Abstract
Dementia increases the risk of morbidity and mortality in hospitalized patients. However, information on the potential effects of dementia on the risks of acute organ dysfunction, severe sepsis and in-hospital mortality, specifically among inpatients with chronic obstructive pulmonary disease (COPD), is limited.
The observational analytic study was inpatient claims during the period from 2000 to 2010 for 1 million people who were randomly selected from all of the beneficiaries of the Taiwan National Health Insurance in 2000. In total, 1406 patients with COPD and dementia were admitted during the study period. Hospitalized patients with COPD and free from a history of dementia were randomly selected and served as control subjects (n = 5334). The patient groups were matched according to age (±3 years), gender, and the year of admission, with a control/dementia ratio of 4. Only the first-time hospitalization data for each subject was analyzed. Logistic regression models were used to calculate the odds ratio (OR) of outcome measures (acute organ dysfunction, severe sepsis, and mortality), controlling for confounding factors (age, sex, comorbidity, infection site, hospital level, and length of stay).
In COPD patients with dementia, the incidence rate of severe sepsis and hospital mortality was 17.1% and 4.8%, respectively, which were higher than the controls (10.6% and 2.3%). After controlling for potential confounding factors, dementia was found to significantly increase the odds of severe sepsis and hospital mortality with an adjusted OR (OR) of 1.38 (95% confidence interval [CI] 1.10–1.72) and 1.69 (95% CI 1.18–2.43), respectively. Dementia was also significantly associated with an increased OR of acute respiratory dysfunction (adjusted OR 1.39, 95% CI 1.09–1.77).
In hospitalized COPD patients, the presence of dementia may increase the risks of acute respiratory dysfunction, severe sepsis, and hospital mortality, which warrants the attention of health care professionals.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a progressive disease characterized by airflow limitation, which cannot be fully reversed.1 The hospitalization rate of patients with COPD was estimated at 53.9 per 10,000 people, and the mortality rate of patients with COPD has increased 2.5% per year for men in Taiwan since 1995.2 Many studies have found that patients with COPD have significant cognitive impairments.3,4 A previous clinical trial reported that moderate-to-severe cognitive impairment occurred in 42% of patients with COPD compared with 14% in controls.4 The Mayo Clinic Study of Aging revealed in patients with COPD between 70 and 89-years old, the prevalence of mild cognitive impairment was approximately 27% compared with 15% in controls.5
According to previous studies,6–9 patients with cognitive impairments have an increased risk of hospitalization, a poor prognosis and a limited life expectancy. A recent study10 found that older patients with dementia who are hospitalized have increased risks of acute organ dysfunction, severe sepsis, and hospital mortality. According to these data, mortality may be increased in patients with cognitive dysfunction and dementia.
Despite the above findings, it is unclear whether dementia may still contribute additional risks to hospitalized patients with COPD who may have experienced a poor prognosis. We hypothesized that patients with COPD and dementia had poorer prognosis after admission compared with patients with COPD without dementia. Therefore, our study aims to investigate whether hospitalized patients with COPD and dementia are at increased risks of acute organ dysfunction, severe sepsis, or death. In this retrospective, population-based, cohort study, we investigated the characteristics of hospitalized patients with COPD and compared the risks of acute organ dysfunction, severe sepsis, and hospital mortality between patients with or without dementia. We also measured the resource use including the following life support treatments: care in the Intensive care unit, vasopressor using, hemodialysis, and mechanical ventilation in hospitalized patients with COPD.
MATERIALS AND METHODS
Ethics Statement
This observational analytic study was conducted by using unidentifiable claims database provided by the Department of Health, Taiwan, and the protocol had been reviewed and approved by its review committee and the principal investigator was requested to sign the agreement upon compliance with the Computer-Processed Personal Data Protection Act11 during proposal application. In addition, the policy of our institution review board is consistent with the principles of the Declaration of Helsinki. This study was approved by the Institutional Review Board of the Chi Mei Medical Center (IRB no. 10403-E05).
Source of Data
Taiwan launched a single-payer National Health Insurance (NHI) program in March 1995. The National Health Insurance Research Database, a medical claims database, was established and used for research purposes. The National Health Insurance Research Database contains all inpatient and outpatient claims data from the NHI Program in Taiwan, including patients’ demographic characteristics, disease diagnoses, prescription records, and medical expenditures. Approximately 99% of the total population in Taiwan was enrolled in the NHI Program. In this study, we analyzed the claim data of 1 million beneficiaries (from January 1, 2000 to December 31, 2010) randomly sampled from all of the beneficiaries registered in 2000.
Study Groups
In the present study, the definition of a hospitalized patient with COPD was a patient with a discharge diagnosis of COPD (ICD-9-CM codes: 490–492, 496) between January 1, 2000 and December 31, 2010 and older than 40 years. Patients with COPD and a history of severe mental disorders (ICD-9-CM codes 291–298) were excluded. These conditions included the following disease: alcohol-induced mental disorders, drug-induced mental disorders, transient mental disorders due to conditions classified elsewhere, persistent mental disorders due to conditions classified elsewhere, schizophrenic disorders, episodic mood disorders, delusional disorders, and other nonorganic psychoses.12 During the study period, one or more readmission events may have occurred for the same patient; only the data from the first-time hospitalization record for COPD was analyzed to ensure the independence of observations. In total, 16,945 patients with COPD were retrieved and analyzed (Figure 1).
FIGURE 1.
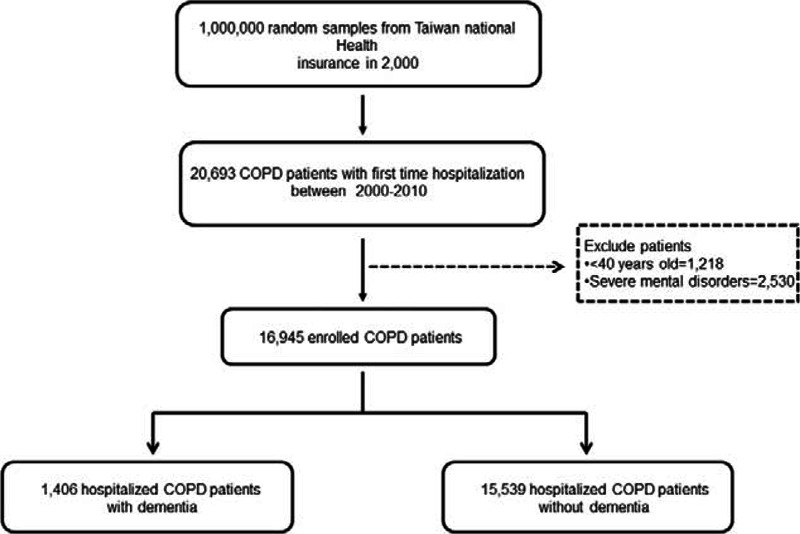
Flow chart of patients included in the study.
Dementia (diagnosed before hospitalization) was defined according to the diagnostic codes for senile or presenile organic psychotic condition (ICD-9-CM code 290) or Alzheimer disease (ICD-9-CM code 331.0). With the defined diagnostic criteria, we identified 1406 patients with COPD who had a history of dementia during the period between January 1, 1997 and the date of the first COPD-related admission from 2000 to 2010. The control subjects were selected from the remaining patients with COPD who had no history of dementia and were matched to the dementia patients by age (±3 years), gender, and the year of admission. The dementia:control ratio was 1:4. In total of 15,539 COPD patients without dementia were selected as controls.
Outcome Measures
Three outcome measures were investigated, including hospital mortality, severe sepsis, and acute organ dysfunction. The selection criteria for severe sepsis have been validated in a previous study.10 To define cases of severe sepsis, we used ICD-9-CM codes for both bacterial and fungal infections.13 These criteria have been used in other studies.10 The diagnostic codes for acute organ dysfunction are listed in S1 Table (see Table, Supplemental Content, which illustrates the diagnostic codes for acute organ dysfunction). As previously described in detail,10 only ICD-9-CM code 584 (excluding 580, 586, and 39.95) was used for acute renal dysfunction in this study.
Statistical Analysis
We described the demographic characteristics of the patients, including age, gender, comorbidities, infection site, hospital level, and length of hospital stay. Life-support treatments included hemodialysis, vasopressors, mechanical ventilation, and intensive care during the initial COPD admission.
Continuous variables are presented as the means (standard deviations), and discrete variables are presented as counts and percentages. We used Chi-square tests for comparing categorical variables and t tests for comparing continuous variables. The statistical significance was inferred at a 2-sided P value of < 0.05. The specific effects of dementia on the individual outcome measures, including acute organ dysfunction (cardiovascular, respiratory, renal, hepatic, neurologic, hematologic, and metabolic), severe sepsis, and hospital mortality, were assessed with multivariable logistic regressions adjusting for all the baseline characteristics (ie, age, sex, comorbidities, infection status, hospital level, life-support measures, and length of hospital stay). We also constructed separate logistic regression models to assess factors associated with the respiratory failure, severe sepsis, and hospital mortality outcomes, using dementia and various baseline covariates. All of the statistical analyses were performed using the Statistical Analysis Software (SAS) System, version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
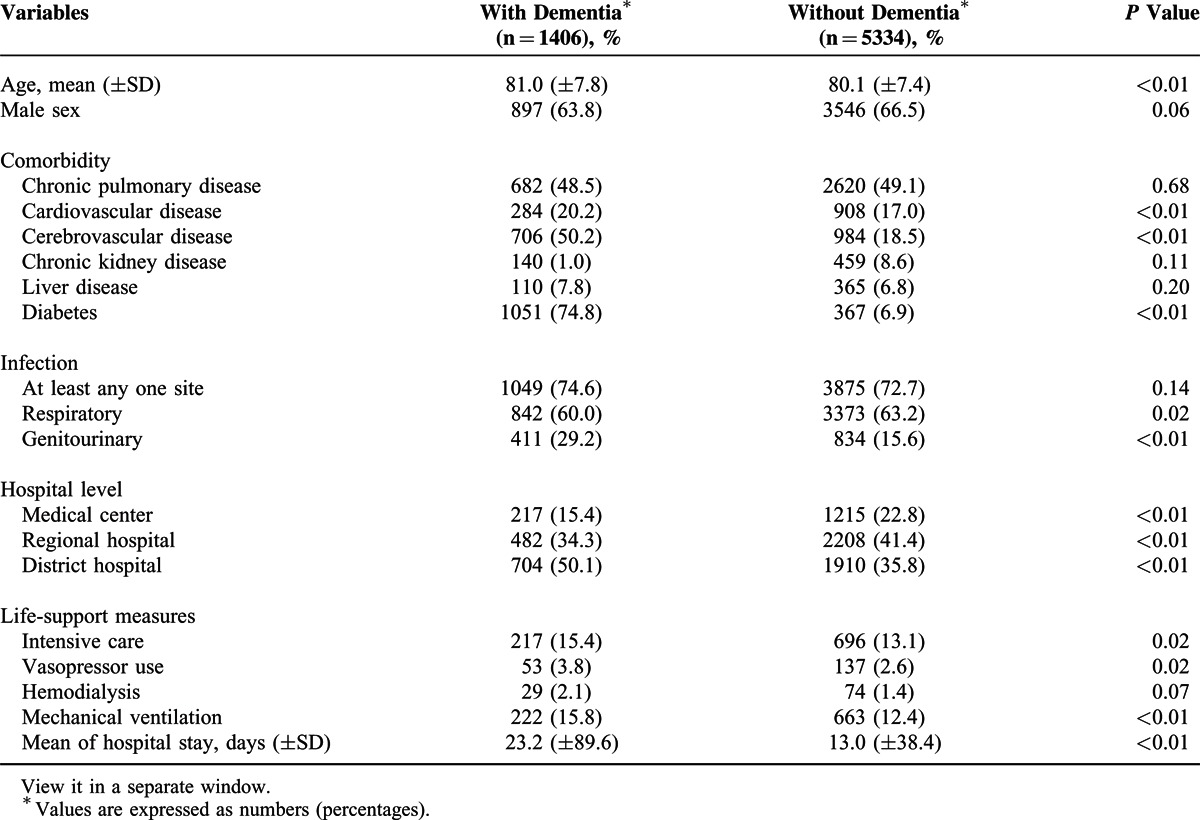
The characteristics and resource uses of the study subjects are shown in Table 1. The mean age of patients with COPD and dementia was 81 ± 7.8 years and were predominantly male (64%) with more prevalent in comorbidities and longer length of hospital stay than patients with COPD only. The patients with COPD and dementia had a higher prevalence of cardiovascular disease, cerebrovascular disease, chronic kidney disease, liver disease, and diabetes. Additionally, they had a slightly higher prevalence of infection than the control group (74.6% vs 72.7%). In contrast, patients with COPD and dementia were less likely to be hospitalized in medical centers compared with the control patients. More than 50% of patients with COPD and dementia were admitted to district hospitals due to COPD. Further, patients with COPD and dementia used significantly more life-sustaining resources, including intensive care, vasopressor use, hemodialysis, and mechanical ventilation and had longer hospital lengths of stay (23.2 vs 13.0 days).
TABLE 1.
Baseline Characteristics and Resource Uses of the Study Population
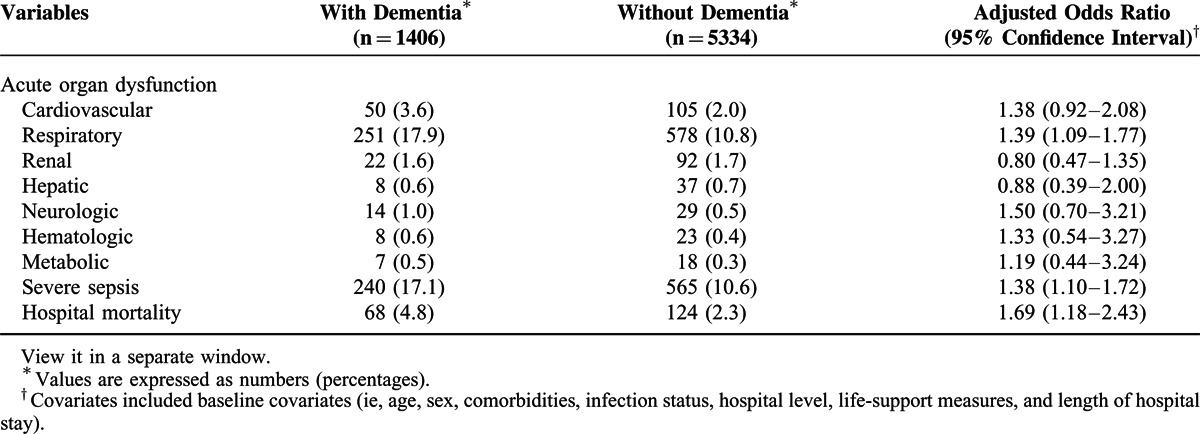
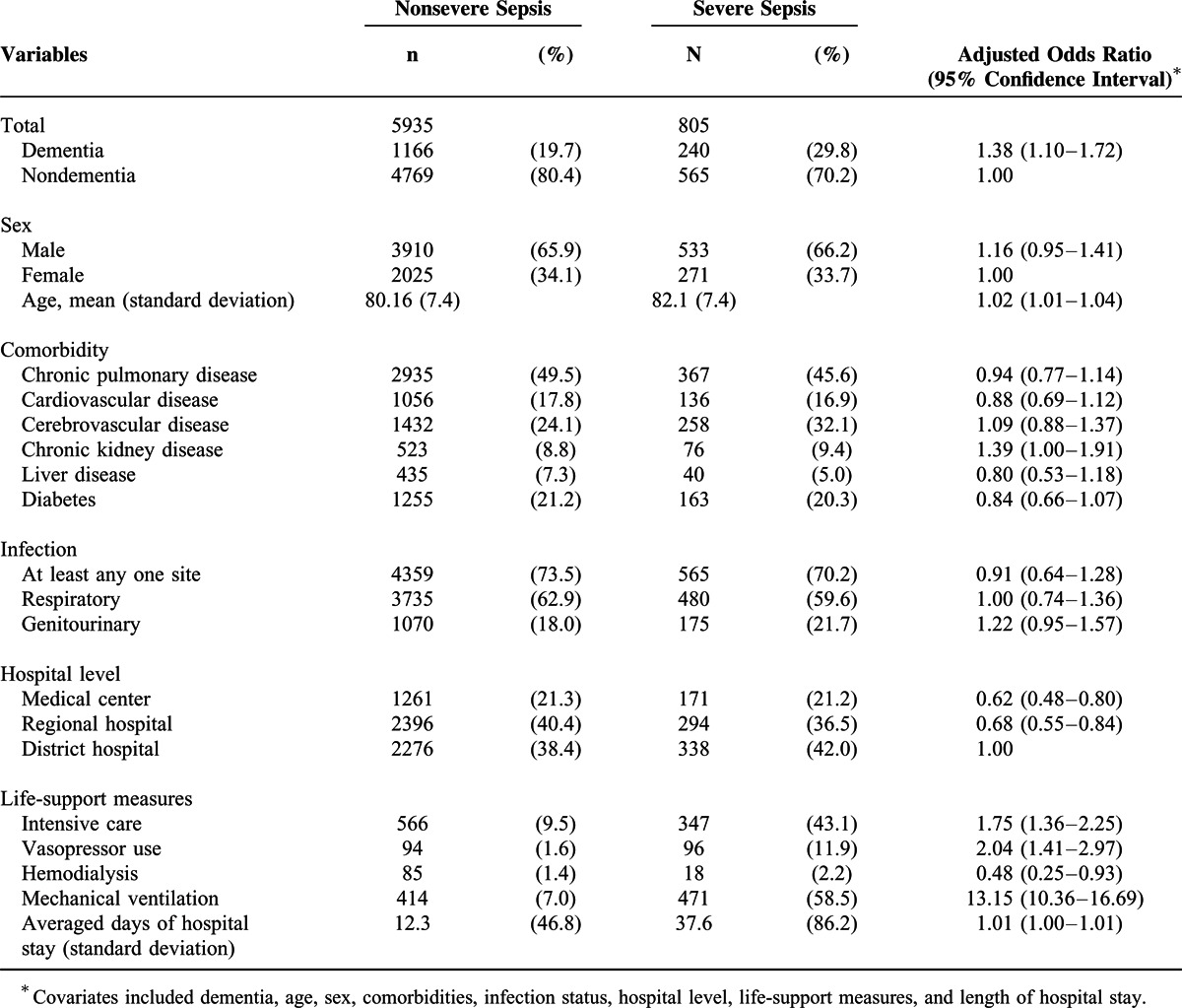
The risk of acute organ dysfunction of the respiratory system was higher in the patients with COPD and dementia than in control subjects. After adjusting for age, sex, comorbidities, infection status, hospital level, life-support measures, and length of hospital stay, the adjusted odds ratio (OR) was 1.39 (95% confidence interval [CI] 1.09–1.77) for respiratory failure (Table 2). Except for the respiratory system, the risks of acute dysfunction on the cardiovascular, renal, hepatic, neurologic, hematologic, and metabolic systems were essentially the same between the 2 groups. Further, after controlling for all baseline covariates, patients with COPD and dementia had a 38% higher risk of severe sepsis (Table 2, adjusted OR 1.38, 95% CI 1.10–1.72).
TABLE 2.
Effects of Dementia on the Risk of Acute Organ Dysfunction, Severe Sepsis, and Hospital Mortality in Patients With COPD
The potential factors associated with respiratory failure, severe sepsis, and hospital mortality in patients with COPD were shown in Tables 3–5, respectively. Besides dementia, factors associated with these clinical outcomes included age, cerebrovascular disease, chronic kidney disease, and length of hospital stay, after adjusting for all baseline characteristics.
TABLE 3.
Factors Associated With Respiratory Failure in Patients With COPD
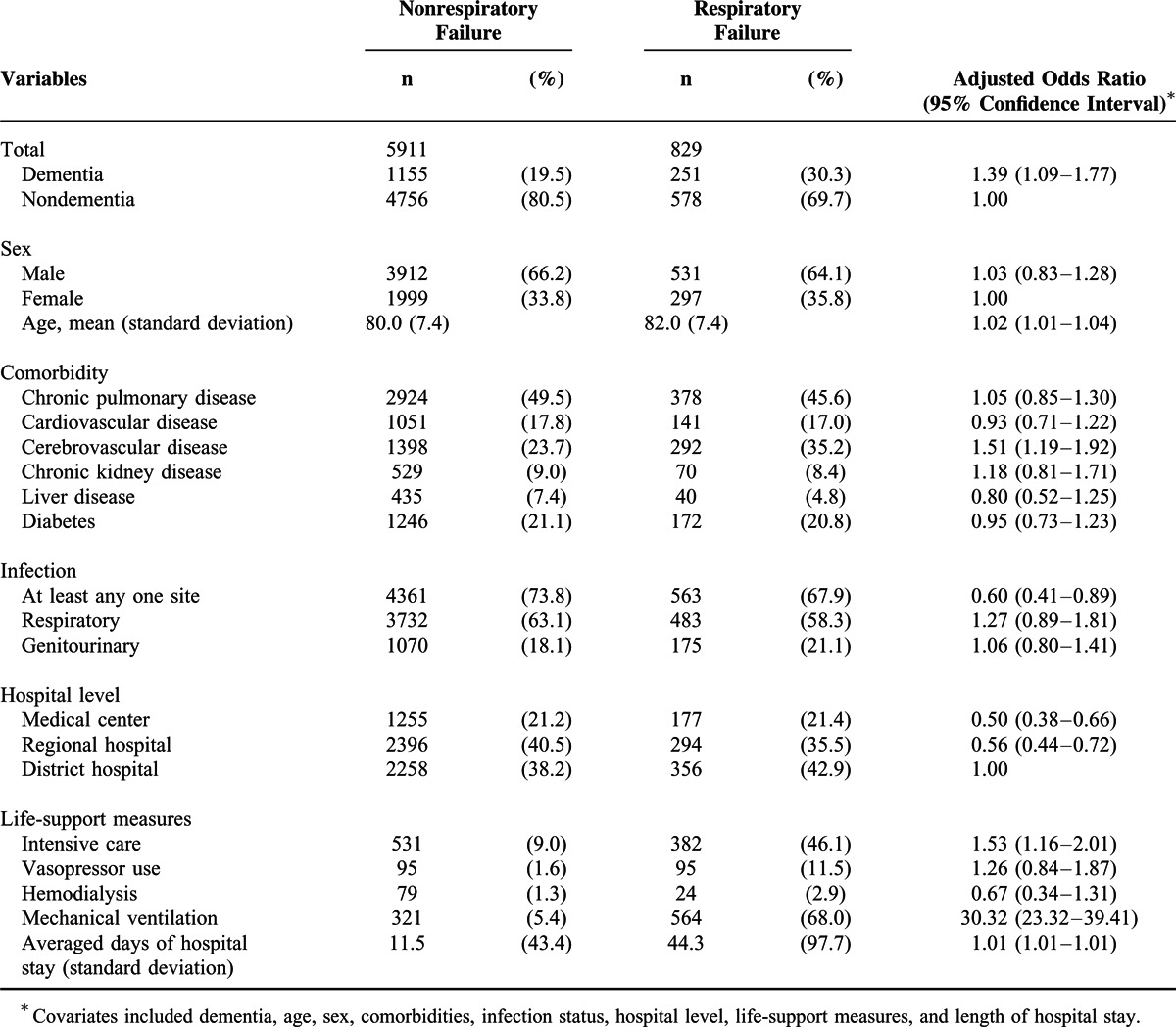
Table 5.
Factors Associated With Hospital Mortality in Patients With COPD
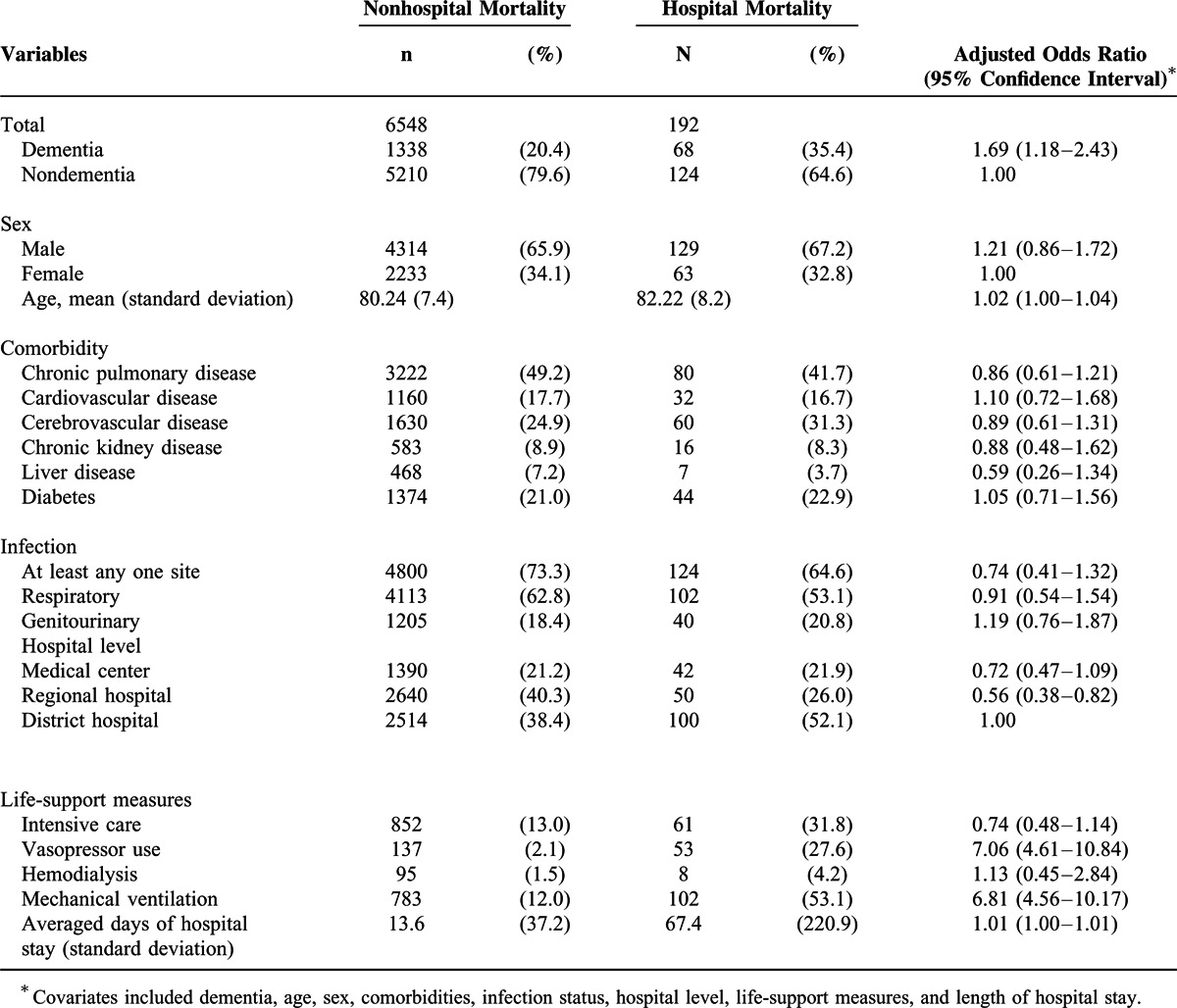
Table 4.
Factors Associated With Severe Sepsis in Patients With COPD
DISCUSSION
Main Findings
This is the first study using a nationwide, population-based, cohort study design to explore the outcomes of dementia in patients with COPD after hospitalization. In this study, we found that the presence of dementia in patients with COPD increased the risk of developing acute respiratory dysfunction, severe sepsis, increased the use of life-sustaining resources, and higher risk of mortality. These findings warrant the attention of health care professionals who care for patients with COPD and dementia.
Characteristics of Patients with COPD and Dementia
Some comorbidities noted in dementia population will increase mortality. For example, pneumonia had a frequency of 9.8% to 17.7% in patients with Alzheimer diseases in comparison to the control group, and pneumonia can predict the hospital mortality in the dementia group.14 According to the previous study, diabetes was the risk factor associated with mortality in institutionalized older patients with dementia (OR = 2.32; 95% CI 1.35–4.00). In our study, patients with COPD and dementia had higher prevalence of comorbid conditions and dementia associated with mortality in patients with COPD with OR = 1.69. Both diabetes and dementia are patient-related risk factors that predict poor outcome.15
In our patients with COPD and dementia, the prevalence of diabetes was extremely high (74.8%) compared to nondementia COPD patients. Although the prevalence of dementia was high in patients with diabetes, the causal relationship between diabetes and dementia is still not fully understood. Previous studies16 have shown that diabetes was associated with changes in cognition, such as slowing of mental speed, learning and memory, or diminished mental flexibility and mental speed. Large, longitudinal, population-based studies, and a systematic review 17 also demonstrated that diabetes was associated with an increased incidence of dementia and that diabetes was prevalent (up to 80%) in patients with Alzheimer disease. A recent study18 suggested that the brain cells had a decreased sensitivity to insulin, which could be an early and common feature of Alzheimer disease. The findings from these studies may account for the high prevalence of diabetes in patients with COPD and dementia.
Previous studies have shown that pneumonia and urinary tract infections were the leading causes of acute care hospitalization in patients with dementia.19 In our study, we found that there was no significant difference in the risk of overall infection between COPD patients with or without dementia. However, genitourinary infections were more common among patients with COPD and dementia than nondementia patients. The respiratory system accounts for a large portion of infections among the COPD population and plays an important role in acute exacerbation. In our cohort, patients with COPD had a high respiratory infection rate regardless of their dementia status.
In Taiwan, more than 50% of patients with COPD and dementia were hospitalized in district hospitals, and they also used more life support measures. Physicians from district hospitals should be aware that patients with COPD and dementia have more comorbidities, severe disease conditions, and higher mortalities, and these patients need more attention. The referral system between hospitals of different accreditation levels should be exercised to transfer patients with deteriorating conditions to medical centers whenever necessary.
The Effect of Dementia on Outcomes in Hospitalized Patients With COPD
From the previous report,20 because of the feeding difficulties, catabolic problem, and other mechanism that are not totally understood, patients with dementia may lead to body weight loss and lower body mass index. These chronic conditions increased mortality rates for patients with dementia. Otherwise, in a longitudinal study of about 250 patients with mild-to-moderate Alzheimer disease, authors showed that the independent risk factor for death caused by dementia was the pathologic process of cerebral inflammation. Aspiration, self-neglect, and sedentary lifestyle are very common consequences of dementia and related causes of death.21 In the study, we found risk factors that associated with dementia were cardiovascular disease, cerebrovascular disease, and diabetes. Our study also demonstrated that the risk of acute organ dysfunction in the respiratory system was significantly greater in patients with COPD and dementia than in nondementia patients. This finding has important implications for the care of patients with COPD and dementia. Because patients with dementia are at risk of developing delirium,22 aspiration, and dysfunctions in other organs, airway protection is important in these patients. Except for respiratory dysfunction, our study found no significant differences in the acute dysfunction of other systems between patients with or without dementia.
A previous study suggested a minor role of dementia on mortality in hospitalized older patients after accounting for life support.10 Other previous studies have also reported a minimal effect of dementia in admitted patients suffering from life-threatening situations.23,24 These studies reported the effect of dementia in life-threatening diseases, but our study highlighted the important role of dementia in association with the risk of death in a wide range of hospitalized patients with COPD. Because our study population focus on patients with a wide range of COPD severity, the effect of dementia on mortality was increased in this population. Given the increasing number of patients impaired by dementia and COPD over the years, the importance of managing dementia in patients with COPD should not be overlooked.
Aspiration in Patients With COPD and Dementia
The prevalence of gastroesophageal reflux disease (GERD) and esophageal disorders in patients with COPD is also higher than the general population. GERD is also associated with COPD acute exacerbations.25 Previous study has also been documented to have a much higher rate of recurrent aspiration, microaspiration, and pneumonia in patients with COPD and GERD.26 The most common cause of death in patients with advanced dementia was aspiration pneumonia and eating problems and dysphagia is a negative prognostic factor for survival.27 A retrospectively study for patients with COPD aged 40 and older, using the Diagnosis Procedure Combination database revealed higher mortality was associated with comorbid conditions, including aspiration pneumonia.28 Aspiration pneumonia is the important factor in COPD exacerbation and mortality, especially in the group of people with dementia. It is important to raise the awareness to protect airways against aspiration in patients with COPD and dementia.
Strengths and Limitations
This study has several strengths. First, this study had a large sample size and adequate statistical power to detect differences in the risks of prognosis related to dementia. Second, studies based on longitudinal claims such as ours have little room for loss to follow-up, which minimized the potential for selection bias. Third, we adjusted for a number of comorbidities and life-supporting measures that illustrated the independent effect of dementia on the outcomes of hospitalization in patients with COPD. Despite the above strengths, some limitations in our study should be addressed. First, the major limitation was that some of the known prognostic factors of COPD, including a history of cigarette smoking, pulmonary function, degree of tachypnea, and severity of dementia were not available from the claims database. The inability to adjust for these prognostic factors might have confounded our results. Second, the reliance on the disease coding in the medical claims might be subject to disease misclassification bias. Moreover, there are only 5 diagnostic codes for each hospital discharge record in the Taiwan NHI inpatient claim data diagnosis. Thus, some outcome measures could have been missed resulting in an underestimation of the incidence of adverse outcome measures. In other countries, like Australia, have 55 diagnostic code spaces per patient episode, which may increase capture rate of diagnoses. Nonetheless, the ICD-9 CM codes used for COPD diagnosis have been extensively used in other studies,29 and the internal findings also support the coding validity.30 Moreover, potential disease misclassification bias, if any, tends to be nondifferential and favors the estimates toward the null hypothesis.10
CONCLUSION
In conclusion, the presence of dementia increases the risk of respiratory organ dysfunction, severe sepsis, and hospital mortality in hospitalized patients with COPD. The outcomes of patients with COPD and dementia can be improved by healthcare professionals’ awareness of this high-risk subpopulation among patients with COPD.
Acknowledgments
This study is based in part on data from the NHIRD provided by the Bureau of the NHI, Department of Health and managed by National Health Research Institutes. The authors acknowledge the assistance of the Bureau of the NHI and National Health Research Institutes.
Footnotes
Abbreviations: CI = confidence interval, COPD = chronic obstructive pulmonary disease, GERD = gastroesophageal reflux disease, NHI = National Health Insurance, OR = odds ratio.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Pauwels RA, Buist AS, Calverley PM, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop Summary. Am J Respir Crit Care Med 2001; 163:1256–1276. [DOI] [PubMed] [Google Scholar]
- 2.Tan WC, Seale P, Ip M, et al. Trends in COPD mortality and hospitalizations in countries and regions of Asia-Pacific. Respirology 2009; 14:90–97. [DOI] [PubMed] [Google Scholar]
- 3.Dodd JW, Getov SV, Jones PW. Cognitive function in COPD. Eur Respir J 2010; 35:913–922. [DOI] [PubMed] [Google Scholar]
- 4.Grant I, Heaton RK, McSweeny AJ, et al. Neuropsychologic findings in hypoxemic chronic obstructive pulmonary disease. Arch Intern Med 1982; 142:1470–1476. [PubMed] [Google Scholar]
- 5.Singh B1, Parsaik AK, Mielke MM, et al. Chronic obstructive pulmonary disease and association with mild cognitive impairment: The Mayo Clinic Study of Aging Mayo Clinic Proceedings. Mayo Clin Proc 2013; 88:1222–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sampson EL, Blanchard MR, Jones L, et al. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009; 195:61–66. [DOI] [PubMed] [Google Scholar]
- 7.Morrison RS, Siu AL. Survival in end-stage dementia following acute illness. JAMA 2000; 284:47–52. [DOI] [PubMed] [Google Scholar]
- 8.Meier DE, Ahronheim JC, Morris J, et al. High short-term mortality in hospitalized patients with advanced dementia: lack of benefit of tube feeding. Arch Intern Med 2001; 161:594–599. [DOI] [PubMed] [Google Scholar]
- 9.Campbell ML, Guzman JA. A proactive approach to improve end-of-life care in a medical intensive care unit for patients with terminal dementia. Crit Care Med 2004; 32:1839–1843. [DOI] [PubMed] [Google Scholar]
- 10.Shen H-N, Lu C-L, Li C-Y. Dementia increases the risks of acute organ dysfunction, severe sepsis and mortality in hospitalized older patients: A National Population-Based Study. PLoS One 2012; 7:e42751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Insurance Research Database. Available: http://nhird.nhri.org.tw/date_01.html (Accessed August 1, 2014). [Google Scholar]
- 12.Chien IC, Lin YC, Chou YJ, et al. Treated prevalence and incidence of dementia among National Health Insurance enrollees in Taiwan, 1996–2003. J Geriatr Psychiatry Neurol 2008; 21:142–148. [DOI] [PubMed] [Google Scholar]
- 13.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29:1303–1310. [DOI] [PubMed] [Google Scholar]
- 14.Heun R, Schoepf D, Potluri R, et al. Alzheimer's disease and co-morbidity: increased prevalence and possible risk factors of excess mortality in a naturalistic 7-year follow-up. Eur Psychiatry 2013; 28:40–48. [DOI] [PubMed] [Google Scholar]
- 15.Navarro-Gil P, González-Vélez AE, Ayala A, et al. Which factors are associated with mortality in institutionalized older adults with dementia? Arch Gerontol Geriatr 2014; 59:522–527. [DOI] [PubMed] [Google Scholar]
- 16.Brands AM, Biessels GJ, de Haan EH, et al. The effects of type 1 diabetes on cognitive performance: a meta-analysis. Diabetes Care 2005; 28:726–735. [DOI] [PubMed] [Google Scholar]
- 17.Biessels GJ, Staekenborg S, Brunner E, et al. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol 2006; 5:64–74. [DOI] [PubMed] [Google Scholar]
- 18.Talbot K, Wang HY, Kazi H, et al. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest 2012; 122:1316–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sampson EL, Blanchard MR, Jones L, et al. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009; 195:61–66. [DOI] [PubMed] [Google Scholar]
- 20.Luchsinger JA, Patel B, Tang MX, et al. Body mass index, dementia, and mortality in the elderly. J Nutr Health Aging 2008; 12:127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nägga K, Wattmo C, Zhang Y, et al. Cerebral inflammation is an underlying mechanism of early death in Alzheimer's disease: a 13-year cause-specific multivariate mortality study. Alzheimers Res Ther 2014; 6:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inouye SK. Delirium in older persons. N Engl J Med 2006; 354:1157–1165. [DOI] [PubMed] [Google Scholar]
- 23.Kimata T, Hirakawa Y, Uemura K, et al. Absence of outcome difference in elderly patients with and without dementia after acute myocardial infarction. Int Heart J 2008; 49:533–543. [DOI] [PubMed] [Google Scholar]
- 24.Pisani MA, Redlich CA, McNicoll L, et al. Short term outcomes in older intensive care unit patients with dementia. Crit Care Med 2005; 33:1371–1376. [DOI] [PubMed] [Google Scholar]
- 25.Hurst JR, Vestbo J, Anzueto A, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators: susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363:1128–1138. [DOI] [PubMed] [Google Scholar]
- 26.Martinez CH1, Okajima Y, Murray S, et al. Impact of self-reported gastroesophageal reflux disease in subjects from COPD Gene cohort. Respir Res 2014; 15:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med 2009; 361:1529–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasegawa W, Yamauchi Y1, Yasunaga H, et al. Factors affecting mortality following emergency admission for chronic obstructive pulmonary disease. BMC Pulm Med 2014; 14:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang MT, Tsai CL, Lo YW, et al. Risk of stroke associated with inhaled ipratropium bromide in chronic obstructive pulmonary disease: a population-based nested case-control study. Int J Cardiol 2012; 158:279–284. [DOI] [PubMed] [Google Scholar]
- 30.Wang MT, Lo YW, Tsai CL, et al. Statin Use and Risk of COPD Exacerbation Requiring Hospitalization. Am J Med 2013; 126:598–606. [DOI] [PubMed] [Google Scholar]


