Abstract
Purpose
To evaluate the accuracy of the Spot (V2.0.16) and Plusoptix S12 (ROC4, V6.1.4.0) photoscreeners in detecting astigmatism meeting AAPOS referral criteria in students from a population with high prevalence of astigmatism.
Methods
Students attending grades 3–8 on the Tohono O’odham reservation were examined. Screening was attempted with both the Spot and Plusoptix photoscreeners. Results were compared to cycloplegic refraction. Screening attempts providing no estimate of refractive error were considered fail/refer. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for detection of refractive errors were determined using AAPOS referral criteria and receiver operating characteristic area under the curve (ROC AUC) analysis was conducted for measures of astigmatism. Agreement between screening and cycloplegic refraction measurements of astigmatism, spherical equivalent, and anisometropia were assessed using t tests and correlation analyses.
Results
A total of 209 students were included. Of the total, 116 (55%) met examination-positive criteria based on cycloplegic refraction, with 105 of those (90%) meeting the criterion for astigmatism. Measurements success rates were 97% for Spot and 54% for Plusoptix. Comparing the Spot and the Plusoptix, sensitivity was 96% versus 100%, specificity was 87% versus 61%, PPV was 90% versus 76%, and NPV was 94% versus 100% for detection of refractive error. Both screeners overestimated astigmatism by 1/3 D to 2/3 D. AUC for astigmatism was 0.97 for Spot and 0.83 for Plusoptix.
Conclusions
In this highly astigmatic population, the Spot and the Plusoptix had similar sensitivity, but the Spot had better specificity and measurement success rates. Compared with results from study samples with lower rates of astigmatism, our results highlight the need to assess the ability of screening instruments to detect individual types of refractive errors.
Instrument-based vision screening of preschool children has been recommended by the American Academy of Pediatrics, the American Academy of Ophthalmology, the American Association for Pediatric Ophthalmology and Strabismus (AAPOS), and the American Association of Certified Orthoptists.1 Because they require minimal subject cooperation, vision screening instruments have the potential to be useful in detecting amblyopia risk factors in infants, toddlers, preschoolers, and nonverbal children. The results of studies evaluating two currently commercially available photoscreeners, the Spot (PediaVision Holdings LLC, Lake Mary FL; now available from Welch Allyn Inc, Skaneateles Falls, NY) and the Plusoptix S12 (Plusoptix Inc, Atlanta GA), in screening for amblyogenic risk factors have been generally positive.2–7 The present study assessed the utility of the Spot and Plusoptix instruments compared to cycloplegic refraction but differed from previous studies primarily in terms of its subject population: participants were members of a Native American tribe, the Tohono O’odham, who have a high prevalence of with-the-rule astigmatism.8,9 The primary purpose of this study is to evaluate the accuracy of the Spot and the Plusoptix S12 in detecting astigmatism meeting AAPOS referral criteria.10
Recent population-based studies have indicated that prevalence of astigmatism (≥1.50 D in the most astigmatic eye) in infants, toddlers, and young children (6–72 months of age) ranges from 6.3% (non-Hispanic white children) to 16.8% (Hispanic children), depending on ethnicity.12–15 Uncorrected astigmatism can negatively affect visual development: astigmatism-related amblyopia can develop by the preschool years (≥3 years of age),16–18 and bilateral decreased visual acuity has been shown to be independently associated with astigmatism (OR for ≥2.00 D = 17.6) in 30- to 72-month-olds.19
Subjects and Methods
Participants included students in grades 3–8 attending schools on the Tohono O’odham reservation who were enrolled in a study of astigmatism and amblyopia. All students in grades 3–8 were eligible to participate. This study was approved by the Tohono O’odham Nation and by the University of Arizona Institutional Review Board. Parents provided written informed consent, and children provided written assent before any testing was conducted.
Apparatus and Procedures
The Spot (Firmware 2.0.17, Software 2.0.16) and the Plusoptix S12 (ROC 4, V6.1.4.0) are infrared photoscreeners designed to screen children for amblyopia risk factors. They record images of both pupils simultaneously, and internal software generates information on noncycloplegic refractive error and ocular alignment. The examiner holds the device approximately 1 meter from the child in a dimly lit room. The devices produce lights and noise to attract the child’s attention and fixation. Both instruments provide the examiner with cues to assist in focusing and automatically record data once the image is properly focused.
Cycloplegic autorefraction was performed with the Retinomax K-Plus2 (Nikon Inc, Melville, NY) at least 30 minutes after instillation of 1 drop of proparacaine 0.5% followed by 1 drop of tropicamide 1% and 1 drop of cyclopentolate 1%. The autorefraction was adjusted as needed based on subjective refinement to determine a best estimate of refractive error. Typically, the final estimate of refractive error was the subjectively refined sphere and the cylinder and axis from autorefraction.
Photoscreening was attempted with the Spot and Plusoptix on all students according to the instructions provided in the instrument manuals. Photoscreenings were conducted in schools on the day of the examination prior to dilation or 2–4 weeks after the examination. Testing environment varied depending on space availability but was typically conducted in a room with reduced light levels to maximize pupil size for measurements. The subjects were positioned facing away from windows or other sources of bright light. If a screening (including an estimate of refractive error) was not successful on the first attempt, at least one additional attempt was made.
Data Analysis
Analyses were conducted using IBM SPSS version 21.0 (IBM Corp, Armonk, NY). In the present study, we used 2013 AAPOS screening criteria for children >48 months in order to classify screening results as pass or fail and to classify cycloplegic refraction results as examination positive or negative (astigmatism of >1.50 D, hyperopia of >3.50 D, myopia of <−1.50 D, anisometropia of >1.50 D).10 Screening attempts resulting in no estimate of refractive error were considered fail/refer. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for detection of refractive errors in general (astigmatism, spherical equivalent [SE], anisometropia) were determined. Receiver operating characteristic (ROC) of area under the curve (AUC) for right eye astigmatism was determined.
Paired t tests and correlation analysis were used to compare refractive error estimates (right eye astigmatism [clinical notation, J0, and J45] and SE, anisometropia) from each screening instrument with cycloplegic refractive error measurements. Astigmatism data was analyzed in vector notation (J0 and J45), because while clinical notation measurements allow for assessment of agreement with regard to astigmatism magnitude, vector notation permits assessment of agreement in astigmatism measurements while taking into account both magnitude and axis. J0 represents horizontal/vertical astigmatism, J45 represents oblique astigmatism.11
Results
Sample Description and Examination Results
A total of 209 students (117 females [56%]) underwent cycloplegic eye examination and attempted screening with both the SPOT and Plusoptix S12. The mean age (with standard deviation) at screening was 11.89 ± 1.89 years (range, 8.64–15.55 years). Of the total, 116 (55%) had refractive error that met AAPOS screening referral criteria (an examination-positive result).10 A summary of AAPOS criteria met is provided in Table 1. Most students with an examination-positive result met the criterion for significant astigmatism (105/116, 90%). Only 1 student was determined to have a constant strabismus (exotropia) on examination. The Spot correctly identified the student as having astigmatism and myopia but did not detect ocular misalignment. We were unable to obtain a screening result for this student using the Plusoptix.
Table 1.
Summary of criteria met for examination positive results (astigmatism >1.50 D, hyperopia >3.50 D, myopia < −1.50 D, anisometropia >1.50 D)
| Examination positive criteria met | n | Percent |
|---|---|---|
| Astigmatism | 78 | 67.24% |
| Astigmatism, myopia | 18 | 15.52% |
| Astigmatism, hyperopia | 4 | 3.45% |
| Astigmatism, myopia, anisometropia | 3 | 2.59% |
| Astigmatism, anisometropia | 2 | 1.72% |
| Myopia | 7 | 6.03% |
| Hyperopia | 2 | 1.72% |
| Hyperopia, anisometropia | 2 | 1.72% |
| Total | 116 | 100% |
Screening Success Rates
A screening result (including an estimate of refractive error) was obtained on 202 students with the Spot (97%) and on 112 students with the Plusoptix (54%). A summary of examination results for the students from whom we were unable to obtain a refractive error estimate with the Spot and Plusoptix is provided in Table 2. Students for whom a refractive error estimate was not obtained were classified as a screening fail.
Table 2.
Examination results for the students for whom we were unable to obtain an estimate of refractive error with the Spot and the Plusoptix
| Instrument | Exam Result | n | Percent |
|---|---|---|---|
| Spot | Exam Negative | 1 | 14.29% |
| Astigmatism | 3 | 42.86% | |
| Astigmatism, Myopia | 2 | 28.57% | |
| Astigmatism, Myopia, Anisometropia | 1 | 14.29% | |
| Total | 7 | 100% | |
| Plusoptix | Exam Negative | 15 | 15.46% |
| Astigmatism | 49 | 50.52% | |
| Astigmatism, Myopia | 18 | 18.56% | |
| Astigmatism, Hyperopia | 4 | 4.12% | |
| Astigmatism, Myopia, Anisometropia | 3 | 3.09% | |
| Astigmatism, Anisometropia | 2 | 2.06% | |
| Hyperopia | 2 | 2.06% | |
| Hyperopia, Anisometropia | 2 | 2.06% | |
| Myopia | 2 | 2.06% | |
| Total | 97 | 100% | |
Comparison of Cycloplegic Examination and Screening Refraction Results
A summary of screening results are provided in Tables 3 and 4. The Spot provided better specificity and PPV; the Plusoptix provided better sensitivity and NPV. ROC analysis for detection of astigmatism was performed on right eye data. Only right eye data are presented, because results were similar for the left eye. For students on whom a screening estimate of astigmatism could not be obtained, a value beyond upper range of astigmatism estimates for the sample (10.00) was assigned so that “missing” values for both instruments (which would be considered screening “fail” results) could be included. The AUC was 0.97 for the Spot and 0.83 for the Plusoptix (P < 0.001 for both).
Table 3.
Cross tabulation of Spot and Plusoptix results by examination results
| Exam Result Negative/Pass |
Positive/Fail | Total | ||
|---|---|---|---|---|
| Spot Result | Negative/Pass | 81 | 5 | 86 |
| Positive/Fail | 12 | 111 | 123 | |
| Total | 93 | 116 | 209 | |
| Exam Result Negative/Pass |
Positive/Fail | Total | ||
| Plusoptix Result | Negative/Pass | 57 | 0 | 57 |
| Positive/Fail | 36 | 116 | 152 | |
| Total | 93 | 116 | 209 | |
Table 4.
Summary of Spot and Plusoptix performance with cycloplegic refraction as gold standard. Success rates are for obtaining estimate of refractive error. Unable to screen considered screening “fail”.
| Screener | Success Rate | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| Spot V2.0.16 | 97% | 96% | 87% | 90% | 94% |
| Plusoptix S12 | 54% | 100% | 61% | 76% | 100% |
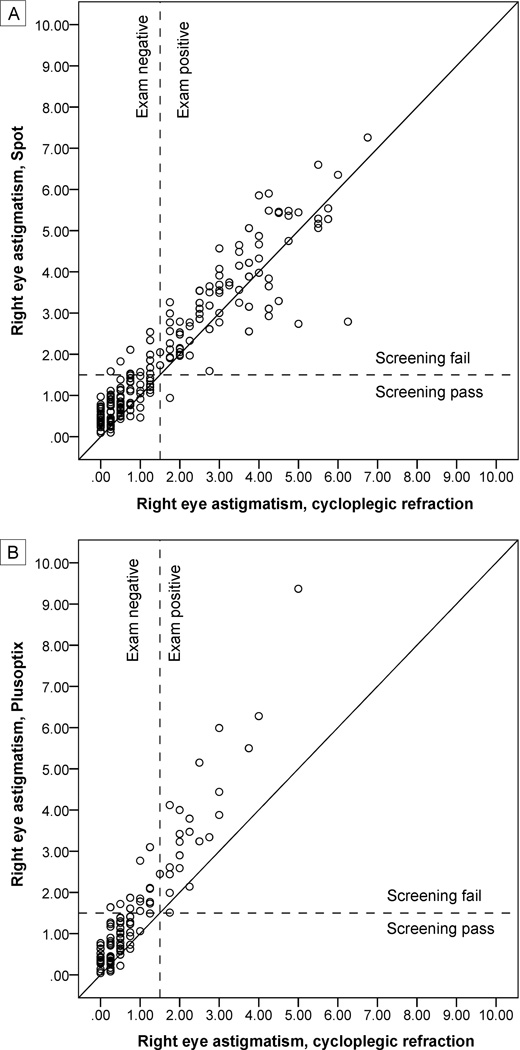
Paired t tests and correlation analyses were used to compare Spot and Plusoptix S12 estimates of right eye astigmatism (clinical notation, J0, J45), right eye SE, and anisometropia (absolute value of the difference between right eye and left eye spherical equivalent) to cycloplegic refraction measurements for students on whom we were able to obtain screening estimates of refractive error (Table 5). All mean screening estimates significantly differed from mean cycloplegic refraction measurements with the exception of anisometropia estimates obtained with the Spot (P = 0.053) and measurements of J45 obtained with the Spot and the Plusoptix (P = 0.10). All screening instrument estimates of refractive error were significantly correlated with cycloplegic measurements. For both instruments, correlations were very strong (>0.90) for clinical notation and J0 astigmatism and strong (>0.50) for J45 astigmatism and SE. For anisometropia, the correlation for the Spot was strong, but the correlation for the Plusoptix was weak (0.21). Scatterplots comparing screening estimates of astigmatism (clinical notation) to cycloplegic measurements of astigmatism are shown in Figure 1.
Table 5.
Comparison of Right Eye (RE) Spot and Plusoptix refractive error estimates to cycloplegic refraction measurements of astigmatism, spherical equivalent, and anisometropia for students on whom a screening estimate was obtained. T-tests and correlation analyses compared results for screening instruments to results for cycloplegic refraction.
| Screener | Measurement | Mean | SD |
t
test P value |
Correlation (r) |
Correlation P value |
|
|---|---|---|---|---|---|---|---|
| Spot N=202 |
Astigmatism J0 | Cyclo Ref | 0.79 | 0.82 | <0.001 | 0.92 | <0.001 |
| Spot | 0.90 | 0.80 | |||||
| Difference | −0.12 | 0.33 | |||||
| Astigmatism J45 | Cyclo Ref | 0.07 | 0.28 | =0.097 | 0.61 | <0.001 | |
| Spot | 0.11 | 0.45 | |||||
| Difference | −0.04 | 0.35 | |||||
| Astigmatism Clinical notation | Cyclo Ref | 1.64 | 1.67 | <0.001 | 0.93 | <0.001 | |
| Spot | 1.98 | 1.65 | |||||
| Difference | −0.34 | 0.60 | |||||
| Spherical Equivalent | Cyclo Ref | +0.20 | 1.51 | <0.001 | 0.85 | <0.001 | |
| Spot | −0.10 | 1.01 | |||||
| Difference | 0.30 | 0.84 | |||||
| Anisometropia | Cyclo Ref | 0.40 | 0.66 | =0.053 | 0.83 | <0.001 | |
| Spot | 0.35 | 0.59 | |||||
| Difference | 0.05 | 0.36 | |||||
| Plusoptix N=112 |
Astigmatism J0 | Cyclo Ref | 0.40 | 0.47 | <0.001 | 0.94 | <0.001 |
| Plusoptix | 0.67 | 0.77 | |||||
| Difference | −0.27 | 0.36 | |||||
| Astigmatism J45 | Cyclo Ref | 0.02 | 0.17 | =0.101 | 0.79 | <0.001 | |
| Plusoptix | 0.05 | 0.30 | |||||
| Difference | −0.03 | 0.20 | |||||
| Astigmatism Clinical notation | Cyclo Ref | 0.84 | 0.97 | <0.001 | 0.94 | <0.001 | |
| Plusoptix | 1.48 | 1.52 | |||||
| Difference | −0.64 | 0.69 | |||||
| Spherical Equivalent | Cyclo Ref | +0.09 | 0.87 | <0.001 | 0.69 | <0.001 | |
| Plusoptix | +0.56 | 1.07 | |||||
| Difference | −0.48 | 0.78 | |||||
| Anisometropia | Cyclo Ref | 0.25 | 0.20 | <0.001 | 0.21 | =0.027 | |
| Plusoptix | 0.43 | 0.41 | |||||
| Difference | −0.17 | 0.41 | |||||
Cyclo Ref = cycloplegic refraction
Figure 1.
Scatterplots of Spot (A) and Plusoptix (B) estimates of astigmatism compared to cycloplegic refraction measurements of astigmatism for right eyes. Solid lines represents line of unity (perfect agreement). Dashed lines represent AAPOS referral criterion for astigmatism (1.50 D). Points in upper right and lower left quadrants represent accurate screening results.
Discussion
In a previous study,20 our group compared four methods for screening Tohono O’odham preschool children for significant astigmatism: Lea symbols visual acuity (Precision Vision, LaSalle IL, now available from Good-Lite Co, Elgin IL), MTI photoscreening (Medical Technologies Inc, Lancaster PA, no longer manufactured), Nidek KM-500 keratometry (Marco Ophthalmic Inc, Jacksonville FL, no longer manufactured), and Nikon Retinomax K-plus noncycloplegic autorefraction (Nikon Inc, Melville, NY; newer versions now manufactured by Right Manufacturing Co, Tokyo, Japan). ROC analyses indicated that autorefraction (AUC, 0.98) and keratometry (AUC, 0.92) provided better results than photoscreening (AUC, 0.78) or visual acuity screening (AUC, 0.70). Measurement success rates for autorefraction and keratometry screening were also very high (>99% for keratometry and autorefraction compared to 93% for photoscreening and 92% for visual acuity screening). As a result, keratometry screening was recommended to the Tribe for screening preschoolers for astigmatism due to the similar performance and lower cost of the keratometer compared to the autorefractor. In the present study, AUC results for detection of astigmatism was high for both instruments, with the Spot (AUC, 0.97) performing similarly to the autorefractor and keratometer and better than the Plusoptix S12 (AUC, 0.83). However, the present study included older subjects than the previous study, and it is possible that the results presented here may overestimate performance for younger children.
Classifying students for whom we were unable to obtain refractive error measurements as screening failures yields similar sensitivity for the two instruments but lower specificity for the Plusoptix compared to the Spot. As shown in Table 2, significant refractive error was present in 85% of subjects on whom we were not able to obtain an estimate of refractive error with the Plusoptix. This result is similar to what we found with the SureSight (Welch Allyn, no longer manufactured) in this population. The SureSight often provided an “out of measurement range” result rather than an estimate of astigmatism magnitude for children with high astigmatism; the out-of-range result was often a reliable indicator of the presence of high astigmatism and the need for referral. However, there were a larger number of examination-negative students for whom we were unable to obtain a screening estimate of refractive error with the Plusoptix (15) compared to the Spot (1); thus failure to obtain a screening estimate of refractive error was not always associated with the presence of high refractive error. Also, confidence in the result on the part of the individual conducting the screening and the parent may be reduced in instances in which the instrument-based screener does not provide an estimate of refractive error or reason for referral and may reduce the likelihood that parents will follow-up appropriately. Future research on compliance with vision screening follow-up should assess this as a possible factor (referrals based on “screening failure” vs “unable to screen” or “out of range”) that may contribute to follow-up compliance.
Several recent studies have examined performance of the Spot and Plusoptix in pediatric ophthalmology patients and classified unsuccessful screenings as fail/refer results.2–6 As in the present study, the Spot had a higher success rate in providing estimates of refractive error in two of three studies that directly compared the two instruments.2,3,5 However, the success rate for the Plusoptix in the present study was much lower than observed in pediatric ophthalmology clinic samples, suggesting that the low success rate we observed was due to the high rate of astigmatism in our study population. Another factor that may contribute to differences in success rates across studies is tester experience.
Direct comparison across studies on measures of sensitivity, specificity, PPV, and NPV should be made with caution, because different versions of the instruments, different screening referral criteria, and different examination-positive criteria are used.2–6 In addition, when using a composite examination-positive definition (eg, “astigmatism or hyperopia or myopia or anisometropia”), the same instrument version and same criteria may still yield different specificity and sensitivity for the composite outcome in populations with different relative prevalences of the different types of refractive error. Reports of sensitivity across studies has been good for both instruments (>80%), although specificity has varied most likely due to differences in study populations (age range, presence of ocular abnormalities, inclusion of children with developmental delay, etc). In a cohort of 444 1- to 16-year-olds screened with the Spot (as in the present study, using Spot software v2.0.16 and applying current AAPOS referral criteria for both screening and examination results10), Peterseim and colleagues6 found a sensitivity of 84.8, specificity of 70.9, PPV of 78.1, and NPV of 79.2, compared with 96%, 87%, 90%, and 94%, respectively, in the present study. The Spot’s poorer performance in their study may be due in part to the fact that it included younger children, many with significant ocular pathology.
In another study, Peterseim and colleagues5 prospectively screened and examined 265 1- to 16-year-old pediatric ophthalmology patients with the Spot (v1.0.3, software 1.1.51) and with the Plusoptix A09, both earlier versions of the instruments used in the present study, and compared refractive error estimates with cycloplegic refraction. The Spot provided refractive error estimates in 94% (compared to 97% in the present study) and the Plusoptix S09 provided refractive error estimates in 71% (compared to 54% in the present study). Both instruments overestimated myopia and underestimated hyperopia (Spot, 1.16 D; Plusoptix, 0.47 D more negative SE than cycloplegic retinoscopy). The Spot estimates of SE in the present study were on average 0.30 D more negative than cycloplegic refraction, and the Plusoptix estimates of SE were on average 0.48 D more positive than cycloplegic refraction. Peterseim and colleagues5 reported that both instruments overestimated astigmatism (Spot overestimated by 0.36 D (compared to 0.34 D in the present study) and the Plusoptix overestimated by 0.32 D (compared to 0.64 D in the present study). For measurements of astigmatism, the Spot provided results comparable to ours, but the Plusoptix performed better in the Peterseim and colleagues study.
When estimates of refractive error were obtained, both instruments provided astigmatism, SE, and anisometropia estimates that were significantly correlated with cycloplegic refraction measurements. Lower correlations for SE and anisometropia were obtained for Plusoptix compared to the Spot. This may be due in part to a reduced range of refractive errors in the Plusoptix sample, because students for whom we were able to acquire Plusoptix refractive error estimates were less astigmatic, less hyperopic, and less anisometropic on average compared to children for whom we were able to acquire Spot refractive error estimates (Table 5). Comparisons of agreement between screening estimates and cycloplegic refraction measurements (t tests and correlation analyses) across instruments must be offered with due caution, because the Plusoptix was unable to provide a refractive error estimate on a significant number of students who are not included in these analyses.
The present study has several limitations. First, the school-age subjects in the study were older than the preschool target age for photoscreening. Measurement success rates may be lower in younger children from this population. Second, the present study provides little information on the ability of the Spot or Plusoptix to detect strabismus: only 1 student was identified upon examination as having a constant strabismus. Third, the findings are limited in terms of generalizability to other populations due to the high prevalence of astigmatism and low prevalence of other refractive errors and strabismus in our sample. For example, pediatric ophthalmology patient samples are likely to have a high prevalence of strabismus, which was essentially absent in our sample, and hyperopia, which is more difficult to detect in the absence of cycloplegia than astigmatism. Comparisons with previous studies suggest that the present study is likely to have underestimated the utility of the Plusoptix for use in populations with lower rates of astigmatism. Fourth, these findings may not apply to all axes of astigmatism. Astigmatism in our sample was almost always with-the-rule, as evidence by the positive mean J0 values (positive J0 = with-the-rule astigmatism; negative J0 = against-the-rule astigmatism) and minimal levels of J45 (oblique) astigmatism (see Table 5).
The present study also has several strengths. First, the school-based sample provides a good indication of how the instruments will perform in a general screening of children from this population (compared to studies with pediatric ophthalmology patient-based samples). Our results reflect screening performance in a situation in which the environment (eg, room lighting) is not completely controlled, as it is in a clinic setting. The high rate of refractive errors and ocular abnormalities in pediatric ophthalmology patient samples allows for assessment of screening performance with relatively few subjects, but the generalizability of the findings to community, school, or primary care–based samples is limited. Second, the results provide valuable information on the ability of these two screeners to detect clinically significant astigmatism. For this population with such a high prevalence of astigmatism, our results suggest that the Spot is more effective.
In conclusion, our findings highlight the need for studies assessing detection of specific refractive errors. Ideally, screening performance should not vary with the population tested. However, in the case of screening for overall refractive error, an instrument may vary in its ability to detect different types of refractive errors, and if relative prevalence varies across populations (as we know it does), overall performance will vary with the population tested. The present study assesses the ability of the instruments to detect significant astigmatism. Future studies should also report screening performance for specific refractive errors as well as overall performance. Such studies will provide valuable information on the strengths and limitations of each instrument, will allow for appropriate selection of screening instruments for use in specific populations (eg, Hispanic preschoolers who also have an elevated prevalence of astigmatism),14 and may lead to further refinement of the instruments.
Acknowledgments
Financial support: National Institutes of Health National Eye Institute (NIH/NEI) grant U10-EY13153 (EMH) and Research to Prevent Blindness (RPB).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data presented in part at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Denver, Colorado, May 3–7, 2015.
References
- 1.Miller JM, Lessin HR American Academy of Pediatrics Section on Ophthalmology; Committee on Practice and Ambulatory Medicine; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Instrument-based pediatric vision screening policy statement. Pediatrics. 2012;130:983–986. doi: 10.1542/peds.2012-2548. [DOI] [PubMed] [Google Scholar]
- 2.Arnold RW, Armitage MD. Performance of four new photoscreeners on pediatric patients with high risk amblyopia. J Pediatr Ophthalmol Strabismus. 2014;51:46–52. doi: 10.3928/01913913-20131223-02. [DOI] [PubMed] [Google Scholar]
- 3.Kirk S, Armitage MD, Dunn S, Arnold RW. Calibration and validation of the 2WIN Photoscreener compared to the Plusoptix S12 and the Spot. J Pediatr Ophthalmol Strabismus. 2014;51:289–292. doi: 10.3928/01913913-20140701-01. [DOI] [PubMed] [Google Scholar]
- 4.Silbert DI, Matta NS. Performance of the Spot vision screener for the detection of amblyopia risk factors in children. J AAPOS. 2014;18:169–172. doi: 10.1016/j.jaapos.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Peterseim MMW, Papa CE, Wilson ME, et al. Photoscreeners in the pediatric eye office: Compared testability and refractions on high-risk children. Am J Ophthalmol. 2014;158:932–938. doi: 10.1016/j.ajo.2014.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peterseim MM, Papa CE, Wilson ME, et al. The effectiveness of the Spot Vision Screener in detecting amblyopia risk factors. J AAPOS. 2014;18:539–542. doi: 10.1016/j.jaapos.2014.07.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silbert DI, Matta NS, Ely AL. Comparison of SureSight autorefractor and plusotiX A09 photoscreeer for vision screening in rural Honduras. J AAPOS. 2014;18:42–44. doi: 10.1016/j.jaapos.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Harvey EM, Dobson V, Miller JM. Prevalence of high astigmatism, eyeglass wear, and poor visual acuity among Native American grade school children. Optom Vis Sci. 2006;83:206–212. doi: 10.1097/01.opx.0000214333.84822.71. [DOI] [PubMed] [Google Scholar]
- 9.Harvey EM, Dobson V, Clifford-Donaldson CE, Green TK, Messer DH, Miller JM. Prevalence of astigmatism in Native American infants and children. Optom Vis Sci. 2010;87:400–405. doi: 10.1097/OPX.0b013e3181d95b23. [DOI] [PubMed] [Google Scholar]
- 10.Donahue SP, Arthur B, Neeley DE, Arnold RW, Silbert D, Ruben JB AAPOS Vision Screening Committee. Guidelines for automated preschool vision screening: a 10-year, evidence based update. J AAPOS. 2013;17:4–8. doi: 10.1016/j.jaapos.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Miller JM. Clinical applications of power vectors. Optom Vis Sci. 2009;86:599–602. doi: 10.1097/OPX.0b013e3181a6a211. [DOI] [PubMed] [Google Scholar]
- 12.Giordano L, Friedman DS, Repka MX, et al. Prevalence of refractive error among preschool children in an urban population: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:739–746. doi: 10.1016/j.ophtha.2008.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dirani M, Chan YH, Gazzard G, et al. Prevalence of refractive error in Singaporean Chinese children: the strabismus, amblyopia, and refractive error in young Singaporean Children (STARS) study. Invest Ophthalmol Vis Sci. 2010;51:1348–1355. doi: 10.1167/iovs.09-3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fozailoff A, Tarczy-Hornoch K, Cotter S, et al. Writing Committee for the MEPEDS Study Group. Prevalence of astigmatism in 6- to 72-month-old African American and Hispanic children: the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2011;118:284–293. doi: 10.1016/j.ophtha.2010.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wen G, Tarczy-Hornoch K, McKean-Cowdin R, et al. Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120:2109–2116. doi: 10.1016/j.ophtha.2013.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atkinson J, Braddick O, Robier B, et al. Two infant vision screening programmes: prediction and prevention of strabismus and amblyopia from photo- and videorefractive screening. Eye (Lond) 1996;10(Pt 2):189–198. doi: 10.1038/eye.1996.46. [DOI] [PubMed] [Google Scholar]
- 17.Dobson V, Miller JM, Harvey EM, Mohan KM. Amblyopia in astigmatic preschool children. Vision Res. 2003;43:1081–1090. doi: 10.1016/s0042-6989(03)00014-2. [DOI] [PubMed] [Google Scholar]
- 18.Mohindra I, Jacobson SG, Held R. Binocular visual form deprivation in human infants. Doc Ophthalmol. 1983;55:237–249. doi: 10.1007/BF00140811. [DOI] [PubMed] [Google Scholar]
- 19.Tarczy-Hornoch K, Varma R, Cotter SA, et al. Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups. Risk factors for decreased visual acuity in preschool children: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011;118:2262–2273. doi: 10.1016/j.ophtha.2011.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller JM, Dobson V, Harvey EM, Sherrill DL. Comparison of preschool vision screening methods in a population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci. 2001;42:917–924. [PubMed] [Google Scholar]