Abstract
Diseases such as gastroesophageal reflux disease (GERD), bulimia, anorexia, and extrinsic alimentary factors may cause dental erosion (DE). The minimally invasive therapeutic attitude preserves the remaining healthy tooth structure. In the earlier stages, the direct restoration of dental lesions is possible, using composite materials. In advanced stages of DE, prosthetic treatments are recommended for stable esthetic and functional results. We present a case of DE in a partially edentulous patient who benefited from a complex therapy. The prosthetic project of the case involves ceramic veneers associated with dental and implant supported fixed prosthesis for the restoration of esthetics, mastication, phonetics and their maintenance.
Keywords: dental erosion, ceramic veneers, fixed partial dentures, gastroesophageal reflux disease
Background and aim
Dental erosion (DE) has become more frequent during the last decades, especially in children and young people [1]. Increased consumption of carbonated drinks but also endogenous factors are involved in DE etiology [2]. Associated esthetic, phonetic and masticatory dysfunctions are related to advanced generalized erosions which affect the entire dental arches.
The important objective in the dental erosion therapy is the minimally invasive crown reconstruction. Direct restoration using composite materials is possible in the earlier stages [1]. Full arch reconstructions are necessary in advanced generalized DE and an esthetic project must be developed.
In this case report we present a treatment plan option in a patient presenting DE and lateral partial edentulous spaces.
When the patient presents tooth loss and severe DE, treatments involving fixed partial dentures (FPD) and all ceramic reconstructions are recommended to obtain improved esthetics and good functionality. In terms of treatment cost, advanced stages of DE become expensive when using all ceramic reconstructions.
Therefore, sustained prophylaxis has to be done to avoid DE evolution: diet control has to be effective in patients with evidenced extrinsic factors. In endogenous DE caused by bulimia, anorexia, gastro-esophageal reflux disease (GERD), or other gastric diseases involving vomiting, associated etiologic therapy is necessary [1].
Case presentation
A 47-year-old female complains of masticatory and esthetic discomfort after a mandibular bridge fracture. She also demands esthetic restorations on maxillary frontal teeth, which became progressively darker and irregular.
Medical history shows GERD diagnosis and antacid medication three years ago. Symptoms of GERD were related to a psychological trauma and were subsided at the time of study.
After the clinical examination of the maxillary arch, we found DE and composite cervical restorations on the central incisors; used composite veneers were present on the lateral incisors. DE could not be evaluated on other maxillary teeth because they were all recovered by metal-ceramic FPD: an FPD on 13, 15 and 17 restoring the missing 14,16 and an extended FPD on 23 and 27 with intermediary for 24, 25, 26 (Fig. 1).
Figure 1.
Initial clinical situation. Metal-ceramic bridges and dental erosions on the front teeth.
A fractured mandibular FPD for the missing 35, 36, was causing masticatory and esthetic disorders; the mesial abutment tooth, 34, was extracted one year ago. A metal-ceramic FPD was found on 44, 45, 47 restoring the 46 missing tooth (Fig 1).
Siebert class one atrophy is present on edentulous crests.
All present fixed prostheses have deficient marginal fit and/or incorrect design. Overload abutment teeth 23, 27 show gingival recession, and X-ray examination shows important bone loss on 27. The patient has a good oral hygiene.
Maxillary central incisors margins and buccal faces are affected by DE, resulting in important tooth wear with shape and color modifications (Fig. 1). Wear composite veneers on the lateral maxillary incisors are also non-aesthetic. Mandibular teeth present dental erosion on incisor margins. Application of DE Questionnaire reveals few alimentary factors involved: citric fruits preference and daily carbonated drinks consumption.
Case analysis and therapeutic decision
After clinical examination, radiologic and basic erosion wear examination (BEWE), the esthetic analysis was performed. All existing FPDs had to be removed and a full maxillary arch reconstruction was decided, using dental and implant supported fixed prosthesis. Eroded maxillary incisors will be restored by ceramic veneers improving esthetics and allowing good biological integration [3]. Bonded cementation of ceramics result in strong restorations when precise fit of the veneers avoid excessive space for the cement [4]. This patient has no parafunction and a favorable prognosis of ceramic restorations is predictable.
A metal-ceramic FPD on 13, 15 and 17 will successfully restore the missing 14 and 16 using modified saddle intermediaries (Fig. 2).
Figure 2.
FPD metal infrastructure on the master cast.
The prognosis of 27 as abutment tooth is uncertain because of reduced bone support. Two implants are required for an implant supported FPD restoring 24, 25, 26 edentulous space. Two metal ceramic crowns will restore 23 and 27, already prepared (Fig. 3). For esthetic reasons, a metal ceramic crown with cervical ceramic collar will restore 13 and 23.
Figure 3.
FPDs metal design on the maxillary master cast.
Good health and favorable bone condition allow us to do a metal-ceramic implant supported FPD in the three-unit edentulous space of 34, 35, 36. Maximum masticatory forces occur on the first mandibular molar. This treatment plan is favorable to bone maintenance, FPD resistance and avoid 33 preparation (Fig. 4). For the missing 46, a metal - ceramic FPD with abutment teeth 44, 45, 47 was decided. Existing endodontic treatments on 44, 45 were accurate from a radiological point of view.
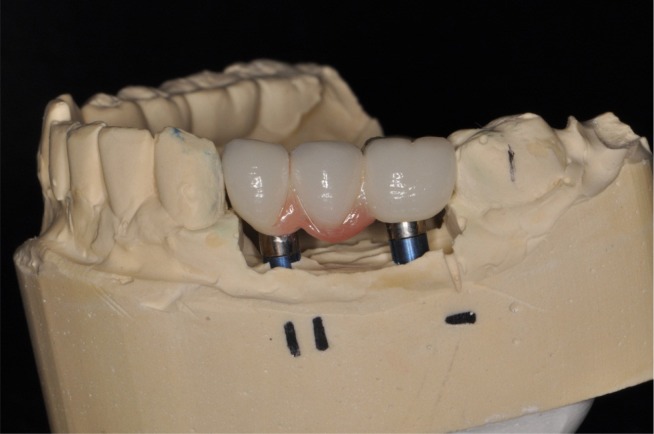
Figure 4.
Gingival appearance on implant supported metal-ceramic FPD.
Clinical procedures
After therapeutic decision was made, we removed the FPDs and implants were inserted. After insertion, the implants were allowed to integrate. Six months later, a new radiologic control was performed, implants were uncovered and healing caps were placed. After two weeks, a first impression in irreversible hydrocolloid was taken and open custom tray was fabricated. Impression copings were adapted to implants and splinted with resin for accurate transfer of implants position to the master cast. One-step technique impressions were taken using medium and light body polyether.
Implant abutments were made in the laboratory and adapted on implants. Teeth preparations were finalized and one-step technique, maxillary and mandibular impressions were made.
The metal FPD infrastructures were made in the laboratory (Fig. 2, 3) and checked for correct fit on the abutment teeth in the oral cavity.
The symmetry of the final metal-ceramic reconstructions adequately solves the esthetic aspects regarding color, shape, position and dimension of the new prosthetic constructions. Rose porcelain was used to make an esthetic gingival appearance on implant supported FPDs (Fig. 4). Functional occlusion was verified to ensure correct antagonist contacts and guidance.
The patient demanded whiter teeth; consequently we replaced the existing fillings and made a bleaching two weeks before making the veneers.
Esthetic criteria was verified on ceramics; teeth visibility and correct position of incisors margins were phonetically and esthetically evaluated in front and lateral view (Fig. 5, 6). After finalization FPDs and veneers cementation was performed using resin cement. Functional anterior guidance was verified after veneers cementation.
Figure 5.
Harmonic relationship of ceramic veneers with inferior lip.
Figure 6.
Esthetic results of full maxillary arch reconstruction.
Finally, the patient quickly integrated her new prosthesis and enjoyed her younger smile.
Discussion
Avoiding teeth overloading is a major objective in the FPD treatment plan. Therefore, an implant-supported FPD is preferred to restore extended partial edentulous spaces when local and general conditions are favorable; crest maintenance is better when functional stimulus is transmitted to the bone by implants.
In the presented case the advanced tooth wear on central maxillary incisors was due to dominant erosive mechanism caused by GERD and associated with abrasion and attrition. Good prognosis of the prosthetic treatment depends on diet education and good general condition; GERD remission is favorable for post-therapeutic maintenance. Ceramic veneers option is less invasive than full ceramic crowns and provides improved esthetics [5,6].
The regular six-month control was performed after treatment, to achieve good maintenance.
Conclusions
Full arch esthetic restoration can change the patient’s life by improving functional comfort and self confidence. Laborious steps are involved and long time temporizations have to be accepted by the patient before starting with the treatment plan decision.
Ceramic veneers can successfully restore endogenous DE when etiology targeted therapy is effective.
Acknowledgments
This paper was written with the support of the grant AUF BECO 2012 – U 56135FT203.
References
- 1.Lussi A, Megert B, Shellis RP, Wang X. Analysis of the erosive defect of different dietary substances and medications. Br J Nutr. 2012;107(2):252–262. doi: 10.1017/S0007114511002820. [DOI] [PubMed] [Google Scholar]
- 2.Wongkhantee S, Patanapiradej V, Maneenut C, Tantbirojn D. Effect of acidic food and drinks on surface hardness of enamel, dentine and tooth coloured filling materials. J Dent. 2006;34:214–220. doi: 10.1016/j.jdent.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Gracis S, Fradeani M, Celletti R, Bracchetti G. Biological integration of aesthetic restorations: factors influencing appearance and long term success. Periodontol 2000. 2001;27:29–44. doi: 10.1034/j.1600-0757.2001.027001029.x. [DOI] [PubMed] [Google Scholar]
- 4.d’Incau E, Couture C, Maureille B. Human tooth wear in the past and the present: Tribological mechanisms, scoring systems, dental and skeletal compensations. Archives of oral biology. 2012;57:214–229. doi: 10.1016/j.archoralbio.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Fradeani M. Vol 2. Prosthetic Treatment: A Systematic Approach to Esthetic, Biologic, and Functional Integration. Paris: Quintessence; 2008. Esthetic rehabilitation in fixed prosthodontics; p. 410. [Google Scholar]
- 6.Chiche GJ, Pinault A. Artistic and scientific principles applied to esthetic dentistry Esthetics of anterior fixed prosthodontics. Chicago Quintessence. 1994:13–32. [Google Scholar]