Abstract
Purpose
There have been few longitudinal studies of deliberate self-harm (DSH) in adolescents. This cross-national longitudinal study outlines risk and protective factors for DSH incidence and persistence.
Methods
Seventh and ninth grade students (average ages 13 and 15 years) were recruited as state-representative cohorts, surveyed and then followed-up 12-months later (N = 3,876), using the same methods in Washington State and Victoria, Australia. The retention rate was 99% in both states at follow-up. A range of risk and protective factors for DSH were examined using multivariate analyses.
Results
The prevalence of DSH in the past year was 1.53% in grade 7 and .91% in grade 9 for males and 4.12% and 1.34% for grade 7 and 9 females, with similar rates across states. In multivariate analyses, incident DSH was lower in Washington State (OR .67, 95% CI .45, 1.00) relative to Victoria 12-months later. Risk factors for incident DSH included being female (OR 1.93, CI 1.35, 2.76), high depressive symptoms (OR 3.52, CI 2.37, 5.21), antisocial behavior (OR 2.42, CI 1.46, 4.00), and lifetime (OR 1.85, CI 1.11, 3.08) and past month (OR 2.70, CI 1.57, 4.64) alcohol use relative to never using alcohol.
Conclusions
Much self-harm in adolescents resolves over the course of 12 months. Young people who self-harm have high rates of other health risk behaviors associated with family and peer risks that may all be targets for preventive intervention.
Keywords: adolescence, deliberate self-harm, cross-national, longitudinal, risk factors, protective factors
The World Health Organization (WHO) has defined deliberate self-harm (DSH) as a behavior that is intended to cause self-harm but without suicide intent and having a non-fatal outcome [1]. DSH, however, is a predictor of completed suicide, [2-5] with around a quarter of those completing suicide having previously engaged in DSH [3]. Adolescents who deliberately harm themselves are of clinical concern, not only because they are at-risk for later suicide and disabilities resulting from DSH-associated injuries [6], but also because they experience other health risks at higher prevalence, including mental health and substance use problems [7].
DSH peaks in prevalence around the mid-teens before rapidly declining by young adulthood [8]. In a community sample of Australian adolescents aged 15, the twelve month prevalence for DSH was 5.1%, with prevalence higher for females [4]. Hawton and James [3] found similar results. Even greater prevalence of 12-13% have been reported in population-based studies of American youth of a similar age, with higher prevalence again for females [9].
Given the rapid rise and decline in DSH during the early-to mid-teens, gaining an understanding of the risk and protective factors for both the incidence and persistence of the behavior can help advance prevention and intervention efforts. Risk factors increase the probability of engaging in DSH, whereas protective factors decrease, mediate or moderate the effect of risk factors, [10, 11]). To date, the majority of studies examining adolescent DSH have been cross-sectional. Amongst the most consistently identified correlates of DSH are mental health problems (e.g. depression and anxiety [3, 5, 9, 12-14]). Others include antisocial behavior [5, 12], alcohol consumption [15] and low emotional control (e.g. inability to relax when feeling tense, or control one's temper) [3, 5, 9, 12]. Social contexts including peer group, family, school, and community [10] have also been linked with DSH [9, 14, 16]. Evans and colleagues [9] for example, showed family conflict is linked with DSH, particularly for females.
The present study examines a broad range of risk and protective factors for DSH incidence and presents exploratory analyses for persistence around the peak age for incidence and prevalence of self-harm. Participants were drawn from state-representative samples of adolescents in seventh and ninth grades (average ages 13 and 15 years respectively) participating in the International Youth Development Study (IYDS) in Victoria, Australia, and Washington State, in the United States (US). The IYDS is a unique cross-national study designed to overcome methodological inconsistencies in data collection that commonly bias cross-national studies of DSH [17]. Two research questions were examined: (1) Are there state differences in levels of incident and persistent DSH? and (2) To what extent do established risk factors increase incident and persistent DSH?
Methods
Participants
Participants were seventh and ninth grade students enrolled in the IYDS, a longitudinal study exploring the development of healthy and problematic behaviors in 3,876 students from Victoria, Australia and Washington State, US. In the years that the study was designed and the sample recruited, the Victorian and Washington State populations were similar in terms of population size, urbanicity, having higher than national levels of educational participation, and in having low proportions of residents living in poverty [18].
Students were first surveyed in 2002 (T1) and re-surveyed one-year later in 2003 (T2). The IYDS utilized standardized methodologies (sample recruitment, survey content, and survey administration) in each state. A two-stage cluster-sampling approach was employed in 2002: 1) public and private schools with grades 7 and 9 were randomly selected for recruitment into the study using a probability proportionate to grade-level size sampling procedure [19]; and 2) one class at the appropriate grade level was randomly selected within each school [18].
Written parental consent was obtained for all participating students prior to T1. Students also provided their assent to participate on the day of the survey. Of all eligible students across the two grade levels, 75% and 74% participated at T1 in Washington State and Victoria, respectively. The retention rate was 99% or above in both states at T2. Survey construction, student recruitment processes, and rates of student participation have been described elsewhere [18].
The data analyzed in the present paper comprised 3,876 students with complete data on the variables under study, with 1,947 seventh grade students (984 Victoria) and 1,929 ninth grade students (973 Victoria). Almost 51% of students were female. The mean age of Washington State students (14.1 years in grade 7, 15.1 years in grade 9) was significantly higher than Victorian students (13.9 years in grade 7, and 14.9 years in grade 9) in both cohorts. The Victorian State sample in grade 7 was comprised mainly of students identifying as Australian (91%) and the Washington State sample had a majority identifying as White (65%).
Procedures
Ethics approval
The University of Washington Human Subjects Review Committee and the Royal Children's Hospital Ethics in Human Research Committee provided approval for this study. Permission from relevant school district authorities and principals was obtained in each state.
Survey administration
A single survey administration protocol was used by trained survey staff at both sites. Surveys were administered to class groupings within schools and took approximately 50-60 minutes to complete. The self-report pen and paper survey was voluntary and completed by participants without any interaction or collaboration with peers. The survey included instructions on how to answer the questions (e.g. place a clear ‘X’ inside the box) and further assurances of confidentiality. These instructions and assurances were presented prior to survey administration by survey staff. Trained school personnel conducted surveys for students absent on the day of the survey, and a small percentage of surveys were completed by mail or by telephone.
Instruments
The IYDS survey was adapted from the Communities That Care self-report youth survey [11, 20, 21]. Similar versions of the survey are available elsewhere [22]. This survey includes measures of risk and protective factors for youth that previous research has shown to be valid and reliable when administered to students in sixth to twelfth grades in the US [11, 20, 21] and in Victoria [23]. The descriptive statistics and example items for all measures are listed in Table 1.
Table 1. Descriptive statistics for risk and protective factors measured at the first survey for seventh and ninth grade students in Victoria and Washington State.
| Established risk and protective factors (T1) | No. of scale items | Response options | Combined Sample (N = 3,876) | Victorian Sample (n = 1,942) | Washington State Sample (n = 1,934) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Mean (SD) | Cronbach's Alpha | Mean (SD) | Cronbach's Alpha | Mean (SD) | Cronbach's Alpha | ||||||
|
|
|||||||||||
| Individual factors | |||||||||||
| Emotional control (P)a | 4 | 1-4 (definitely no to definitely yes) | 2.68(.69) | .74 | 2.62(.69) | .72 | 2.75(.69)*** | .75 | |||
| Bullying victimization b | 1 | 1-4 (no to yes most days) | 1.61(.94) | n/a | 1.65(.96)* | n/a | 1.58(.92) | n/a | |||
| Antisocial behavior c | 9 | 1-8 (never to 40 times or more) | 1.11(.30) | .71 | 1.09(.26) | .69 | 1.13(.33)*** | .73 | |||
| Depressive symptoms d | 13 | 0-2 (Not true to true) | 1.55(.45) | .88 | 1.55(.44) | .87 | 1.55(.46) | .89 | |||
| Impulsivity e | 3 | 1-4 (definitely no to definitely yes) | 1.95(.58) | .57 | 1.97(.58)* | .56 | 1.92(.58) | .57 | |||
| Family factors | |||||||||||
| Family conflict f | 4 | 1-4 (definitely no to definitely yes) | 2.21(.85) | .79 | 2.20(.84) | .79 | 2.21(.86) | .80 | |||
| Parental overcontrol g | 2 | 1-4 (definitely no to definitely yes) | 2.27(.92) | .72 | 2.30(.89) | .71 | 2.25(.94) | .74 | |||
| Poor family management h | 9 | 1-4 (definitely no to definitely yes) | 1.67(.57) | .79 | 1.72(.56)** | .78 | 1.62(.58) | .79 | |||
|
|
|||||||||||
| SUBSTANCE USE | n | % | N | % | n | % | |||||
|
|
|||||||||||
| Alcohol use | 1 | Recoded (see text) | |||||||||
| No alcohol use | 1,577 | 40.69 | n/a | 568 | 29.25 | n/a | 1,009 | 52.17*** | n/a | ||
| No recent alcohol use | 1,116 | 28.79 | n/a | 549 | 28.27 | n/a | 567 | 29.32*** | n/a | ||
| Recent (past month) alcohol usei | 944 | 24.36 | n/a | 653 | 33.63*** | n/a | 294 | 15.05 | n/a | ||
| Binge drinkingj | 1 | Recoded (see text) | 239 | 6.17 | n/a | 172 | 8.86*** | n/a | 67 | 3.46 | n/a |
| Current cannabis use k | 1 | Recoded (see text) | 260 | 6.71 | n/a | 79 | 4.07 | n/a | 181 | 9.36*** | n/a |
| Current tobacco use l | 1 | Recoded (see text) | 412 | 10.63 | n/a | 275 | 14.16*** | n/a | 137 | 7.08 | n/a |
Note. (P) Protective factor (italics). N = sample size, SD = standard deviation.
= p < .05,
= p < .01,
p < .001.
Example item: “I know how to relax when I feel tense”
“Have you been bullied recently (teased or called names, had rumors spread about you, been deliberately left out of things, threatened physically or hurt)?”
Example item: “How many times in the past year (12 months) have you stolen something worth more than $5/10?”
Example item: “I felt miserable or unhappy”
Example item: “It's important to think before you act?”
Example item: “We argue about the same things in my family over and over”
Example item: “My parents try to control everything”
Example item: “Would your parents know if you did not come home on time?”
“In the past 30 days on how many occasions (if any) have you: Had more than just a few sips of an alcoholic beverage (like beer, wine or liquor/spirits)?”
Think back over the last 2 weeks. How many times have you had five or more drinks in a row?
“Have you used marijuana (pot, weed, grass)” in the past 30 days?
“How frequently have you smoked cigarettes in the past 30 days?”
Deliberate self-harm
DSH was measured by asking students “In the past year, have you ever deliberately hurt yourself or done anything that you knew might have harmed you or even killed you?” [4]. Response options were dichotomous, ‘Yes’ and ‘No’. When participants indicated engagement in DSH, they were asked the follow-up question, “If you answered yes, what was it that you did?” and they provided a qualitative description of their DSH. A measure of DSH was constructed by coding participant responses to exclude DSH completed to experience pleasure or thrill and identify behavior intended to physically damage one's body/person. Two trained research assistants conducted this coding using a specified protocol, resolving differences by consensus. Strong inter-rater agreement demonstrated by a Cohen's kappa of .77 for DSH was reported for independent evaluations of a random sample of 20% of coded responses [24].
Based on DSH data at the T1 and T2 surveys, two outcome variables were coded. The first outcome variable, persistent DSH, applied only to students who engaged in DSH at T1; it was assigned value 1 if the student continued to engage in DSH at T2, and value 0 if the student no longer engaged in DSH at T2. The persistence analyses were exploratory due to the small number of participants and limited power to detect differences. The second outcome variable, incident DSH, only applied to students who did not engage in DSH at T1; it was assigned value 1 if the student engaged in DSH at T2, and value 0 if the student remained not engaged in DSH at T2. The variable incident DSH is only an approximate measure, because it assumes that a student with value 1 (i.e., reported DSH at T2 but not at T1) started DSH within the period between the T1 and T2 surveys (hence labeled “incident”), and had not engaged in DSH prior to the T1 survey.
Established risk and protective factors
The analyses examined twelve established risk factors and one protective factor measured at T1 based on measures being available in the IYDS dataset that previous studies had implicated as influences for DSH [3, 5, 9, 12-14]. The established protective factor was emotional control. Risk factors included: bullying victimization; antisocial behavior; depressive symptoms; impulsivity; family conflict; parental overcontrol; poor family management; and alcohol, cannabis and tobacco use (see Table 1). The included measures comprise of previously validated items [21] that were risk or protective factors for DSH and other related adolescent problems in previous IYDS analyses [23, 25, 26].
Across all risk and protective factor scales, high scores indicated higher levels of the factor. Scores for each risk and protective factor were obtained through averaging the responses for scale items. Response options were recoded to reflect ‘Not at all’ (0) vs. ‘one or more occasion’ (1) in the past month for tobacco use and cannabis use. Participants' level of alcohol use was classified using measures of alcohol use (lifetime and past month) and binge drinking (five or more drinks in a row in the past fortnight). One variable, with four categories was created to define: no alcohol use (reference group), non-recent alcohol use (lifetime use but no use in the past month), recent (past month) alcohol use (but no binge use), and binge drinking (in the past 2 weeks). The measure created ranged from 0 (no alcohol use) to 3 (binge drinking).
Survey Response Accuracy
To determine the accuracy of students' self-reports, three items were used. Students' responses were coded as questionable if: 1) students reported ‘I was not honest all of the time’ when asked to report how honest they were when completing the survey; 2) students reported use of a fictitious drug (which was included in the survey for accuracy checking) in their lifetime or in the past month; and 3) students reported other drug use on more than 120 occasions in the past month. Fifteen students at T1, 35 students at T2, and 6 students at both surveys met the criteria for questionable responses, and were excluded from the analyses.
Statistical Analyses
STATA IC software for Windows, version 12 [27] was used to conduct all analyses. To compare the means and frequencies of the risk and protective factors between the two state samples T-tests and chi-square analyses were conducted.
Congruent with the probability proportionate to grade-level size sampling procedure [19] used for sample recruitment, sampling weights were calculated separately for each class as the inverse probability of selection in a particular class within the school grade. The sampling weights were implemented in prevalence point and interval estimation using the svy package. Prevalence estimates and 95% confidence intervals were derived using design-based estimation of proportions. Next, to compare outcome prevalence by gender and state, prevalence estimates were calculated. All prevalence estimates and measures of association (see below) used robust “information sandwich” estimates of standard errors, with adjustment for clustering of students within schools. Logistic regression model estimates were used to evaluate state and gender differences in outcome prevalence. Model adjusted proportions were projected for state-by-gender groups with age considered as a covariate fixed at the mean age for each grade level.
Third, correlations between DSH and risk and protective factors were examined to identify pairs or sets of predictor variables that were highly correlated, that might result in collinearity in logistic regression analysis.
Measures of association between risk and protective factors and DSH outcomes were examined in two sets of hierarchical logistic regression analyses. In accordance with studies examining the developmental trajectories of influences on behavior [28], risk and protective factors were grouped by domain and entered hierarchically. The first predicted incident DSH at T2 within the sub-sample reporting no DSH at T1. The second predicted persistent DSH at T2 within the sub-sample reporting T1 DSH. Predictors in these analyses were T1 grade, gender, state, and risk and protective factors. Demographic factors including state location were initially entered (Model 1) and then subsequent models were implemented to examine the effect of state differences with alcohol and drug use on DSH (Model 2); followed by T1 individual risk and protective factors (Model 3); and T1 family risk factors (Model 4).
Results
State comparisons of risk and protective factors
Table 1 presents state differences in means and frequencies of risk and protective factors. Of the 14 risk and protective factors examined, 11 factors (79%) showed state differences. Higher levels of risk for bullying victimization, impulsivity, poor family management, recent alcohol use, binge drinking and tobacco use are evident for Victorian students, relative to Washington State students. A higher level of protection for Washington State students as compared with Victorian students was found for emotional control. Relative to Victorian students, those in Washington State showed higher levels of risk for antisocial behavior, and cannabis use.
Prevalence of DSH
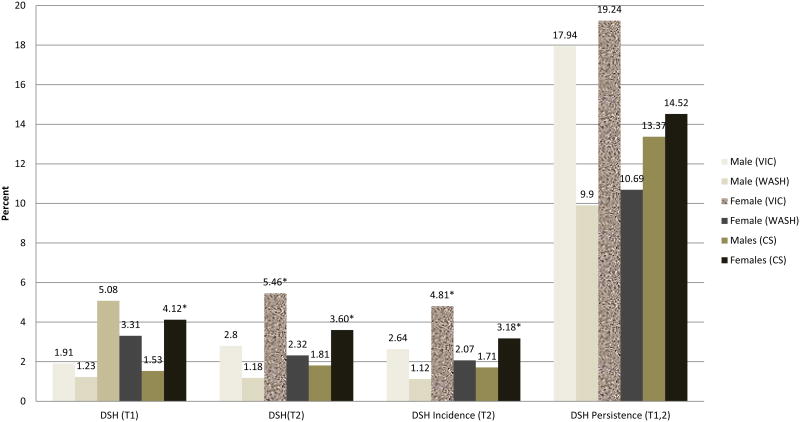
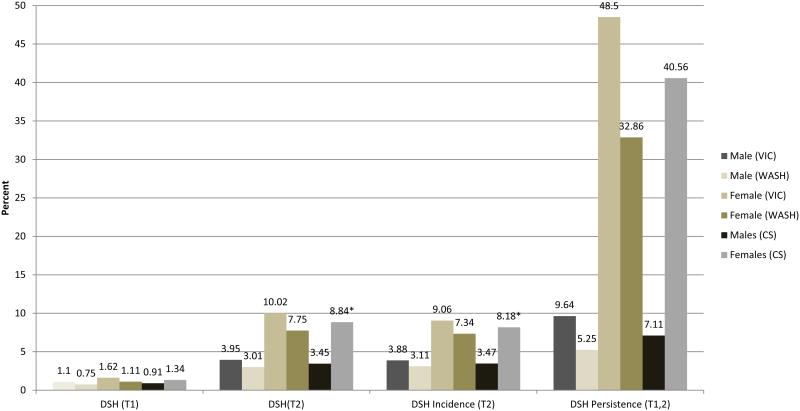
Figures 1 and 2 present the prevalence of DSH at T1 and T2, and incident and persistent DSH for 7th and 9th grade respectively. The prevalence of DSH was significantly higher for Victorian students compared to their Washington State counterparts for 7th grade female students at T1 and T2. This difference was partly due to significantly higher prevalence of DSH at T1 and T2 in Victorian females. For 7th grade students at T1 and T2, the prevalence of DSH was significantly higher for females than males in the combined Washington State-Victoria sample. In 9th grade the prevalence of persistent DSH in males was low with fewer than one in 10 males reporting continuing self-harm 12 months later (7.1%, 95% Confidence Interval [CI] .08, 87.13). Around two in five girls who self-harm continued to report self harming 12 months later (40.6%, CI 2.00, 95.81).
Figure 1. Prevalence, incidence, and persistence of DSH among students in grade 7.
Note. T1 = baseline, T2 = follow-up, DSH = deliberate self-harm. VIC = Victoria, WASH == Washington State, CS = Combined Sample. Incidence = T2 DSH/T1 no DSH, Persistence = T2 DSH/T1 DSH; *p <.05 (see text for description of comparisons).
Figure 2. Prevalence, incidence, and persistence of DSH among students in grade 9.
Note. T1 = baseline, T2 = follow-up, DSH = deliberate self-harm. VIC = Victoria, WASH == Washington State, CS = Combined Sample. Incidence = T2 DSH/T1 no DSH, Persistence = T2 DSH/T1 DSH; *p <.05 (females higher than males in the combined samples: DSH T2; DSH Incidence).
Correlations between DSH and Risk and Protective Factors
All correlations were low to moderate, with no correlation greater than .42 (range .02 to .42). No correlation approached .80, indicating no problems with multicollinearity between the examined variables [29]. All correlations with the incident DSH variable were significant at p less than .01, ranging from .06 to .37. Due to limited power, only depressive symptoms were significantly correlated with persistent DSH (refer Online Appendix 1, Table 1).
Risk and protective factors for incident and persistent DSH
Table 2 presents findings for hierarchical multivariate logistic regression models investigating risk and protective factors for incident DSH. In Model 4, living in Washington State was associated with lower odds of incident DSH (Adjusted Odds Ratio [OR] .67, CI .45, 1.00). Female gender (OR 1.93, CI 1.35, 2.76), antisocial behavior (OR 2.42, CI .1.46, 4.00), and past month depressive symptoms (OR 3.52, CI 2.37, 5.21) were all statistically significant risk factors in the adjusted models. Lifetime (non recent) (OR 1.85, CI 1.11, 3.08) or recent (past month) (OR 2.70, CI 1.57, 4.64) alcohol consumption carried higher odds relative to those reporting no alcohol use (Model 4).
Table 2. Logistic regression models investigating longitudinal risk and protective factors for incident DSH.
| INCIDENT DSH (n=3,746) | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| HIERARCHICAL MULTIVARIATE MODELS | ||||||||
|
| ||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|
| ||||||||
| Established risk and protective factors (T1) | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p |
|
|
||||||||
| Grade 7 (referent: grade 9) | .80 [.58, 1.12] | .191 | .52 [.37, .74] | <.0001 | .52 [.36, .74] | <.0001 | .52 [.36, .75] | <.0001 |
| Female Gender (referent: male) | 2.15 [1.53, 3.01] | <.0001 | 2.22 [1.60, 3.06] | <.0001 | 1.99 [1.39, 2.85] | <.0001 | 1.93 [1.35, 2.76] | <.0001 |
| Washington State (referent: Victoria) | .62 [.43, .88] | .009 | .81 [.54, 1.21] | .299 | .67 [.45, 1.01] | .056 | .67 [.45, 1.00] | .048 |
| Substance use | ||||||||
| Alcohol use classification (referent: no use) | ||||||||
| No recent alcohol use | 2.49 [1.52, 4.06] | <.0001 | 1.88 [1.15, 3.09] | .013 | 1.85 [1.11, 3.08] | .019 | ||
| Recent alcohol use | 4.11 [2.43, 6.97] | <.0001 | 2.75 [1.60, 4.73] | <.0001 | 2.70 [1.57, 4.64] | <.0001 | ||
| Binge drinking | 3.27 [1.40, 7.63] | .006 | 1.72 [.74, 4.02] | .209 | 1.73 [.73, 4.13] | .213 | ||
| Current Cannabis Use | 1.61 [.84, 3.09] | .148 | 1.15 [.55, 2.42] | .714 | 1.14 [.54, 2.39] | .736 | ||
| Current Tobacco Use | 2.52 [1.48, 4.29] | .001 | 1.61 [.96, 2.68] | .070 | 1.60 [.95, 2.71] | .079 | ||
| Individual factors | ||||||||
| Emotional Control (P) | .87 [.64, 1.18] | .381 | .88 [.65, 1.20] | .421 | ||||
| Bullying victimization | 1.03 [.85, 1.23] | .774 | 1.01 [.84, 1.21] | .925 | ||||
| Antisocial Behavior | 2.42 [1.46, 4.01] | .001 | 2.42 [1.46, 4.00] | .001 | ||||
| Depressive Symptoms | 3.40 [2.69, 5.64] | <.0001 | 3.52 [2.37, 5.21] | <.0001 | ||||
| Impulsivity | 1.31 [.93, 1.86] | .124 | 1.25 [.88, 1.79] | .211 | ||||
| Family factors | ||||||||
| Family Conflict | 1.16 [.90, 1.44] | .1161 | ||||||
| Parent Overcontrol | 1.11 [.90, 1.37] | .318 | ||||||
| Poor Family Management | .95 [.65, 1.38] | .784 | ||||||
Note. OR = odds ratio, CI = confidence interval.
DSH = deliberate self-harm, (P) Protective factor
Grade 7 (coded 0 = grade 7, 1 = grade 9 [50.23%]), Female gender (coded 0 = male, 1 = female [50.95%]), Washington State (coded 0 = Victoria, 1 = Washington State [49.90%])
For hierarchical multivariate logistic regression models of persistent DSH (n = 133), depressive symptoms (past month) predicted a three-fold increase in this behavior (Table 3, Model 4: OR 3.68, CI 1.33, 10.19) and no other predictors were significant.
Table 3. Logistic regression models investigating longitudinal risk and protective factors for persistent DSH.
| PERSISTENT DSH (n=133) | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| HIERARCHICAL MULTIVARIATE MODELS | ||||||||
|
| ||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|
| ||||||||
| Established risk and protective factors (T1) | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p |
|
|
||||||||
| Grade 7 (referent: grade 9) | 1.01 [.41, 2.48] | .981 | .99 [.39, 2.51] | .976 | 1.08 [.40, 2.94] | .874 | 1.08 [.38, 3.03] | .887 |
| Female Gender (referent: male) | 1.87 [.74, 4.80] | .178 | 1.84 [.69, 4.91] | .218 | 1.47 [.55, 3.99] | .440 | 1.47 [.54, 3.99] | .444 |
| Washington State (referent: Victoria) | .58 [.25, 1.35] | .201 | .73 [.26, 2.05] | .551 | .64 [.19, 2.11] | .456 | .64 [.19, 2.21] | .478 |
| Substance use | ||||||||
| Alcohol use classification (referent: no use) | ||||||||
| No recent alcohol use | .94 [.15, 6.01] | .949 | .93 [.13, 6.86] | .943 | .87 [.11, 6.80] | .897 | ||
| Recent alcohol use | 1.87 [.33, 10.70] | .478 | 1.78 [.26, 12.11] | .552 | 1.76 [.25, 12.46] | .570 | ||
| Binge drinking | 2.01 [.31, 12.89] | .456 | 2.27 [.32, 16.03] | .407 | 2.16 [.30, 15.59] | .442 | ||
| Current Cannabis Use | .74 [.18, 3.04] | .670 | .64 [.11, 3.68] | .618 | .63 [.10, 3.89] | .615 | ||
| Current Tobacco Use | .97 [.36, 2.62] | .957 | .85 [.28, 2.55] | .767 | .79 [.25, 2.48] | .689 | ||
| Individual factors | ||||||||
| Emotional Control (P) | .90 [.51, 1.58] | .708 | .91 [.50, 1.65] | .753 | ||||
| Bullying victimization | .89 [.65, 1.22] | .458 | .88 [.64, 1.21] | .428 | ||||
| Antisocial Behavior | 1.23 [.30, 5.09] | .772 | 1.18 [.26, 5.37] | .827 | ||||
| Depressive Symptoms | 3.88 [1.42, 10.56] | .009 | 3.68 [1.33, 10.19] | .013 | ||||
| Impulsivity | .87 [.33, 2.28] | .772 | .79 [.29, 2.17] | .643 | ||||
| Family factors | ||||||||
| Family Conflict | 1.22 [.71, 2.11] | .464 | ||||||
| Parent Overcontrol | .90 [.53, 1.53] | .691 | ||||||
| Poor Family Management | 1.04 [.46, 2.36] | .930 | ||||||
Note. OR = odds ratio, CI = confidence interval.
DSH = deliberate self-harm, (P) Protective factor
Grade 7 (coded 0 = grade 7, 1 = grade 9 [69.70%]), Female gender (coded 0 = male, 1 = female [78.79%]), Washington State (coded 0 = Victoria, 1 = Washington State [30.30%])
Discussion
This is one of the few prospective studies of adolescent DSH. Consistent with prior studies, DSH is relatively common but has a high rate of resolution, particularly in males. Around two in five females continued to self-harm twelve months later whereas less than one in 10 males continued to do so. The clearest risk factors for incident DSH were recent depressive symptoms, past year antisocial behavior, living in Victoria, and being female. In addition, lifetime and recent (past month) alcohol use predicted new episodes of DSH relative to those who had never used alcohol. Adjustment for depressive symptoms, antisocial behavior and alcohol use did not completely explain the lower prevalence of new cases of DSH in Washington State. Depressive symptoms was the only factor associated with persistent DSH at either bivariate or multivariate levels.
The same recruitment and survey methods were used to investigate and compare the prevalence of incident and persistent DSH, and the influence of established risk factors on these measures, for state-representative samples of students in Victoria and Washington State. Although Victorian prevalence of DSH in females was higher than that in Washington State females, these differences became statistically significant only when the 7th grade cohort entered 8th grade. The finding of higher DSH prevalence amongst Victorian adolescents is consistent with the limited previous studies of Australian students [30]. Other studies have shown the prevalence of adolescent suicide is greater in Australia compared to the US [31].
Consistent with earlier cross-sectional findings, we found many variables were longitudinally related to DSH at the bivariate level. However, in the adjusted analyses, this study identified only mental health problems (depressive symptoms) [3, 9, 12], antisocial behavior [5, 12], and alcohol use [32], to be uniquely predictive of incident DSH. Persistence was higher (over 40%) for girls at grade 9, and girls had higher DSH prevalence than boys at grades 7, 8 and 10, adding specification to prior observations of higher DSH for females [3, 4, 9, 12].
Depressive symptoms were the only clear factor predictive of persistent DSH, probably in part due to the relatively small number of cases in this analysis. It does suggest that young people who self-harm and who have conspicuous associated mental health problems are a group at higher risk not only of the morbidities associated with self-harm but potentially for suicide as well.
DSH does cluster with other health risks, including alcohol and antisocial behavior as well as risks in the family and peer social contexts. It seems possible these risks in the social context have effects mediated through antisocial behavior, depressive symptoms, and perhaps alcohol use. For these reasons, these behaviors and symptoms remain important targets for preventive intervention.
Study Limitations and Strengths
The longitudinal design and comprehensive measures enabled a wider range of risk factors for the course of DSH to be investigated relative to prior studies. Although the study is unique in surveying cross-national, state-representative samples followed with little attrition, several limitations are acknowledged. Due to the low prevalence of persistent DSH (only 130 cases), analyses may have been underpowered to detect significant effects, making these findings exploratory. A longer time frame would ideally be required to study the incidence and persistence/desistence of DSH. The analyses conducted should be replicated in future studies. Additionally, analyses relied exclusively on student self-report data; however, the survey measures used have demonstrated good reliability and validity in large samples [11, 20, 21], and longitudinal validity [23]. Further, the factor structure of all measures has been validated using confirmatory factor analyses [21], and all measures have been previously used in other analyses of the larger dataset examining risk and protective factors among the Washington State and Victorian samples in the IYDS [23, 25, 26].
There may be stigma associated with reporting DSH in a survey where identity details were known to the research team, despite the assurance of confidentiality and anonymity to participants. Importantly, the survey was completed by participants without interaction with or collaboration with peers, and included further assurances of confidentiality that were presented prior to administration by study staff.
An associated limitation relates to the approximate measure of incident DSH. In this study, the report of no DSH in 12 months prior to T1 combined with DSH at T2 was used to define incident DSH, and assumed that there was no DSH prior to the T1 assessment. The measure does not take into consideration that DSH may have occurred in the years prior to that assessed by the survey item. Given the study is one of few examining longitudinal patterns, there is no clear basis to estimate to what extent DSH may have occurred prior to our assessment period. However, a strength of this measure is its suitability for large epidemiologic studies [24]. Although the results of this study are generalizable only to the state and grade levels examined, previous analyses suggest the cohorts are similar to national samples in the two countries [18, 20, 23].
Study Implications
The present study used comparable longitudinal data from two state samples in two different countries to report prevalence and investigate risk and protective factors for incident DSH and to complete an exploratory analysis of persistent DSH among adolescents. The findings of the present study suggest that DSH in adolescents mostly resolved over the course of 12 months. In common with previous findings, adolescents engaging in DSH with associated depressive symptoms were more likely to be a high risk group for persistence suggesting greater suicide risk [3, 9, 14]. The present findings confirm that incident DSH is clustered with antisocial behavior [5, 12], alcohol use [15], and depressive symptoms [9, 12] that may each offer preventive intervention opportunities. Strategies addressing these variables may not only reduce DSH but have broader health benefits on other adolescent problems. The findings revealed cross-national differences in DSH that were not completely explained by the factors included in our models, warranting further research attention.
Supplementary Material
Online Appendix 1, Table 1: Correlation matrix for incident and persistent DSH and established risk and protective factors.
Acknowledgments
Data collection for this research was supported through a grant from the National Institute on Drug Abuse (DA-012140-05) while data analysis was supported through a grant from the National Institute on Alcohol Abuse and Alcoholism (1R01AA017188-01), National Institutes of Health, United States Department of Health and Human Services; Richard F. Catalano, PI. Data analysis was also supported through grants from the: National Health and Medical Research Council (Projects 491241; 594793; and 1047902); the Australian Research Council (DP109574); and the Australian Health and Medical Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
The work of Dr. Heerde is supported by funding provided through the Learning Sciences Institute Australia at Australian Catholic University.
Footnotes
Implications and contributions: Adolescent DSH clusters with depressive symptoms, alcohol use, and antisocial behaviors. Adolescents displaying these symptoms and behaviors might also be targeted for interventions to reduce DSH. Those who self-harm in the context of associated mental health problems are at high risk for persistence, suggesting greater suicide risk.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jessica A. Heerde, Email: jessica.heerde@acu.edu.au.
John W. Toumbourou, Email: john.toumbourou@deakin.edu.au.
Sheryl A. Hemphill, Email: sheryl.hemphill@acu.edu.au.
Todd I. Herrenkohl, Email: tih@u.washington.edu.
George C. Patton, Email: george.patton@rch.org.au.
Richard F. Catalano, Email: catalano@u.washington.edu.
References
- 1.National Collaborating Centre for Mental Health. Self-harm: the short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care 2004. British Psychological Society; 2004. [PubMed] [Google Scholar]
- 2.Gratz KL. Risk factors for and functions of deliberate self-harm: An empirical and conceptual review. Clin Psychol. 2003;10:192–205. [Google Scholar]
- 3.Hawton K, James A. ABC of adolescence: Suicide and deliberate self harm in young people. BMJ. 2005;330:891–894. doi: 10.1136/bmj.330.7496.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patton GC, Harris R, Carlin JB, et al. Adolescent suicidal behaviours: a population-based study of risk. Psychol Med. 1997;27:715–724. doi: 10.1017/s003329179600462x. [DOI] [PubMed] [Google Scholar]
- 5.Portzky G, van Heeringen K. Deliberate self-harm in adolescents. Curr Opin Psychiatry. 2007;20:337–342. doi: 10.1097/YCO.0b013e3281c49ff1. [DOI] [PubMed] [Google Scholar]
- 6.Harrison J, Moller J, Bordeaux S. Youth suicide and self-injury Australia. Adelaide, Australia: Research Centre for Injury Studies; 1997. [Google Scholar]
- 7.Mars B, Heron J, Crane C, et al. Clinical and social outcomes of adolescent self harm: population based birth cohort study. BMJ. 2014;349:g5954. doi: 10.1136/bmj.g5954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate self-harm in a nonclinical population: Prevalence and psychological correlates. Am J Psychiatry. 2003;160:1501–1508. doi: 10.1176/appi.ajp.160.8.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans E, Hawton K, Rodham K. Factors associated with suicidal phenomena in adolescents: A systematic review of population-based studies. Clin Psychol Rev. 2004;24:957–979. doi: 10.1016/j.cpr.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Catalano RF, Hawkins JD. The Social Development Model: A Theory of Antisocial Behavior. In: Hawkins JD, editor. Delinquency and Crime: Current theories. New York: Cambridge; 1996. pp. 149–197. [Google Scholar]
- 11.Pollard JA, Hawkins JD, Arthur MW. Risk and protection: are both necessary to understand diverse behavioral outcomes in adolescence? Soc Work Res. 1999;23:145–158. [Google Scholar]
- 12.Fliege H, Lee JR, Grimm A, et al. Risk factors and correlates of deliberate self-harm behavior: A systematic review. J Psychosom Res. 2009;66:477–493. doi: 10.1016/j.jpsychores.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Skegg K. Self-harm. Lancet. 2005;366:1471–1483. doi: 10.1016/S0140-6736(05)67600-3. [DOI] [PubMed] [Google Scholar]
- 14.Webb L. Deliberate self-harm in adolescence: a systematic review of psychological and psychosocial factors. J Adv Nurs. 2002;38:235–244. doi: 10.1046/j.1365-2648.2002.02174.x. [DOI] [PubMed] [Google Scholar]
- 15.Rossow I, Ystgaard M, Hawtom K, et al. Cross-national comparisons of the association between alcohol consumption and deliberate self-harm in adolescents. Suicide Life Threat Behav. 2007;37:605–615. doi: 10.1521/suli.2007.37.6.605. [DOI] [PubMed] [Google Scholar]
- 16.Wagner BM. Family risk factors for child and adolescent suicidal behavior. Psychol Bull. 1997;121:246–298. doi: 10.1037/0033-2909.121.2.246. [DOI] [PubMed] [Google Scholar]
- 17.Pirkis JE, Irwin C, Brindis C, et al. Adolescent substance use: beware of international comparisons. J Adolesc Health. 2003;33:279–286. doi: 10.1016/s1054-139x(03)00209-x. [DOI] [PubMed] [Google Scholar]
- 18.McMorris BJ, Hemphill SA, Toumbourou JW, et al. Prevalence of substance use and delinquent behaviour in adolescents from Victoria, Australia and Washington State, United States. Health Educ Behav. 2007;34:634–650. doi: 10.1177/1090198106286272. [DOI] [PubMed] [Google Scholar]
- 19.Kish L. Survey Sampling. New York, NY: John Wiley & Sons; 1965. [Google Scholar]
- 20.Arthur MW, Hawkins JD, Pollard JA, et al. Measuring risk and protective factors for substance use, delinquency, and other adolescent problem behaviors: The Communities That Care Youth Survey. Eval Rev. 2002;26:575–601. doi: 10.1177/0193841X0202600601. [DOI] [PubMed] [Google Scholar]
- 21.Glaser RR, Lee Van Horn M, Arthur MW, et al. Measurement Properties of the Communities That Care Youth Survey Across Demographic Groups. J Quant Criminol. 2005;21:73–102. [Google Scholar]
- 22.Social Development Research Group. Communities That Care Youth Survey. Available at: http://www.sdrg.org/ctcresource/CTC_Youth_Survey_2006.pdf.
- 23.Hemphill SA, Heerde JA, Herrenkohl TI, et al. Risk and protective factors for adolescent substance use in Washington State, the United States and Victoria, Australia: A longitudinal study. J Adolesc Health. 2011;49:312–320. doi: 10.1016/j.jadohealth.2010.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patton GC, Hemphill SA, Beyers JM, et al. Pubertal stage and deliberate self-harm in adolescents. J Am Acad Child Adolesc Psychiatry. 2007;46:508–514. doi: 10.1097/chi.0b013e31803065c7. [DOI] [PubMed] [Google Scholar]
- 25.Hemphill SA, Kotevski A, Herrenkohl TI, et al. Longitudinal consequences of adolescent bullying perpetration and victimisation: A study of students in Victoria, Australia. Crim Behav Ment Health. 2011;21:107–116. doi: 10.1002/cbm.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hemphill SA, Smith R, Toumbourou JW, et al. Modifiable determinants of youth violence in Australia and the United States: A longitudinal study. Aust N Z J Criminol. 2009;42:289–309. doi: 10.1375/acri.42.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.StataCorp. Stata: Statistics/data analysis. College Station, TX: StataCorp; 2009. 10:1 IC edition edition. [Google Scholar]
- 28.Loeber R, Farrington DP. Young children who commit crime: Epidemiology, developmental origins, risk factors, early interventions, and policy implications. Dev Psychopathol. 2000;12:737–762. doi: 10.1017/s0954579400004107. [DOI] [PubMed] [Google Scholar]
- 29.Tabachnick BG, Fidell LS. Using multivariate statistics. 6th. Boston, United States of America: Pearson Education Inc; 2013. [Google Scholar]
- 30.Madge N, Hewitt A, Hawton K, et al. Deliberate self-harm within an international community sample of young people: comparative findings from the child & adolescent self-harm in Europe (CASE) study. J Child Psychol Psychiatr. 2008;49:667–677. doi: 10.1111/j.1469-7610.2008.01879.x. [DOI] [PubMed] [Google Scholar]
- 31.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 32.Bagge CL, Sher KJ. Adolescent alcohol involvement and suicide attempts: Toward the development of a conceptual framework. Clin Psychol Rev. 2008;28:1283–1296. doi: 10.1016/j.cpr.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Appendix 1, Table 1: Correlation matrix for incident and persistent DSH and established risk and protective factors.