Abstract
Range-of-motion (ROM) assessment is a critical assessment tool during the rehabilitation process. The conventional approach uses the goniometer which remains the most reliable instrument but it is usually time-consuming and subject to both intra- and inter-therapist measurement errors. An automated wireless wearable sensor system for the measurement of ROM has previously been developed by the current authors. Presented is the correlation and accuracy of the automated wireless wearable sensor system against a goniometer in measuring ROM in the major joints of upper (UEs) and lower extremities (LEs) in 19 healthy subjects and 20 newly disabled inpatients through intra (same) subject comparison of ROM assessments between the sensor system against goniometer measurements by physical therapists. In healthy subjects, ROM measurements using the new sensor system were highly correlated with goniometry, with 95% of differences < 20° and 10° for most movements in major joints of UE and LE, respectively. Among inpatients undergoing rehabilitation, ROM measurements using the new sensor system were also highly correlated with goniometry, with 95% of the differences being < 20° and 25° for most movements in the major joints of UE and LE, respectively.
Keywords: wireless sensor networks, biomechanics, motion measurement, patient rehabilitation, goniometers, biomedical equipment
Keywords: goniometer measurements, rehabilitation process, range-of-motion assessment, lower extremity joints, upper extremity joints, wireless wearable range-of-motion sensor system
1. Introduction
Clinical measurement of range-of-motion (ROM) is a fundamental evaluation procedure in rehabilitation. ROM is also the most widely used evaluation procedure in rehabilitation by physiotherapists and occupational therapists to quantify baseline joint function, guide appropriate therapeutic interventions and document the effectiveness of these rehabilitation interventions. The universal goniometer (i.e. full-circle manual goniometer) remains the most versatile, reliable and widely used instrument in clinical practice to measure ROM [1]. However, most physical therapists do not routinely use goniometers to measure joint ROM because the process is cumbersome and time-consuming, preferring to rely on visual estimation, which is dependent on the experience of the assessor [2] and unreliable [3, 4], especially when objectivity and accuracy are needed.
Specialised methods to measure ROM, like photography [5, 6] or radiography [7, 8] have been developed but are largely unused by physical therapists because they are expensive, difficult to set up, not portable and not easily used at the bedside or at home and expose patients to unnecessary risks such as radiation. In tandem, with technological advancements in recent years, several sensor systems that are more portable and user-friendly have been developed to measure ROM. However, some of these sensor systems only measure gross whole body [9] movements or upper against lower body segment movements [10], and not ROM at specific joints. Other sensor systems have been developed to measure ROM at only a single joint [5, 7, 8, 11, 12] or a series of complex joints as a whole (e.g. spine) [13]. Watanabe and Saito [14] recently developed a wireless wearable sensor system for joint angle measurement of the major joints in the lower extremities (LEs) (i.e. hip, knee and ankle) [14]. However, their system only measured ROM in a single plane (e.g. only hip flexion and extension were measured but hip abduction, adduction, internal rotation and external rotation were neglected) and did not measure ROM in the upper extremities (UEs). Finally, most of these papers were engineering-centric with minimal involvement of physical therapists and rehabilitation physicians, focusing on the engineering aspects of the system (e.g. algorithms used for joint angle measurements) and testing their system only on a small sample of subjects (usually n = 1 to 3).
We have previously developed an automated portable wireless wearable sensor system to measure ROM in all planes of the major joints of the UEs (shoulder, elbow, radio-ulnar and wrist) and LEs (hip, knee and ankle) in collaboration with engineers, rehabilitation physicians, physiotherapists and occupational therapists. Details on the engineering aspects of the sensor system and the algorithms used are described in Lee et al. [15]. In this Letter, we report the correlation and agreement between the sensor system and goniometer in measuring ROM in all planes of the major joints of UEs and LEs in 19 healthy subjects and 20 newly disabled inpatients.
2. Methods
The sensor system was first tested by attaching the sensors to the movable arm of a 12 in goniometer and recording the angle read by the sensor for every 5° rotation of the movable arms of the goniometer. The sensor system was then tested on a group of healthy non-disabled fully independent subjects who were either undergraduate, graduate or staff of the National University of Singapore (NUS), to assess the correlation and agreement between the sensor system and the goniometer in measuring ROM for all major joints of the UEs and LEs bilaterally. For both the sensor system and goniometer measurements in subjects, only active ROM was tested and maximal angles were recorded. Subjects were invited to participate through email advertisement and the validation study was conducted over four days: two days for UE and two days for LE testing.
For UE assessment, the sensors were placed in a customised pocket and mounted onto the back of the neck via a snug but flexible three-quarter circle plastic holder (Figs. 1a and 2a), and bilaterally to the lateral mid-upper arm parallel to the humerus (Figs. 1a and 2b), volar aspect of the mid-forearm parallel to the ulnar bone (Figs. 1a and 2c) and dorsum of the hand parallel to the third meta-carpal bone (Figs. 1a and 2d), via a firmly secured Velcro® strap (to minimise sensor displacement during movement). Similarly, for LE assessment, the sensor nodes were attached bilaterally to the anterior mid-thigh parallel to the distal femur, lateral side of the calf parallel to the tibia mid-calf and dorsum of the forefoot parallel to the third meta-tarsal bone (Fig. 1b). Each of the sensors contained a gyroscope, accelerometer, compass (magnetometer), micro-controller and a wireless communication chip, allowing it to measure angles of motion and velocity in all three spatial dimensions and to determine the sensor's position in relation to gravity, left–right orientation and the four cardinal directions of navigation (i.e. North, South, East and West). In standardised ROM measurements, each joint has specific movements from which ROM is traditionally measured. For the UE: in the shoulder joint, the standardised movements are flexion, extension, abduction–adduction, internal rotation and external rotation; in the elbow joint, they are flexion and extension; in the superior–inferior radio-ulnar joint, they are forearm supination and pronation; and in the wrist joint, they are flexion, extension, radial and ulnar deviation. For the LE: in the hip joint, the standardised movements are flexion, extension, abduction, adduction, internal rotation and external rotation; in the knee joint, they are flexion and extension; in the ankle joint, they are dorsi-flexion and plantar-flexion. Although the sensor system can measure ROM in two or more planes, this Letter will focus on reporting the correlation and accuracy of ROM measurements of these standardised movements against goniometry which can only measure ROM in one plane. A detailed explanation of the initial position, action performed by the subject and actual angle measured by the sensor system for each movement in all major joints of the UEs and LEs is found in Table 1. The wearable sensor nodes attached onto the patient communicate with a central server, which can be a desktop, laptop, tablet or mobile smart-phone (in this study, a standard laptop was used for LE testing and an Android smart-phone used for UE testing). Each of the sensor nodes detected and sent the data from its accelerometer, gyroscope and compass wirelessly to an application running on the central server at 25 Hz.
Figure 1.
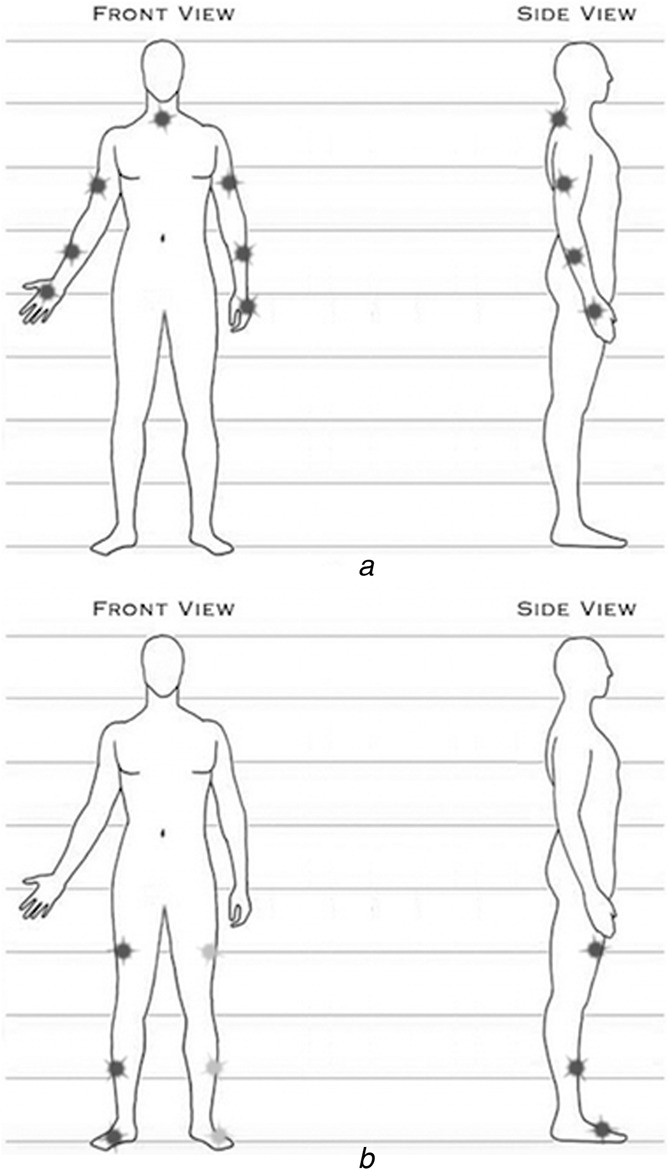
Positions of sensors on UEs and LEs
a UEs
b LEs
Figure 2.
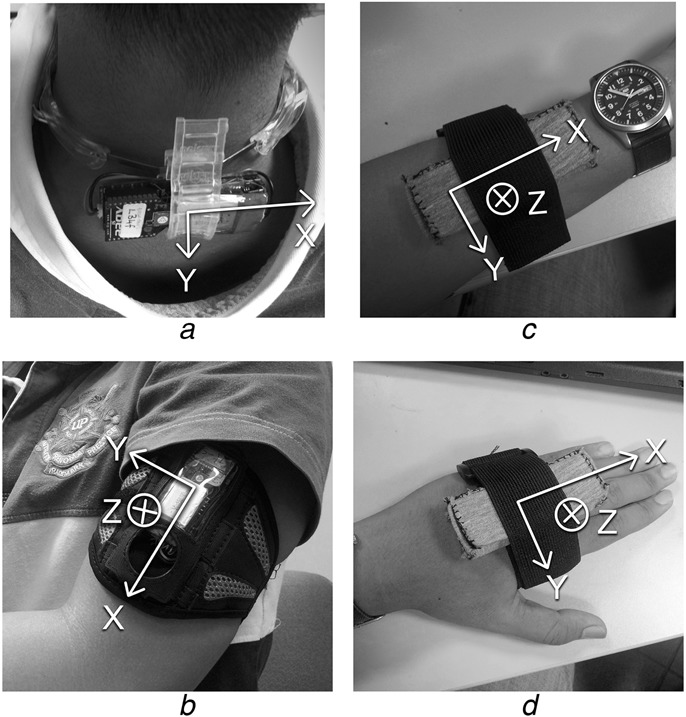
Photograph of sensor set up on neck, upper arm, forearm and hand
a Neck
b Upper arm
c Forearm
d Hand
Table 1.
Description of standard procedures used in sensor system to determine active ROM of major joints of UEs and LEs
| Joint | Activity (normal ROM) | Initial position | Action | Angle measured by sensor system in degrees |
|---|---|---|---|---|
| shoulder | flexion (0–180°) | the subject can be in sitting or standing position. The forearm does not need to point directly downwards, even though the ROM for this activity is calculated from the vertical | the subject moves his/her humerus in an anterior and upwards direction | angle between the humerus and the gravity |
| extension (0–30°) | the subject moves his/her humerus posteriorly as much as possible | |||
| abduction (0–180°) | the subject moves his/her humerus laterally and upwards as much as possible | |||
| internal rotation (0–70°) | the subject can be in sitting or standing position with the elbow flexed to 90° and the forearm in mid-position | the subject moves his/her palm towards the abdomen as much as possible while maintaining the 90° flexion of the elbow | angle through which the forearm has moved, starting from the initial position | |
| external rotation (0–90°) | the subject moves his/her palm away from the abdomen as much as possible while maintaining the 90° flexion of the elbow | |||
| elbow | flexion (0–150°) | the subject is in sitting or standing position, with the elbow extended (as close to 0° as possible) | the forearm moves in an anterior direction to bring the palm towards the shoulder as much as possible | angle through which the forearm has moved, starting from the initial position, relative to the upper arm |
| radio-ulnar | pronation (0–90°) | the subject is in sitting or standing position with the elbow flexed to 90°, forearm in mid-position and the palms facing each other | the forearm rotates about itself so that the palm faces downwards | angle through which the forearm has been rotated |
| supination (0–90°) | the forearm rotates about itself so that the palm faces upwards | |||
| wrist | flexion (0–80°) | the subject is in sitting or standing position with the forearm resting on the table in pronation and the hand over the end of the table with the fingers relaxed | the subject moves the hand in a volar direction as much as possible, with the fingers relaxed | the elevation or depression angle through which the wrist is moved |
| extension (0–70°) | the subject moves the hand in a dorsal direction as much as possible with the fingers relaxed | |||
| radial deviation (0–20°) | the subject is in sitting or standing position with the forearm and the hand resting on the table in pronation with the fingers relaxed | the subject moves the hand in the radial direction as much as possible | the heading angle through which the wrist has been turned | |
| ulnar deviation (0–30°) | the subject moves the hand in the ulnar direction as much as possible | |||
| hip | flexion (0–120°) | the subject is to be supine with at least the test side (left or right) of the LE resting on a plinth. For adduction, the hip is to be abducted on the non-test side at the start | the hip flexes to bring the kneecap as close to the chest as possible until the limit of motion | angle that the distal femur on the test side has swept through, from start of the activity to its end |
| abduction (0–45°) | the hip abducts to turn the distal femur of the test side laterally away from the non-test side | |||
| adduction (0–30°) | the hip adducts to turn the distal femur of the test side laterally towards the abducted non-test side | |||
| extension (0–30°) | the subject is to lay sideways with the hip and knee of the test side in neutral position. The hip and knee of the non-test side are to be partially flexed to stabilise the pelvis | the hip on the test side extends as much as possible | angle that the distal femur on the test side has swept through | |
| internal rotation (0–45°) | the subject is in sitting position with the hip in 90° of flexion and the knee in neutral rotation, with the hip on the non-test side abducted slightly so as to ensure sufficient space for the external rotation to take place | the hip internally rotates as much as possible while the position of the femur is maintained | ||
| external rotation (0–45°) | the hip externally rotates as much as possible while the position of the femur is maintained | |||
| knee | flexion (0–135°) | the subject is to be supine with the test side of the LE resting on a plinth | the heel moves towards the buttock as much as possible | angle moved by the longitudinal axis of the fibula |
| ankle | dorsi-flexion (0–20°) | the subject is to be supine with the ankle over the end of the plinth | the ankle flexes as much as possible while the position of the fibula on the test side is maintained | angle swept by the heel |
| plantar-flexion (0–50°) | the ankle extends as much as possible while the position of the fibula on the test side is maintained |
For subject testing, after a participant wearing the sensor system achieved the maximal excursion of a particular movement in a specific joint, the maximal active ROM was measured by the occupational therapist or physiotherapist following the protocols as described by Clarkson [16] and the equivalent angle measured by the sensor was recorded by an independent engineering research assistant. Similar pairs of readings were recorded for the rest of the other movements for every major joint of the four extremities. Research ethics approval was obtained from NUS Institutional Review Board (reference code 11-013 and approval number NUS-1270), informed consent was taken from all participants and participation was voluntary.
We used Pearson's correlation to compare the maximal active ROM measured using the sensor system and goniometry and report the Pearson's correlation coefficient (). Taylor's system of categorising absolute values was adopted in this study: values < 0.35 were considered as weak correlation, 0.36–0.67 as moderate correlation and 0.68–0.89 as strong correlation and values > 0.9 as very high correlation [17]. We also used Bland–Altman plots, which are scatter plots of the difference between the measurements of the sensor system and goniometer (vertical axis) against the average of the measurements of the sensor system and goniometer (horizontal axis) [18, 19]. As all the Bland–Altman plots for each joint movement did not demonstrate obvious heteroscedasticity, logarithmic transformation was not performed. The 95% upper and lower bounds of the mean difference in ROM measured by the sensor system and goniometer were also determined and indicated in all Bland–Altman plots generated.
Details on the characteristics of the final study population for healthy subjects and newly disabled inpatients by UE and LE test groups are found in Table 2. The healthy subject population was young, with a mean age of 24.6 and 24.9 years in the UE and LE groups, respectively. The disabled patient population was elderly with a mean age of 68.4 and 70.7 years in the UE and LE groups, respectively. In both study populations, there were more females and the majority of participants were Chinese, which reflects the ethnic distribution of multi-ethnic Singapore.
Table 2.
Characteristics of study population of healthy subjects and newly disabled elderly inpatients
| Characteristic | UE | LE |
|---|---|---|
| Healthy subjects | (n = 19) | (n = 19) |
| age (years) (mean ± SD) | 24.6 ± 6.7 | 24.9 ± 6.7 |
| sex, n, % | ||
| male | 6 (31.6) | 7 (36.8) |
| female | 13 (68.4) | 12 (63.2) |
| ethnic group, n, % | ||
| Chinese | 9 (47.4) | 8 (42.1) |
| non-Chinese | 10 (52.6) | 11 (57.9) |
| Newly disabled patients | (n = 19) | (n = 20) |
| age (years) (mean ± SD) | 68.4 (8.9) | 70.7 (8.8) |
| gender, n, % | ||
| male | 4 (21.1%) | 4 (20%) |
| female | 15 (72.9%) | 16 (80%) |
| ethnic group, n, % | ||
| Chinese | 17 (89.5%) | 18 (90%) |
| non-Chinese (i.e. Malay or Indian) | 2 (10.5%) | 2 (10.0%) |
| principal diagnosis, n, % | ||
| post knee replacement for | 6 | 5 |
| osteoarthritis | ||
| post hip arthroplasty for fracture | 4 | 5 |
| stroke | 2 | 4 |
| other fractures (e.g. patella, ankle) | 2 | 1 |
| sepsis | 1 | 2 |
| Parkinson's disease | 1 | 1 |
| deconditioning | 1 | 1 |
| knee osteoarthritis (without surgery) | 1 | 0 |
| deep vein thrombosis | 1 | 0 |
| cancer | 0 | 1 |
| Shah-modified Barthel index (mean ± SD) | ||
| personal hygiene (range = 0–5) | 4.2 (1) | 4.7 (0.5) |
| bathing (range = 0–5) | 2.8 (1) | 3.1 (1.4) |
| dressing (range = 0–10) | 6.1 (1.8) | 7.8 (1.7) |
| feeding (range = 0–10) | 8.8 (1.9) | 9.2 (1.4) |
| toileting (range = 0–10) | 5.4 (2.5) | 6.4 (2.6) |
| bowel control and management (range = 0–10) | 7.2 (2.3) | 7.5 (3.3) |
| bladder control and management, (range = 0–10) | 7.4 (2.3) | 8 (3) |
| transferring (chair to bed), (range = 0–15) | 9.8 (3) | 10.5 (3.2) |
| mobility (ambulation), (range = 0–15) | 8.4 (4.3) | 7.9 (4.7) |
| stairs (range = 0–10) | 0.4 (1.2) | 0.3 (1.1) |
| total (range = 0–100) | 60.4 (15.2) | 62.1 (20.9) |
3. Results (healthy subjects)
The between the goniometer and the sensor applied to the movable arm of the goniometer was very highly correlated at 1 (Fig. 3). When all measurements taken using the goniometer and the sensor were taken into consideration, the for UE and LE assessments were 0.97 (Fig. 4a) and 0.99 (Fig. 4b), respectively, indicating very high correlation. When measurements were considered for each movement at each joint, the demonstrated smaller but still very highly or highly correlated values. For UE, the for shoulder movements ranged from 0.79 to 0.89 (flexion = 0.84, extension = 0.84, abduction = 0.86, internal rotation = 0.79 and external rotation = 0.89); for elbow, flexion was 0.77; for the forearm, pronation was 0.75 and supination was 0.73; and for wrist movements, it ranged from 0.62 to 0.88 (flexion = 0.86, extension = 0.68, radial deviation = 0.88 and ulnar deviation = 0.62). For LE, the for hip movements ranged from 0.69 to 0.93 (abduction = 0.93, adduction = 0.82, extension = 0.82, flexion = 0.90, internal rotation = 0.79 and external rotation = 0.69); for knee, flexion was 0.82; and for the ankle, dorsi-flexion was 0.92 and plantar-flexion was 0.93.
Figure 3.
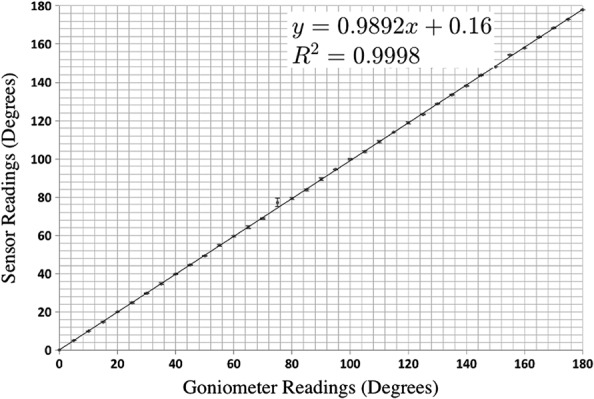
Plot of angles measured using goniometer against sensor applied onto arm of goniometer
Figure 4.
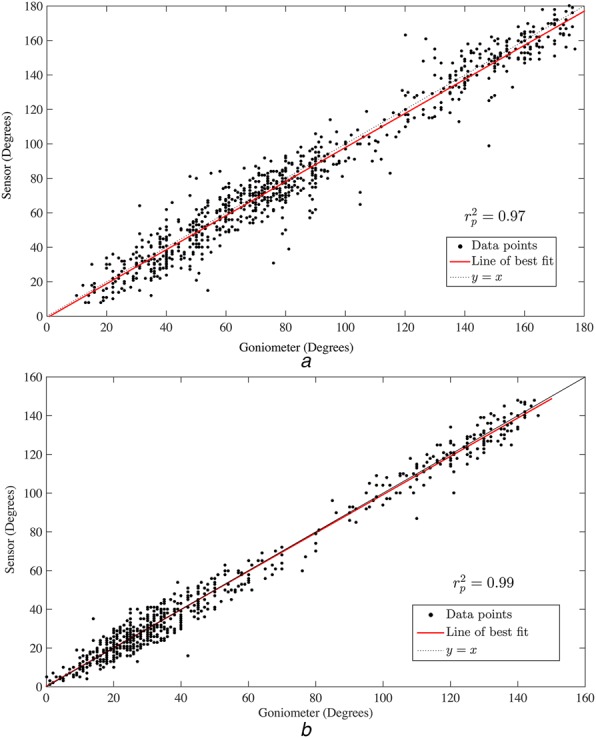
Scatter plot of angles using goniometer against sensor of major joints for both sides of
a UE
b LE (healthy)
As shown by the Bland–Altman plots, 95% of the differences in angle measured between the sensor system and goniometry for all movements in the major joints of the UE were generally ±20°, except for extension and ulnar deviation at the wrist joint, which were higher at ±30° (Fig. 5). For the major joints of the LE, 95% of the differences in angles measured between the sensor system and goniometry for all movements were generally better at ±10°, except for adduction, extension and flexion at the hip joint which were higher at < ±20° (Fig. 6).
Figure 5.
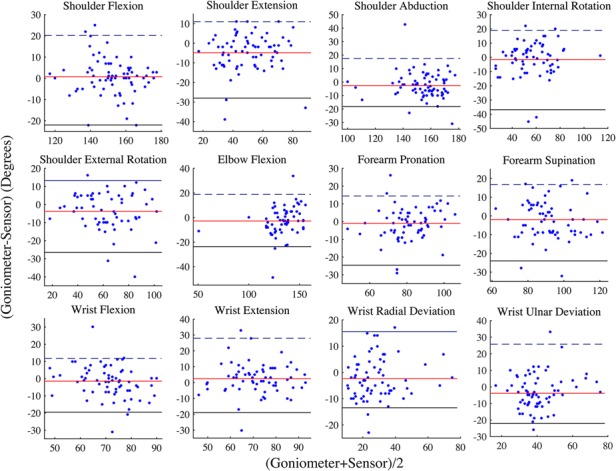
BA plots of diff against mean of angles measured using goniometer against sensor for both sides of UE (healthy)
Figure 6.
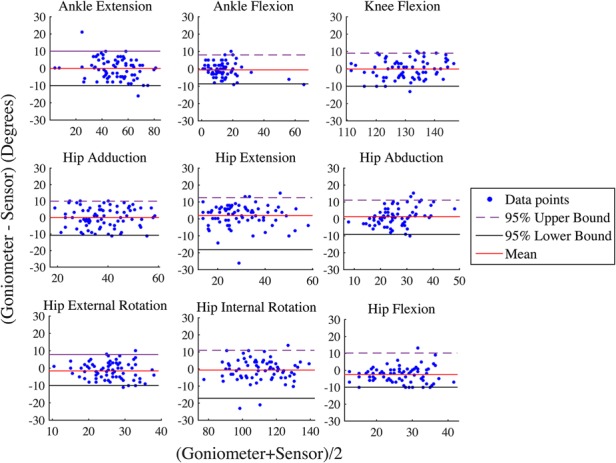
BA plots of diff against mean of angles measured using goniometer against sensor for both sides of LE (healthy)
4. Results (patients)
For this group of newly disabled inpatients, the for UE and LE assessments were 0.97 (Fig. 7a) and 0.96 (Fig. 7b), respectively, indicating very high correlation. When measurements were considered for each movement at each joint, the demonstrated smaller but still very highly correlated, or highly correlated values. For UE, the for shoulder movements ranged from 0.79 to 0.97 (flexion = 0.93, extension = 0.95, abduction = 0.97, internal rotation = 0.96 and external rotation = 0.79); for elbow, flexion was 0.97; for the forearm, pronation was 0.95 and supination was 0.93; and for wrist movements, it ranged from 0.42 to 0.79 (flexion = 0.42, extension = 0.79, radial deviation = 0.71 and ulnar deviation = 0.70). For LE, the for hip movements ranged from 0.73 to 0.98 (abduction = 0.95, adduction = 0.73, extension = 0.73, flexion = 0.84, internal rotation = 0.98 and external rotation = 0.77); for knee, flexion was 0.94; and for the ankle, dorsi-flexion was 0.89 and plantar-flexion was 0.95.
Figure 7.
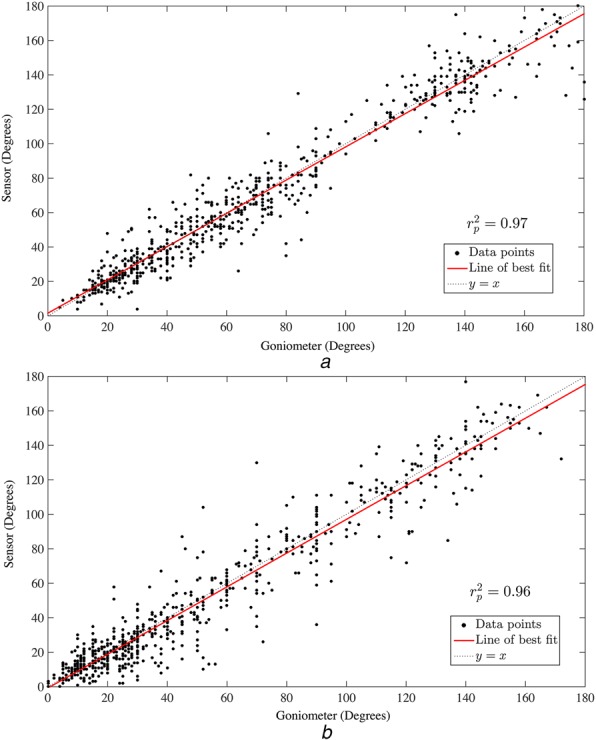
Scatter plot of angles using goniometer against sensor of major joints for both sides of UE and LE (patients)
a UE
b LE
The Bland–Altman plots in Figs. 8 and 9 show that 95% of the differences in angle measured between the sensor system and goniometry for all movements in the major joints of the UE were generally ±20°; except for shoulder internal rotation, elbow flexion and wrist extension which were higher at ±30° and shoulder abduction and wrist flexion which were highest at ±40° (Fig. 7). For the major joints of the LE, 95% of the differences in angles measured between the sensor system and goniometry for all movements were generally better at ±25°, except for adduction, extension and flexion at the hip joint which were higher at ±40° (Fig. 8).
Figure 8.
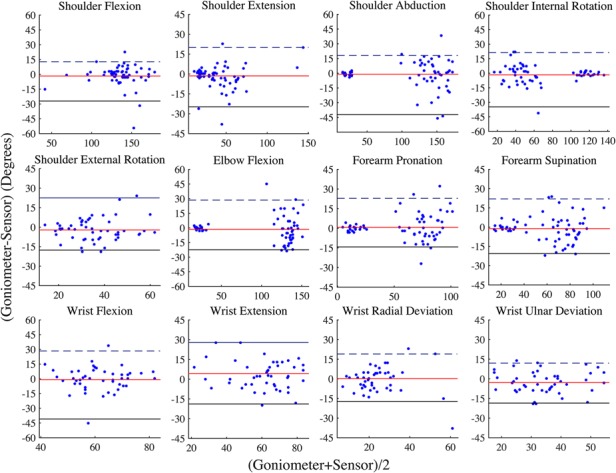
BA plots of diff against mean of angles measured using goniometer against sensor for both sides of UE (patients)
Figure 9.
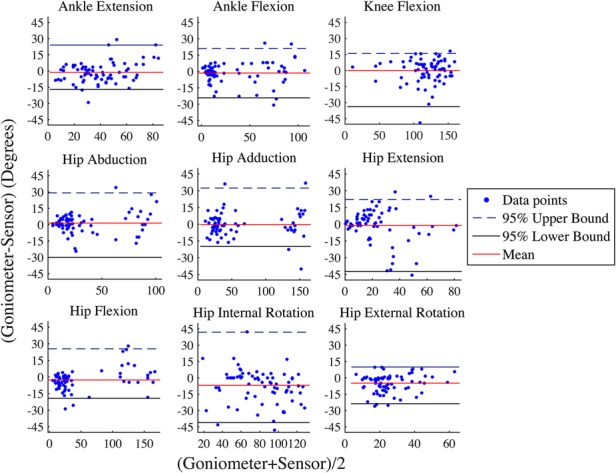
BA Plots of diff against mean of angles measured using goniometer against sensor for both sides of LE (patients)
5. Discussion
The ROM measurements using the new sensor system were highly correlated with goniometry based on the testings on healthy subjects and newly disabled patients. With respect to the mean angle between the two methods, 95% of the differences were <20° for most movements in the major joints of the UEs and <10° for most movements in the major joints of the LEs in healthy subjects; whereas in newly disabled patients, 95% of the differences were <20° for most movements in the major joints of the UEs and <25° for most movements in the major joints of the LEs. Although the 95% confidence limits of the difference of <20° for the UE and <10° for the LE appears high, previous studies using Bland–Altman analysis to compare the use of the goniometer with other validated methods of measuring ROM reported similar limits: Kolber and Hanney [20] found 95% limits of agreement of up to 20° between goniometry and digital inclinometry for shoulder ROM in healthy subjects, while Peeler and Anderson [21] found 95% limits of agreement of more than 10° between test and retest conducted by the same assessor using goniometry to measure knee ROM in healthy subjects. Since the sensor system had almost perfect correlation with the moving arm of a goniometer and a 95% limit of Bland–Altman agreement of ± 1%, the variations in ROM measured between sensors and manual goniometry is probably more due to the patient's joint movements during ROM measurement than sensor inaccuracy. A possible reason as to why the 95% limit of agreement was wider for UEs could be that the shoulder joint has more complex movements than the hip joint as the former involves scapula rotation, and the wrist joint has more complex movement than the ankle joint as the former is also involved in forearm supination and pronation. As to why the 95% limit of agreement was higher for LEs in newly disabled patients than in healthy subjects, the probable reason could be that the patient population had more painful conditions involving the LE (i.e. total knee replacement, femoral fractures and deep vein thrombosis) than the UE, which may have made it difficult for the patient to maintain the position of his LE joints while ROM was being manually measured using the goniometer. Another possible reason could be that the disabling conditions could have distorted the normal anatomy that the sensor algorithms were based on. To compensate for differing anatomies of disabled patients, the sensor system will be enhanced with a zeroing calibration procedure to take into account baseline limitations in ROM at rest when calculating active ROM. In addition, we have also tested to see if the correlation between sensor and goniometer readings were different between stroke and non-stroke patients and found that this is not statistically significantly different (p = 0.854).
The advantages of the sensor system are its speed, convenience and ease of use. Unlike conventional goniometry, the assessor only needs to be trained to apply the sensors correctly. On the other hand, goniometry requires extensive training of the assessor in the correct positioning of the goniometer fulcrum and movable arm for each movement. Moreover, the sensor system is more efficient because multiple movements and joints can be measured seamlessly without having to reapply the goniometer between each movement; and faster because the sensor system can complete a full four limb assessment in 10 min, whereas goniometry can take up to 2–3 times longer. Finally, in addition, if correctly applied, the sensor system eliminates the problem of inter-rater variability and subjectivity, which is an issue in ROM measurements [1]. The accompanying software can also now generate plots of ROM metrics (e.g. maximum active ROM, maximum angular velocity and maximum angular acceleration or deceleration) for each joint movement over repeated measurements, demonstrating time trends in ROM.
The strength of this validation study is its direct simultaneous comparison of angles measured using goniometry and the sensor system, eliminating the problems associated with test–retest repeated measurements and inter-rater variability which is considerable in ROM measurements [1]. Additionally, ROM by goniometry and the sensor system was measured by two independent assessors, although the measurements were performed at the same time. Other strengths of the study are the inclusion of all movements of all major joints in both UE and LEs, and the use of Bland–Altman analysis, which is the optimal method to compare two forms of measurements, and the use of actual newly disabled patients undergoing rehabilitation for validation. A limitation of this study is that the study population consisted predominantly of patients with LE disabilities and the accuracy of the sensor system for the UE could be poorer than currently measured for disabling conditions of the upper limbs such as Colles fractures.
6. Conclusion
In healthy subjects and newly disabled patients undergoing rehabilitation, ROM measurements using the new sensor system were highly correlated with those using goniometry. Considering the convenience, ease of use and efficiency of the sensor system, it has the potential of providing an alternative method for measuring ROM in limb joints that is as fast as visual inspection but with the objectivity and accuracy of goniometry in healthy persons and disabled patients for a wide range of rehabilitation situations.
7. Acknowledgments
The authors thank all staff and patients from Ang Mo Kio Thye-Hua Kwan Hospital that participated in the study.
8. Funding and declaration of interests
This study was supported by grants from the Cross Faculty Research Program, National University of Singapore and the Singapore Millennium Foundation. Conflict of interest: Dr Tay, Dr G. Koh and Dr Yen have a patent pending; US Provisional Patent Application No. 62/038,532 – An Apparatus and Method for Quantifying Rehabilitation Exercises Including the Detection of Motor Compensation. Dr Tay, Dr G. Koh, Dr Yen and Dr Kumar report that they are part of a start-up company that will aim to commercialise the system described in the Letter.
9 References
- 1.Gajdosik R.L., Bohannon R.W.: ‘Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity’, Phys. Ther., 1987, 67, pp. 1867–1872 [DOI] [PubMed] [Google Scholar]
- 2.Blonna D., Zarkadas P.C., Fitzsimmons J.S., O'Driscoll S.W.: ‘Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow’, Knee Surg. Sports Traumatol. Arthrosc., 2012, 20, pp. 1378–1385 (doi: ) [DOI] [PubMed] [Google Scholar]
- 3.Van De Pol R.J., Van Trijffel E., Lucas C.: ‘Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review’, J. Physiother., 2010, 56, pp. 7–17 (doi: ) [DOI] [PubMed] [Google Scholar]
- 4.Hellebrandt F.A., Duvall E.N., Moore M.L.: ‘The measurement of joint motion: part III. Reliability of goniometry’, Phys. Ther. Rev., 1949, 29, pp. 302–307 [Google Scholar]
- 5.Ferriero G., Vercelli S., Sartorio F., et al. : ‘Reliability of a smartphone-based goniometer for knee joint goniometry’, Int. J. Rehabil. Res., 2012, [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Hoffmann T., Russell T., Cooke H.: ‘Remote measurement via the internet of upper limb range of motion in people who have had a stroke’, J. Telemed. Telecare, 2007, 13, pp. 401–405 (doi: ) [DOI] [PubMed] [Google Scholar]
- 7.Chapleau J., Canet F., Petit Y., Laflamme G.Y., Rouleau D.M.: ‘Validity of goniometric elbow measurements: comparative study with a radiographic method’, Clin. Orthopaedics Relat. Res., 2011, 469, pp. 3134–3140 (doi: ) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Draper C.E., Chew K.T., Wang R., Jennings F., Gold G.E., Fredericson M.: ‘Comparison of quadriceps angle measurements using short-arm and long-arm goniometers: correlation with MRI’, PM&R, 2011, 3, pp. 111–116 [DOI] [PubMed] [Google Scholar]
- 9.Najafi B., Aminian K., Paraschiv-Ionescu A., Loew F., Büla C.J., Robert P.: ‘Ambulatory system for human motion analysis using a kinematic sensor: monitoring of daily physical activity in the elderly’, IEEE Trans. Biomed. Eng., 2003, 50, pp. 711–723 (doi: ) [DOI] [PubMed] [Google Scholar]
- 10.Liu K., Liu T., Shibata K., Inoue Y., Zheng R.: ‘Novel approach to ambulatory assessment of human segmental orientation on a wearable sensor system’, J. Biomech., 2009, 42, pp. 2747–2752 (doi: ) [DOI] [PubMed] [Google Scholar]
- 11.Gibbs P.T., Asada H.H.: ‘Wearable conductive fiber sensors for multi-axis human joint angle measurements’, J. Neuroeng. Rehabil., 2005, 2, (7), pp. 1743–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dejnabadi H., Jolles B.M., Aminian K.: ‘A new approach to accurate measurement of uniaxial joint angles based on a combination of accelerometers and gyroscopes’, IEEE Trans. Biomed. Eng., 2005, 52, pp. 1478–1484 (doi: ) [DOI] [PubMed] [Google Scholar]
- 13.Goodvin C., Park E.J., Huang K., Sakaki K.: ‘Development of a real-time three-dimensional spinal motion measurement system for clinical practice’, Med. Biol. Eng. Comput., 2006, 44, pp. 1061–1075 (doi: ) [DOI] [PubMed] [Google Scholar]
- 14.Watanabe T., Saito H.: ‘Tests of wireless wearable sensor system in joint angle measurement of lower limbs’. Conf. Proc. IEEE Engineering in Medicine Biology Society, Boston, MA, USA, September 2011, pp. 5469–5472 [DOI] [PubMed] [Google Scholar]
- 15.Lee W.W., Yen S.C., Tay A., et al. : ‘A smartphone-centric system for range of motion assessment in stroke patients’, IEEE J. Biomed. Health Inform., 2014, 18, (6), pp. 1839–1847 (doi: ) [DOI] [PubMed] [Google Scholar]
- 16.Clarkson H.M.: ‘Musculoskeletal assessment: joint range of motion and manual muscle strength’ (Lippincott Williams & Wilkins, USA, 2000, 2nd edn.) [Google Scholar]
- 17.Taylor R.: ‘Interpretation of the correlation coefficient: a basic review’, J. Diagn. Med. Sonography, 1990, 1, pp. 35–39 (doi: ) [Google Scholar]
- 18.Bland J.M., Altman D.G.: ‘Statistical methods for assessing agreement between two methods of clinical measurement’, Lancet., 1986, i, pp. 307–310 (doi: ) [PubMed] [Google Scholar]
- 19.Bland J.M., Altman D.G.: ‘Comparing methods of measurement: why plotting difference against standard method is misleading’, Lancet, 1995, 346, pp. 1085–1087 (doi: ) [DOI] [PubMed] [Google Scholar]
- 20.Kolber M.J., Hanney W.J.: ‘The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report’, Int. J. Sports Phys. Ther., 2012, 7, pp. 306–313 [PMC free article] [PubMed] [Google Scholar]
- 21.Peeler J., Anderson J.E.: ‘Reliability of the Ely's test for assessing rectus femoris muscle flexibility and joint range of motion’, J. Orthopaedic Res., 2008, 26, pp. 793–799 (doi: ) [DOI] [PubMed] [Google Scholar]


