Abstract
Many of the treatment strategies for sigmoid diverticulitis are actually focusing on nonoperative and minimally invasive approaches. The aim of this systematic review was to evaluate the actual role of damage control surgery (DCS) in the treatment of generalized peritonitis caused by perforated sigmoid diverticulitis.
A literature search was performed in PubMed and Google Scholar for articles published from 1960 to July 2013. Comparative and noncomparative studies that included patients who underwent DCS for complicated diverticulitis were considered.
Acute Physiology and Chronic Health Evaluation score, duration of open abdomen, intensive care unit length of stay, reoperation, bowel resection performed at first operation, fecal diversion, method, and timing of closure of abdominal wall were the main outcomes of interest.
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses algorithm for the literature search and review, 10 studies were included in this systematic review. DCS was exclusively performed in diverticulitis patients with septic shock or requiring vasopressors intraoperatively. Two surgical different approaches were highlighted: limited resection of the diseased colonic segment with or without stoma or reconstruction in situ, and laparoscopic washing and drainage without colonic resection.
Despite the heterogeneity of patient groups, clinical settings, and interventions included in this review, DCS appears to be a promising strategy for the treatment of Hinchey III and IV diverticulitis, complicated by septic shock. A tailored approach to each patient seems to be appropriate.
INTRODUCTION
Generalized peritonitis as a consequence of complicated acute diverticulitis (AD) is rare and corresponds to stages III and IV of the Hinchey classification.1 Mortality is still high, up to 40% of cases, despite the progress in antibiotics regimens and fluid administration.2 Hartmann procedure (HP) has long been considered to be a safe treatment for this severe clinical condition, accounting for about a half of all patients undergoing surgery for complicated AD in Europe, mostly as an open procedure;3 however, more than 1/3 of the patients who undergo a HP do not have their stoma reversed within 1 year,4 if ever5 and when they have, they are exposed to the risk of a difficult surgical procedure due to the unrare sequela of the generalized peritonitis. Combined with improvements in medical support, this has led surgeons to consider whether resection with primary anastomosis (PA) or any other less-invasive surgical procedure could provide equivalent safety. Two multicenter trials,6,7 the latter aborted because of difficult accrual,8 found substantial equivalence between HP and PA groups in terms of morbidity, although patients with both purulent and fecal peritonitis were included. A recent systematic review and meta-analysis including 1041 patients, despite a vast heterogeneity of patients’ characteristics, suggested an advantage in terms of mortality and hospital stay in favor of PA.9
Patients with Hinchey III and IV with severe sepsis might benefit from damage control surgery (DCS).10 Initially described for the treatment of major abdominal injuries,11,12 indications for DCS have been extended to patients with necrotizing pancreatitis, severe peritonitis, or intraperitoneal hemorrhage.13
The aim of this systematic review was to evaluate the actual role of DCS in the treatment of generalized peritonitis caused by perforated sigmoid diverticulitis and determine whether there were any specific indications for one approach or another
METHODS
A systematic literature search was performed on PubMed and Google Scholar from January 1960 to July 2014. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses was followed. The following search strategies were used in PubMed:
damage[All Fields] AND (“prevention and control”[Subheading] OR (“prevention”[All Fields] AND “control”[All Fields]) OR “prevention and control”[All Fields] OR “control”[All Fields] OR “control groups”[MeSH Terms] OR (“control”[All Fields] AND “groups”[All Fields]) OR “control groups”[All Fields]) AND (“surgery”[Subheading] OR “surgery”[All Fields] OR “surgical procedures, operative”[MeSH Terms] OR (“surgical”[All Fields] AND “procedures”[All Fields] AND “operative”[All Fields]) OR “operative surgical procedures”[All Fields] OR “surgery”[All Fields] OR “general surgery”[MeSH Terms] OR (“general”[All Fields] AND “surgery”[All Fields]) OR “general surgery”[All Fields]) AND (“diverticulitis”[MeSH Terms] OR “diverticulitis”[All Fields])
damage[All Fields] AND (“prevention and control”[Subheading] OR (“prevention”[All Fields] AND “control”[All Fields]) OR “prevention and control”[All Fields] OR “control”[All Fields] OR “control groups”[MeSH Terms] OR (“control”[All Fields] AND “groups”[All Fields]) OR “control groups”[All Fields]) AND (“laparotomy”[MeSH Terms] OR “laparotomy”[All Fields]) AND (“diverticulitis”[MeSH Terms] OR “diverticulitis”[All Fields])
(“colon, sigmoid”[MeSH Terms] OR (“colon”[All Fields] AND “sigmoid”[All Fields]) OR “sigmoid colon”[All Fields] OR “sigmoid”[All Fields]) AND (“diverticulitis”[MeSH Terms] OR “diverticulitis”[All Fields]) AND damage[All Fields] AND (“prevention and control”[Subheading] OR (“prevention”[All Fields] AND “control”[All Fields]) OR “prevention and control”[All Fields] OR “control”[All Fields] OR “control groups”[MeSH Terms] OR (“control”[All Fields] AND “groups”[All Fields]) OR “control groups”[All Fields]) AND (“surgery”[Subheading] OR “surgery”[All Fields] OR “surgical procedures, operative”[MeSH Terms] OR (“surgical”[All Fields] AND “procedures”[All Fields] AND “operative”[All Fields]) OR “operative surgical procedures”[All Fields] OR “surgery”[All Fields] OR “general surgery”[MeSH Terms] OR (“general”[All Fields] AND “surgery”[All Fields]) OR “general surgery”[All Fields])
feculent [All Fields] AND (“peritonitis”[MeSH Terms] OR “peritonitis”[All Fields])
All titles and abstracts were assessed to select those focusing on DCS. Subsequently, the full text of the selected trials was independently screened by 2 authors (RC and GC) for eligibility.
When there was overlapping between multiple articles published by the same authors and no difference in the examined time, only the most recent trial was enclosed to avoid redundant counting. The PubMed function “related articles” were used to search further articles. The references of the included studies were evaluated for other potential trials missed by the screening process. Ethical approval for this study was not necessary because of its design consisting a systematic review of the literature.
Inclusion Criteria
We considered both comparative and noncomparative studies, which included patients who underwent DCS for complicated diverticulitis irrespectively of their size, publication status, or language. Comparative studies were included if they focused on selected outcomes of interest (Acute Physiology and Chronic Health Evaluation [APACHE] II score, duration of open abdomen, intensive care unit [ICU] day, reoperation, bowel resection performed at first operation, fecal diversion, method, and timing of closure of abdominal wall), irrespective of the type of surgical approach used for comparative group (laparoscopic or open).
Data Extraction
Included studies were reviewed and data were extracted by 2 blinded reviewers (RC and GC) using a standardized data extraction form.
Assessment of Risk of Bias in Included Studies
We assessed the methodological quality of the trials independently, without masking the trial names. The review authors performed the risk of bias assessment according to “The Cochrane Collaboration tool for assessing risk of bias.”14
RESULTS
Our comprehensive literature search identified 4550 records, of which 50 full texts were identified for further examination, while the others were excluded based on the titles and/or abstract. According to the inclusion criteria, 10 studies were selected for the current review and analysis. All studies were published in English (Figure 1).
FIGURE 1.
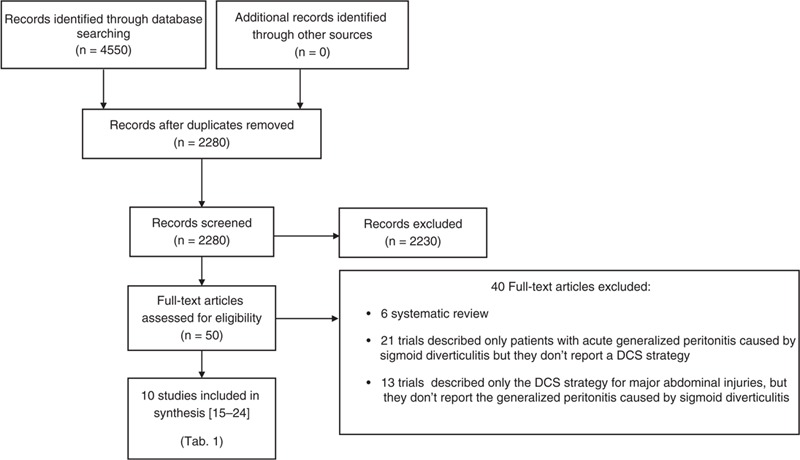
PRISMA flowchart of literature search. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Description of Studies
A detailed description of the characteristics of patients included in the 10 selected studies is presented in Table 1 .15–24
TABLE 1.
Characteristics of the Included Studies
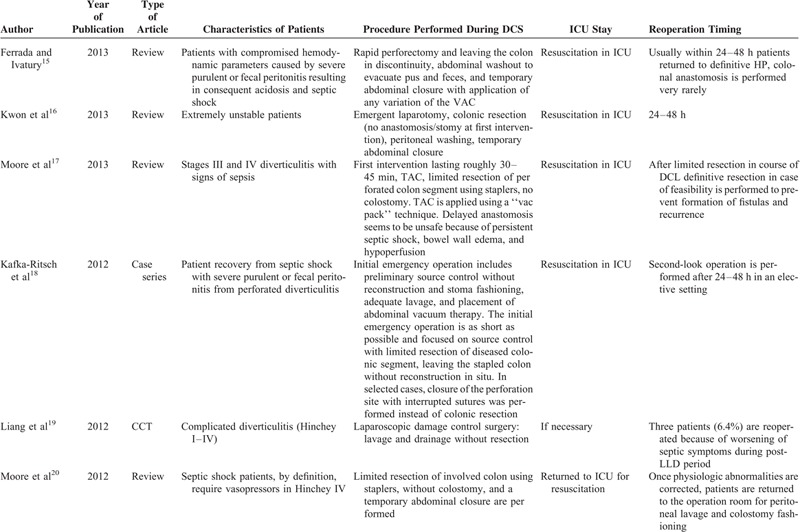
TABLE 1 (Continued).
Characteristics of the Included Studies
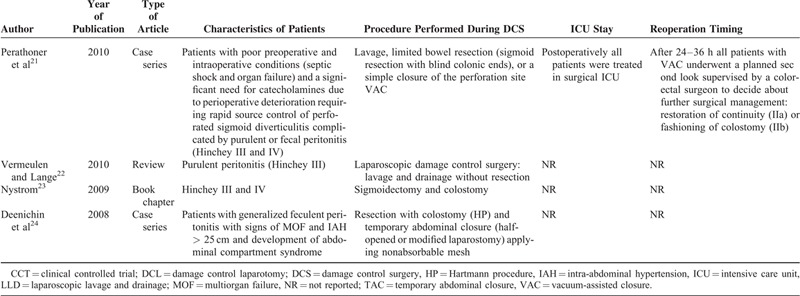
Only patients with septic shock caused by severe purulent (Hinchey III) or fecal (Hinchey IV) peritonitis15 and who required catecholamine administration because of perioperative general conditions15,16,20,21 underwent conventional DCS.
Definition of DCS
Two different DCS approaches have been described in the literature to treat acute peritonitis caused by diverticulitis.
The first, that is, conventional,15,16,18,20,21,24 is characterized by the shortest possible initial emergency operation focused on source control (limited resection of the diseased colonic segment) leaving the stapled remaining colon with or without a stoma or reconstruction in situ. In selected cases, instead of colonic resection, closure of the perforation site with interrupted sutures, adequate lavage, and temporary closure was performed. In all cases after 24–48 hours of reequilibration in the ICU, definitive surgical treatment was applied. The authors who followed this approach proposed different abdominal closure techniques: most recommended temporary abdominal closure while a few preferred vacuum-assisted closure (VAC).15,21
The second consists laparoscopic abdominal washing and drainage only, without resection.19,24 The proponents of washing and drainage19,24 considered these procedures as definitive surgery and reintervention was performed only in case of postoperative complications.19 Moore et al20 did not consider this technique as DCS and reserved it only for patients with Hinchey III without septic shock.
Patients Who Underwent DCS
Conventional DCS15,16,18,20,21,24 was performed in patients with septic shock defined as hemodynamically unstable patients who required immediate inotropic or vasopressor support15,16,20,21 and generalized purulent or fecal peritonitis; on the contrary, patients who underwent laparoscopic DCS had only generalized purulent or fecal peritonitis and were not hemodynamically unstable.19,22 Kown et al16 recommended the HP in unstable but controllable patients, while DCS should be limited to extremely unstable patients.
DCS involved a 3-staged approach—stage I: an abbreviated initial operative procedure with temporary abdominal closure; stage II: continued resuscitation and management of physiologic and acid–base derangements; and stage III: definitive treatment and closure.25
Subgroup analysis for type of abbreviated initial operative procedure with temporary abdominal closure (stage I of DCS) revealed that the majority of surgeons insisted on limited resection of diseased colon. Both Kafka-Ritsch et al18 and Perathoner et al21 left the colon stapled-off in situ without reconstruction in 45 of 51 cases. In the remaining, selected cases (6/51), the perforation site was closed with interrupted sutures without colonic resection.15,18 Other authors performed colonic resection with colostomy in all cases (HP).24 According to Ferrada and Ivatury,15 Kwon et al,16 and Moore et al,20 treatment should be tailored: “a limited colon resection of the inflamed colon is performed using staplers, with no colostomy.” Ferrada and Ivatury,15 Kwon et al,16 Kafka-Ritsch et al,18 and Perathoner et al21 preferred temporary abdominal VAC.
Subgroup analysis for recovery in ICU (stage II of DCS) revealed that after surgery, all patients were admitted to ICU for resuscitation. The duration of ICU ranged from 24 to 48 hours in all reports.15–24
Subgroup analysis for type of secondary procedures (stage III of DCS) showed that bowel continuity restoration or colostomy was performed by planned relaparotomy21 or on-demand relaparotomy20 and the choice was based on surgeon's preference.
Moreover, our review failed to determine whether any distinct physiologic parameters (eg, APACHE and Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity [POSSUM]) were useful to triage patients into receiving DCS versus other treatment.
DISCUSSION
The goal of DCS is the same as in trauma surgery: the initial emergency operation is to be kept as short as possible and focused on limiting the physiological insult.
The concept of DCS is based on a sequence of key phases25: short initial surgery, ICU for resuscitation, and return to the operating room as soon as normal or near-normal physiology is reached for the definitive operation. In trauma patients, this multistage approach is first of all performed to avoid or correct the lethal triad of hypothermia, acidosis, and coagulopathy,26 particularly well suited in patients with critical hemodynamic conditions, excessive peritoneal edema, difficulty to obtain a definitive control of the source of sepsis, incomplete debridement of necrotic tissue, uncertainty about bowel viability, uncontrolled bleeding, and massive abdominal wall loss.27 The goal of DCS in nontrauma patients is to obtain the same reduction of mortality. Some authors28 prefer the terms “advanced open operative treatment of peritonitis” or “aggressive method” terms29 instead of DCS. This approach is in accordance with the American Society of Colon and Rectal Surgeons practice parameters for sigmoid diverticulitis: minimum resection and diversion in urgent and emergent cases are generally required.30 Perathoner et al21 and Kafka-Ritsch et al18 underlined the fact that this kind of treatment should be applied only to patients with colic perforation. Others support that laparoscopy can be offered to all patients with complicated diverticulitis ranging from Hinchey stages I–IV.19
This review showed that DCS for treatment of peritonitis caused by complicated colon diverticulitis is not always applied according to the same criteria and methods. The results are quite inconsistent, likely because of the innate heterogeneity of patient groups, presentations, and operations. The extreme heterogeneity of indications and procedures make it difficult to analyze this procedure systematically. Nevertheless, it is possible to identify the pros and cons of the different approaches. Although much has been written over the last 50 years, only 2 randomized controlled trial have been performed.31,32 In both the studies, one of the arms was a precursor to DCS. Analysis of the published articles demonstrated 2 different surgical approaches, nonetheless not yet compared between themselves. This review showed that DCS is not a new strategy for the management of sepsis caused by diverticulitis, although distinctly different management DCS approaches are presented. Laparoscopy might have a role as DCS only in hemodynamically stable septic peritonitis unresponsive to medical or percutaneous treatment, with lavage/drainage operation but which needs to be validated for both purulent and fecal peritonitis. The question is if inclusion of the concepts, today widely approved, of trauma DCS in the guidelines for diverticulitis, should contribute to standardization of the therapeutic protocols. In the future, there is need to design longitudinal prospective studies apt to prove the results (already obtained for trauma surgery) in the septic complications of AD. The results of 3 ongoing trials are largely awaited (Ladies, Scandiv, and LapLAND trials).33–35
CONCLUSIONS
Our literature review showed that there was an extreme heterogeneity in the performance of DCS for treatment of acute generalized peritonitis caused by sigmoid diverticulitis. Also, the review failed to determine specific physiologic parameters (eg, APACHE, POSSUM, …) that could be used to triage patients to receive DCS versus other treatment. DCS is not a new strategy for the management of sepsis caused by diverticulitis, although distinctly different management DCS approaches are presented. The only new procedure is laparoscopic lavage for perforated diverticulitis (grade III). Clearly, an individual tailored approach to each patient might be appropriate depending on the patient's status.
Footnotes
Abbreviations: AD = acute diverticulitis, APACHE = Acute Physiology and Chronic Health Evaluation, DCS = damage control surgery, HP = Hartmann procedure, ICU = intensive care unit, PA = primary anastomosis, POSSUM = Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg 1979; 12:85–109. [PubMed] [Google Scholar]
- 2.Gilg M, Schweizer W, Maddern G, et al. Outcome of diffuse faecal and purulent peritonitis following colonic perforation. Dig Surg 1992; 9:72–75. [Google Scholar]
- 3.Sartelli M, Catena F, Ansaloni L, et al. Complicated intra-abdominal infections in Europe: preliminary data from the first three months of the CIAO Study. World J Emerg Surg 2012; 7:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riansuwan W, Hull TL, Millan MM, et al. Nonreversal of Hartmann's procedure for diverticulitis: derivation of a scoring system to predict nonreversal. Dis Colon Rectum 2009; 52:1400–1408. [DOI] [PubMed] [Google Scholar]
- 5.Binda GA, Arezzo A, Serventi A, et al. Multicentre observational study of the natural history of left-sided acute diverticulitis. Br J Surg 2012; 99:276–285. [DOI] [PubMed] [Google Scholar]
- 6.Oberkofler CE, Rickenbacher A, Raptis DA, et al. A multicenter randomized clinical trial of primary anastomosis or Hartmann's procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg 2012; 256:819–826. [DOI] [PubMed] [Google Scholar]
- 7.Binda GA, Karas JR, Serventi A, et al. Study Group on Diverticulitis. Primary anastomosis vs non restorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis 2012; 14:1403–1410. [DOI] [PubMed] [Google Scholar]
- 8.Binda GA, Serventi A, Puntoni M, et al. Primary anastomosis versus Hartmann's procedure for perforated diverticulitis with peritonitis: an impracticable trial. Ann Surg 2014; 0:1. [DOI] [PubMed] [Google Scholar]
- 9.Cirocchi R, Trastulli S, Desiderio J, et al. Treatment of Hinchey stage III-IV diverticulitis: a systematic review and meta-analysis. Int J Colorectal Dis 2013; 28:447–457. [DOI] [PubMed] [Google Scholar]
- 10.Moore FA, Catena F, Moore EE, et al. Position paper: management of perforated sigmoid diverticulitis. World J Emerg Surg 2013; 8:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rotondo MF, Schwab CW, McGonigal MD, et al. “Damage control”: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993; 35:375–382. [PubMed] [Google Scholar]
- 12.Mosenthal AC, Murphy PA. Trauma care and palliative care: time to integrate the two? J Am Coll Surg 2003; 197:509–516. [DOI] [PubMed] [Google Scholar]
- 13.Finlay IG, Edwards TJ, Lambert AW. Damage control laparotomy. Br J Surg 2004; 91:83–85. [DOI] [PubMed] [Google Scholar]
- 14.The Cochrane Collaboration, Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 2011; www.cochrane-handbook.org. [Google Scholar]
- 15.Ferrada P, Ivatury RR. The management of diverticular disease of the colon. Cameron JL, Cameron AM. Current Surgical Therapy. 11th ed. Philadelphia: Saunders; 2013. [Google Scholar]
- 16.Kwon E, Browder T, Fildes J. Surgical management of fulminant diverticulitis. Curr Surg Rep 2013; 2:40. [Google Scholar]
- 17.Moore FA, Coimbra R, Davis JW, et al. Mandatory exploration is not necessary for patients with acute diverticulitis and free intraperitoneal air. J Trauma Acute Care Surg 2013; 74:1376–1377. [DOI] [PubMed] [Google Scholar]
- 18.Kafka-Ritsch R, Birkfellner F, Perathoner A, et al. Damage control surgery with abdominal vacuum and delayed bowel reconstruction in patients with perforated diverticulitis Hinchey III/IV. J Gastrointest Surg 2012; 16:1915–1922. [DOI] [PubMed] [Google Scholar]
- 19.Liang S, Russek K, Franklin ME., Jr Damage control strategy for the management of perforated diverticulitis with generalized peritonitis: laparoscopic lavage and drainage vs. laparoscopic Hartmann's procedure. Surg Endosc 2012; 26:2835–2842. [DOI] [PubMed] [Google Scholar]
- 20.Moore FA, Moore EE, Burlew CC, et al. Western Trauma Association critical decisions in trauma: management of complicated diverticulitis. J Trauma Acute Care Surg 2012; 73:1365–1371. [DOI] [PubMed] [Google Scholar]
- 21.Perathoner A, Klaus A, Mühlmann G, et al. Damage control with abdominal vacuum therapy (VAC) to manage perforated diverticulitis with advanced generalized peritonitis—a proof of concept. Int J Colorectal Dis 2010; 25:767–774. [DOI] [PubMed] [Google Scholar]
- 22.Vermeulen J, Lange JF. Treatment of perforated diverticulitis with generalized peritonitis: past, present, and future. World J Surg 2010; 34:587–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nystrom PO. Schein M, Paul R, Ahmad A. Part B: the operation: chapter 26 acute diverticulitis. Schein's Common Sense Emergency Abdominal Surgery 3rd ed.New York, NY: Springer; 2009. 277–288. [Google Scholar]
- 24.Deenichin GP, Dimov RS, Stefanov CS, et al. Acute perforated diverticulitis of the colon as a rare cause for development of abdominal compartment syndrome. Folia Med (Plovdiv) 2008; 50:32–36. [PubMed] [Google Scholar]
- 25.Rodning KJ, Rodning CB, Rodning SP. “Keys to the Kingdom:” ritualism in the surgical disciplines. J Am Soc Abdom Surgeons 2011/2012; http://www.abdominalsurg.org/journal/2012/http://www.abdominalsurg.org/journal/2012/. Accessed July 2014. [Google Scholar]
- 26.Martini WZ. Coagulopathy by hypothermia and acidosis: mechanisms of thrombin generation and fibrinogen availability. J Trauma 2009; 67:202–208. [DOI] [PubMed] [Google Scholar]
- 27.Wittmann DH, Schein M, Condon RE. Management of secondary peritonitis. Ann Surg 1996; 224:10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holzheimer RG, Gathof B. Re-operation for complicated secondary peritonitis—how to identify patients at risk for persistent sepsis. Eur J Med Res 2003; 8:125–134. [PubMed] [Google Scholar]
- 29.Koroukov B, Damyanov D, Stoyanov S. Planned relaparotomy and laparostomy—“aggressive methods” in the treatment of diffuse purulent peritonitis. Med Health Sci J 2012; 13:58–68. [Google Scholar]
- 30.Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 2014; 57:284–294. [DOI] [PubMed] [Google Scholar]
- 31.Zeitoun G, Laurent A, Rouffet F, et al. French Associations for Surgical Research. Multicentre, randomized clinical trial of primary versus secondary sigmoid resection in generalized peritonitis complicating sigmoid diverticulitis. Br J Surg 2000; 87:1366–1374. [DOI] [PubMed] [Google Scholar]
- 32.Kronborg O. Treatment of perforated sigmoid diverticulitis: a prospective randomized trial. Br J Surg 1993; 80:505–507. [DOI] [PubMed] [Google Scholar]
- 33.Laparoscopic Peritoneal Lavage or Resection for Generalised Peritonitis for Perforated Diverticulitis: A Nationwide Multicenter Randomised Trial. http://clinicaltrials.gov/show/NCT01317485 Accessed July 2014 [Google Scholar]
- 34.Scandinavian Diverticulitis Trial. Laparoscopic Lavage vs Primary Resection as Treatment for Perforated Diverticulitis. A Randomized Prospective Multicenter Trial. http://www.clinicaltrials.gov/show/NCT01047462 Accessed July 2014 [Google Scholar]
- 35.Laparoscopic Lavage for Acute Non-Faeculant Diverticulitis (LapLAND). http://www.clinicaltrials.gov/ct2/show/NCT01019239?term=LapLAND&rank=1 Accessed July 2014 [Google Scholar]


