) was associated with self-efficacy for completing nebulized medications and was directly related to actual adherence to administering enzyme supplements (Grossoehme et al., 2012). Rivett and colleagues suggested that the quality of life for adolescents with idiopathic scoliosis may be more related to their coping styles than to their physical condition and its implications (Rivett, Rothberg, Stewardt, & Berkowitz, 2009). Benore reported that negative religious coping predicted up to 50% of variance in adjustment to asthma in children (Benore et al., 2008), and Dew and colleagues reported that negative religious coping was significantly related to depression among adolescents at two outpatient psychiatric clinics (Bosek, Lowry, Lindeman, Burck, & Gwyther, 2003). A 44-study review of religious coping and health outcomes found that poorer health outcomes were associated with negative religious coping (Pargament, 1997). Negative religious coping also predicted 11.6% of the variation among depression scores in a sample of lung-transplant candidates, which included young adults with CF (Burker et al., 2005). However, no previous studies have examined the potential relationship between adolescents’ reports of religious coping and pulmonary function decline due to CF.
As a first step toward understanding whether religious coping could be a modifiable factor in a future intervention, this exploratory study was designed to (1) determine the reliability of a religious coping instrument (the Brief R-COPE) among adolescents with CF; (2), based on previous studies among adults, test the hypothesis that the rate of decline in pulmonary function would be associated with subsequent negative religious coping; and (3), test the hypothesis that styles of religious coping for control would be associated with rates of pulmonary decline. Pulmonary function was operationalized as FEV1% (Forced Expiratory Volume: the ratio of the volume of air that is forcibly expelled in one second compared to predicted norms) over a three-year period. A multi-year FEV1 slope is a common measure of patient-specific trends in pulmonary function used in retrospective analyses (Dasenbrook, Merlo, Diener-West, Lechtzin, & Boyle, 2008; Konstan, Byard, Hoppel, & Davis, 1995; Konstan, Schluchter, Xue, & Davis, 2007; McPhail, Acton, Fenchel, Amin, & Seid, 2008).
METHODS
Participants
This institution’s IRB approved the study. Data were collected from a convenience sample of 19 adolescent males and 9 adolescent females (N=28). The first author collected religious coping data from the adolescents (11–18 years of age, median=13.5 years) during outpatient anniversary clinic visits to the CF Center in his role as clinical chaplain. Completion of the Brief R-COPE was voluntary, and the adolescents received no incentive. The sample represents 34% of the adolescents who performed valid pulmonary function tests and had at least three years of pulmonary function test scores at the time of this study.
Measures
Portions of the Brief R-COPE were used to measure patients’ religious coping (Bush et al., 1999; Cotton et al., 2006; Keefe et al., 2001; Koenig, Pargament, & Nielsen, 1998; Pargament, et al., 2000; Pargament, Koenig, Tarakeshwar, & Hahn, 2001, 2004). The first seven items in Table 1 measured negative religious coping styles; the final item in Table 1 (item # 7) measured the Pleading style of religious coping for control). All items were scored on a four-point Likert-style scale in response to the question, “How often have you used the following to cope with your CF?” Responses range from 0 (“not at all”) to 3 (“quite a bit”). Given the sample size and the relatively low prevalence of negative religious coping use, we followed an approach similar to that described by Fitchett and colleagues to reduce bias in odds ratios from logistic regressions by dichotomizing the responses into “used” and “not used” (Fitchett et al., 2004; Nemes, Jonasson, Genell, & Steineck, 2009). To determine whether or not a participant had a particular religious coping style, corresponding item scores less than 2 were categorized as “not used” while scores of 2 or above were categorized as “used.” Participants that used any of the seven negative religious coping styles were classified as exhibiting negative religious coping.
TABLE 1.
Frequencies of Individual Brief R-COPE Item Responses
| Brief R-COPE item | Frequency
|
|
|---|---|---|
| “Not at all” or “Somewhat” N (%) |
“Quite a bit” or “A great deal” N (%) |
|
| 2. Wondered whether God had abandoned me. | 27 (100%) | 0 |
| 4. Felt punished by God for my lack of devotion. | 26 (96%) | 1 (4%) |
| 6. Wondered what I did for God to punish me. | 24 (96%) | 1 (4%) |
| 8. Questioned God’s love for me. | 26 (96%) | 1 (4%) |
| 10. Wondered whether my church had abandoned me. | 27 (100%) | 0 |
| 12. Decided the devil made this happen. | 26 (96%) | 1 (4%) |
| 14. Questioned the power of God. | 26 (96%) | 1 (4%) |
| 7. Tried to put my plans into action together with God. | 14 (58%) | 11 (42%) |
All available FEV1% values for each participant during the three years prior to the date they completed the Brief R-COPE were obtained by a retrospective chart review. From this, the FEV1% rate of change was calculated for each participant by performing individual least-squares regressions of observed FEV1% as a function of age (in years). The resulting slope, used in a previous study as an aggregate patient-level measure of change in lung function over time, is expressed as percent predicted per year (McPhail et al., 2008).
Analysis
Spearman correlations were calculated between religious coping (measured on the Likert-style scale) and quantitative clinical and demographic characteristics. The association between FEV1% slope and dichotomized religious coping use was examined using logistic regression. In each regression, the preceding FEV1% slope was treated as the predictor variable and the subsequent religious coping outcome was treated as the response variable. Clinical and demographic characteristics significant at p<0.10 in individual regressions were included in each final model. Covariates included gender, age at initial pulmonary function test (in years), baseline FEV1%, and time in months between the first pulmonary function test and completing the Brief R-COPE. Model results are reported as odds ratios (OR) with the 95%confidence interval (CI), along with regression (β) coefficient and standard error (SE). All statistical analyses were implemented in SAS 9.2 (SAS Institute, Cary, NC).
RESULTS
Baseline FEV1 was 91.2 (25.6–118.4) % predicted; median (range) for FEV1% slope was −2.4 (−9.4 to 6.0) % predicted per year. Time between initial FEV1 measurement and completing the subsequent Brief R-COPE was 2.85 (2.53–2.97) years. Reliability (Cronbach’s alpha) for the R-COPE was 0.62 for the negative religious item subscale. Frequencies for specific negative religious coping and Pleading religious coping styles are presented in Table 1. No associations were found between positive religious coping styles and pulmonary function and no data is reported.
A negative correlation was found between an adolescent’s baseline pulmonary function (FEV1%) and the elapsed time between that baseline FEV1 measurement and the time they completed the Brief R-COPE (rho= −0.45; p=0.018). There was a negative correlation between an adolescent’s age at the time of their baseline pulmonary function test and their baseline FEV1 value (rho=−0.53; p=0.0043). No correlations existed between FEV1 slope and either baseline FEV1 score or age at baseline FEV1.
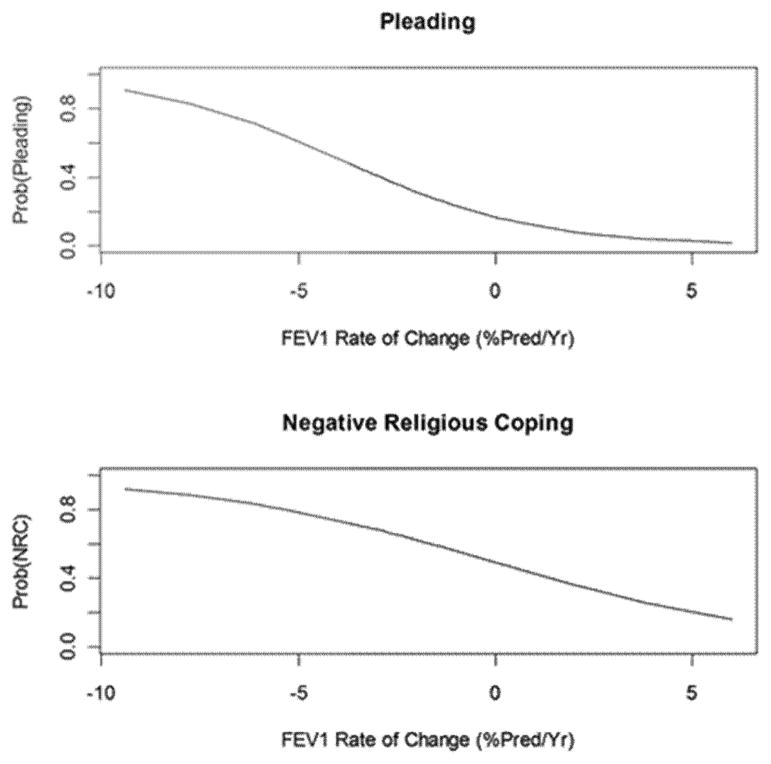
There was a significant association between the use of one of the styles of religious coping for control (Pleading) and the adolescent’s rate of change in pulmonary function. For every 1% predicted per year increase in FEV1% slope, the odds that adolescents used Pleading religious coping decreased by 34% (OR=0.66, β=−0.41, SE=0.21; p=0.045). There also was a significant association between the use of negative religious coping styles and the adolescents’ three-year pulmonary function slope (OR=0.77, β=−0.27, SE=0.13; p=0.046). For every 1% predicted per year increase in FEV1%, the odds of using one or more negative coping styles decreased by 24% (p=0.0462; OR=0.765; 95% CI:0.587, 0.995). The change in probability of using religious coping styles, specifically Pleading religious coping and any negative religious coping style, across pulmonary function rates of change are presented in Figure 1. In each plot, the x-axis represents the three-year FEV1% slope for study patients; the y-axis is the predicted probability of each outcome. Both predictions indicate that a negative relationship exists between the adolescents’ pulmonary function changes and subsequent use of negative religious coping.
FIGURE 1.
The use of pleading and negative religious coping across pulmonary function (FEV1%) rates of change.
Adolescents with more rapid rates of decline in lung function were more likely to use the Pleading style of religious coping. Both models suggest that a negative relationship exists between certain religious coping styles and longitudinal changes in lung function. Positive rates of change in lung function corresponded to lower probability (less use) of Pleading. The probability of using any religious coping was lower for less rapid pulmonary function decline; however, compared to Pleading, the probability of any negative religious coping use did not decrease as sharply. These results suggest that negative religious coping was still being used, even when adolescents experienced lung function changes above the normal range for their healthier counterparts.
DISCUSSION
Our findings demonstrate the reliability of the Brief R-COPE instrument in adolescents with CF. This is significant since it allows for new avenues for both screening adolescents for spiritual struggle and research involving the religious coping styles of adolescents. Screening for spiritual struggle is important due to the association of negative religious coping (often a marker of spiritual struggle) with poorer physical and mental health outcomes and because persons likely to experience spiritual struggle are less likely to request chaplaincy care (Fitchett, Meyer, & Burton, 2000). If chaplaincy services are a limited resource, the need to identify those in need of intervention increases and use of the Brief R-COPE can assist chaplains in addressing this issue.
Our study is the first to report an association between clinical decline in adolescents with CF and the use of negative religious coping. Faster pulmonary function decline was associated with increased odds of using negative religious coping, suggesting two clinical implications for chaplains. First, adolescents with faster decline in pulmonary function may be screened for negative religious coping. Second, adolescents using negative religious coping may become a focus of clinical attention for the chaplain. However, it is important to note “faster” is not the same as “poor” pulmonary function, nor does it imply a rapid decline near the end of life. Our findings suggest that such a rapid decline, even in an adolescent whose pulmonary function used to exceed 100% of their predicted functioning, and who experiences a precipitous decline, has increased the odds of that adolescent using negative religious coping compared to an adolescent with relatively poor, but constant, pulmonary function. Thus, the adolescent who may benefit from a chaplain’s intervention is one who, formerly active in school sports, has declined to the point where this is no longer possible, and has lost their sense of identity as an athlete or who may be struggling against the identify of being a “sick” person. Negative religious coping in adolescents is associated with psychological distress and symptoms of anxiety and depression (Terreri & Glenwick, 2011). An assessment of spiritual and psychological health should be considered for all adolescents with chronic disease.
In this study, Pleading religious coping was associated with a worse clinical trajectory. Pargament and colleagues considered Pleading to be ineffective coping when a person could control the outcome of a situation (Pargament, 1997). CF disease progression is modifiable through treatment adherence to an evidence-based pulmonary regimen. Therefore, Pleading religious coping, in this context, could be interpreted as ineffective coping. Pleading coping could be used in clinical chaplaincy practice to identify patients who might benefit from referral for adherence-improving interventions. Pleading coping also could be used to identify adolescents with whom a chaplain may facilitate exploring options to help cognitively reframe their negative coping styles. Until more is known, cognitive reframing interventions may have greater impact on other outcomes, such as mental health.
The limitations of this study include a limited retrospective convenience sample from a single site. Nevertheless, there are noteworthy findings: adolescents do use spiritual styles of coping in relation to their disease, and this study demonstrates that the Brief R-COPE can be used with adolescents. Further, we report an association of lung function decline in CF patients with subsequent religious coping. Future studies should test the modifiability of adolescents’ religious coping styles. The study design does not permit causality to be addressed; however, the subsequent collection of religious coping data means it may have existed prior to completing the Brief R-COPE. A prospective longitudinal, multi-site study including other covariates to construct a model addressing causality and mechanisms of action is needed. Exploration of the utility of the Brief R-COPE with adolescents, including development of an age-specific version and or alternative scoring, is needed. Until such studies are completed, however, chaplains and other pulmonary team clinicians may consider the use of either FEV1 slope (rate of decline of pulmonary function) or religious coping styles for further assessment or possible intervention.
Acknowledgments
This study was funded in part by NIH=NICHD K23 HD062642 (PI: Grossoehme) and by the Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center (Raouf Amin, MD, Director). The authors gratefully acknowledge the contributions of medical writer Denise Wetzel to this article, and Jane Khoury, PhD and Phil Khoury, PhD for their assistance.
Footnotes
Portions of this article were previously presented in poster form at the 2011 North American Cystic Fibrosis Conference (November 3–5, 2011, Anaheim, CA).
Contributor Information
DANIEL H. GROSSOEHME, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA
RHONDA SZCZESNIAK, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA and Division of Biostatistics and Epidemiology, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA.
GARY L. MCPHAIL, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA
MICHAEL SEID, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA and James Anderson Center for Health Systems Excellence, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA.
References
- Benore E, Pargament KI, Pendleton SM. An initial examination of religious coping in children with asthma. International Journal for the Psychology of Religion. 2008;18:267–290. [Google Scholar]
- Bosek MS, Lowry E, Lindeman DA, Burck JR, Gwyther LP. Promoting a good death for persons with dementia in nursing facilities: Family caregivers’ perspectives. JONA’S Healthcare Law, Ethics and Regulation. 2003;5(2):34–41. doi: 10.1097/00128488-200306000-00006. [DOI] [PubMed] [Google Scholar]
- Boyatzis CJ, Dollahite DC, Marks LD. The family as a context for religious and spiritual development in children and youth. In: Roehlkepartain EC, King PE, Wagener L, Benson P, editors. The handbook of spiritual development in childhood and adolescence. Thousand Oaks, CA: SAGE Publications; 2006. pp. 297–309. [Google Scholar]
- Burker EJ, Evon DM, Sedway JA, Egan T. Religious and non-religious coping in lung transplant candidates: Does adding God to the picture tell us more? Journal of Behavioral Medicine. 2005;28(6):513–526. doi: 10.1007/s10865-005-9025-4. [DOI] [PubMed] [Google Scholar]
- Bush EG, Rye MS, Brant CR, Emery E, Pargament KI, Riessinger CA. Religious coping with chronic pain. Applied Psychophysiology and Biofeedback. 1999;24(4):249–260. doi: 10.1023/A:1022234913899. [DOI] [PubMed] [Google Scholar]
- Cotton S, Grossoehme D, Rosenthal SL, McGrady ME, Roberts YH, Hines J, Tsevat J. Religious=spiritual coping in adolescents with sickle cell disease a pilot study. Journal of Pediatric Hematology and Oncology. 2009;31(5):313–318. doi: 10.1097/MPH.0b013e31819e40e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Puchalski CM, Sherman SN, Mrus JM, Peterman AH, Feinberg J, Tsevat J. Spirituality and religion in patients with HIV=AIDS. Journal of General Internal Medicine. 2006;21(Suppl 5):S5–13. doi: 10.1111/j.1525-1497.2006.00642.x. JGI642 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasenbrook EC, Merlo CA, Diener-West M, Lechtzin N, Boyle MP. Persistent methicillin-resistant staphylococcus aureus and rate of FEV1 decline in cystic fibrosis. American Journal of Respiratory and Critical Care Medicine. 2008;178:814–821. doi: 10.1164/rccm.200802-327OC. [DOI] [PubMed] [Google Scholar]
- Fitchett G, Meyer PM, Burton LA. Spiritual care in the hospital: Who requests it? who needs it? Journal of Pastoral Care. 2000;54(2):173–186. doi: 10.1177/002234090005400207. [DOI] [PubMed] [Google Scholar]
- Fitchett G, Murphy PE, Kim J, Gibbons JL, Cameron JR, Davis JA. Religious struggle: Prevalence, correlates and mental health risks in diabetic, congestive heart failure and oncology patients. International Journal of Psychiatry in Medicine. 2004;34(2):179–196. doi: 10.2190/UCJ9-DP4M-9C0X-835M. [DOI] [PubMed] [Google Scholar]
- Fowler JW. Stages of faith. New York, NY: HarperCollins; 1981. [Google Scholar]
- Grossoehme DH, Cotton S, Leonard A. Spiritual and religious experiences of adolescent psychiatric inpatients versus healthy peers. Journal of Pastoral Care and Counseling. 2007;61(3):197–204. doi: 10.1177/154230500706100304. [DOI] [PubMed] [Google Scholar]
- Grossoehme DH, Dimitriou S, Szczesniak R, Britton L, McPhail G, Seid M. Parental spirituality, depression, and marital adjustment: Role in treatment adherence. Paper presented at the North American Cystic Fibrosis Conference; 2012; Orlando, FL. 2012. [Google Scholar]
- Keefe FJ, Affleck G, Lefebvre J, Underwood L, Caldwell DS, Drew J, Pargament K. Living with rheumatoid arthritis: The role of daily spirituality and daily religious and spiritual coping. Journal of Pain. 2001;2(2):101–110. doi: 10.1054/jpai.2001.19296. S1526-5900(01)22873-9 [pii] doi:10.1054=jpai.2001.19296. [DOI] [PubMed] [Google Scholar]
- Knight JR, Sherritt L, Harris SK, Holder DW, Kulig J, Shrier LA, Chang G. Alcohol use and religiousness=spirituality among adolescents. Southern Medical Journal. 2007;100(4):349–355. doi: 10.1097/SMJ.0b013e3180316a32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, Pargament KI, Nielsen J. Religious coping and health status in medically ill hospitalized older adults. Journal of Nervous and Mental Disease. 1998;186(9):513–521. doi: 10.1097/00005053-199809000-00001. [DOI] [PubMed] [Google Scholar]
- Konstan MW, Byard PJ, Hoppel CL, Davis PB. Effect of High-Dose Ibuprofen in patients with cystic fibrosis. New England Journal of Medicine. 1995;332(13):848–854. doi: 10.1056/NEJM199503303321303. [DOI] [PubMed] [Google Scholar]
- Konstan MW, Schluchter MD, Xue W, Davis PB. Clinical use of ibuprofen is associated with slower FEV1 decline in children with cystic fibrosis. American Journal of Respiratory and Critical Care Medicine. 2007;176:1084–1089. doi: 10.1164/rccm.200702-181OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liou TG, Elkin EP, Pasta DJ, Jacobs JR, Konstan MW, Morgan WJ, Wagener JS. Year-to-year changes in lung function in individuals with cystic fibrosis. Journal of Cystic Fibrosis. 2010;9:250–256. doi: 10.1016/j.jcf.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhail GL, Acton JD, Fenchel Mc, Amin RS, Seid M. Improvements in lung funtion outcomes in children with cystic fibrosis are associated with better nutrition, fewer chronic pseudomonas aeruginosa infections and dornase alfa use. Journal of Pediatrics. 2008;153(6):752–757. doi: 10.1016/j.jpeds.2008.07.011. [DOI] [PubMed] [Google Scholar]
- Nemes S, Jonasson JM, Genell A, Steineck G. Bias in odds ratios by logistic regression modeling and sample size. BMC Medical Research Methodology. 2009;9(56) doi: 10.1186/1471-2288-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pargament KI. Psychology of religious coping. New York, NY: Guildford Press; 1997. [Google Scholar]
- Pargament KI, Cole B, VandeCreek L, Belavich T, Brant CR, Perez LM. The vigil: Religion and the search for control in the hospital waiting room. Journal of Health Psychology. 1999;4:327–341. doi: 10.1177/135910539900400303. [DOI] [PubMed] [Google Scholar]
- Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: Development and Initial validation of the RCOPE. Journal of Clinical Psychology. 2000;56(4):519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients: A 2-year longitudinal study. Archives of Internal Medicine. 2001;161(15):1881–1885. doi: 10.1001/archinte.161.15.1881. ioi00736 [pii] [DOI] [PubMed] [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. Journal of Health Psychology. 2004;9(6):713–730. doi: 10.1177/1359105304045366. [DOI] [PubMed] [Google Scholar]
- Pendleton SM, Cavalli KS, Pargament KI, Nasr SZ. Religious/spiritual coping in childhood cystic fibrosis: A qualitative study. Pediatrics. 2002;109(1):e8–e8. doi: 10.1542/peds.109.1.e8. [DOI] [PubMed] [Google Scholar]
- Ratcliff MB, Blount RL, Mee LL. The relationship betwen adolescent renal transplant recipients’ perceived adversity, coping and medical adherence. Journal of Clinical Psychology in Medical Settings. 2010;17(2):116–124. doi: 10.1007/s10880-010-9194-3. [DOI] [PubMed] [Google Scholar]
- Rivett L, Rothberg A, Stewardt A, Berkowitz R. The relationship between quality of life and compliance to a brace protocol in adolescents with idiopathci scoliosis: A comparitive study. BMC Musculoskeletal Disorders. 2009;10(5) doi: 10.1186/1471-2474-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terreri CJ, Glenwick DS. The relationship of religious and general coping to psychological adjustment and distress in urban adolescents. Journal of Religion and Health. 2011:1–15. doi: 10.1007/s10943-011-9555-8. [DOI] [PubMed] [Google Scholar]