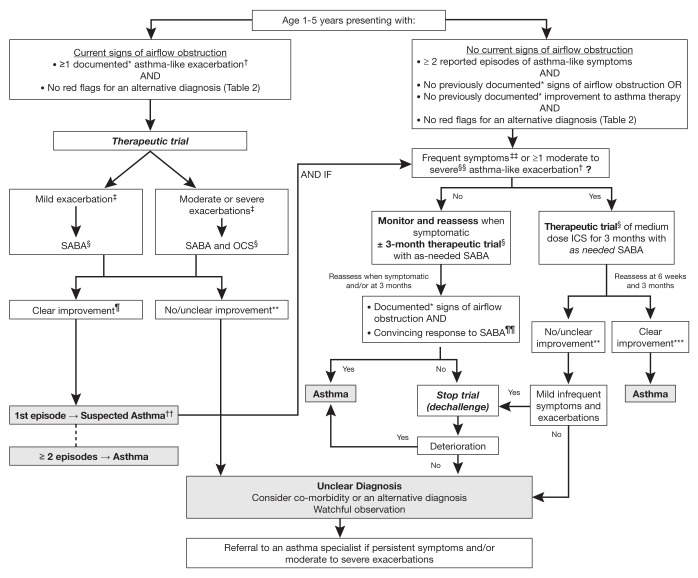
Figure 1).
Diagnosis algorithm for children one to five years of age. *Documentation by a physician or trained health care practitioner; †Episodes of wheezing with/without difficulty breathing; ‡Severity of an exacerbation documented by clinical assessment of signs of airflow obstruction, preferably with the addition of objective measures such oxygen saturation and respiratory rate, and/or validated score such as the Pediatric Respiratory Assessment Measure (PRAM) score; §See Table 3 for dosing; ¶Based on marked improvement in signs of airflow obstruction before and after therapy or a reduction of ≥3 points on the PRAM score, recognizing the expected time response to therapy; **A conclusive therapeutic trial hinges on adequate dose of asthma medication, adequate inhalation technique, diligent documentation of the signs and/or symptoms, and timely medical reassessment; if these conditions are not met, consider repeating the treatment or therapeutic trial; ††The diagnosis of asthma is based on recurrent (≥2) episodes of asthma-like exacerbations (documented signs) and/or symptoms. In case of a first occurrence of exacerbation with no previous asthma-like symptoms, the diagnostic of asthma is suspected and can be confirmed with re-occurrence of asthma-like symptoms or exacerbations with response to asthma therapy ; ‡‡≥8 days/month with asthma-like symptoms; §§Episodes requiring rescue oral corticosteroids (OCS) or a hospital admission; ¶¶In this age group, the diagnostic accuracy of parental report of a short-term response to as-needed short-acting β2-agonist (SABA) may be unreliable due to misperception and/or spontaneous improvement of another condition. Documentation of airflow obstruction and reversibility when symptomatic, by a physician or trained health care practitioner, is preferred; ***Based on 50% fewer moderate/severe exacerbations, shorter and milder exacerbations, and fewer, milder symptoms between episodes. ICS Inhaled corticosteroid