Abstract
Context
Cataract surgery is one of the most frequently performed intra-ocular surgeries, of these manual Small Incision Cataract Surgery (SICS) is a time tested technique of cataract removal.
Any corneal incisional surgery, including cataract surgery, can induce dry eye postoperatively. Various factors have been implicated, of which oneis the inflammation induced by the surgery.
Lactoferrin, a glycoprotein present in tears is said to have anti-inflammatory effects, and promotes cell growth. It has been used orally in patients of immune mediated dry eye to alleviate symptoms.
Aim
This study was aimed to evaluate the dry eyes induced by manual Small Incision Cataract Surgery, and the effect if any, of oral lactoferrin on the dry eyes.
Settings and Trial Design
A single centre, prospective randomised controlled trial with a concurrent parallel design. The study was carried out on patients presenting in the OPD of Rohilkhand Medical College hospital for cataract surgery.
Materials and Methods
Sixty four patients of cataract surgery were included in the study. Patients with pre-existing dry eyes, ocular disease or systemic disease predisposing to dry eyes were excluded from the study. The selected patients were assigned into two groups by simple randomisation-Control Group A-32 patients that did not receive oral lactoferrin postoperatively.
Group B-32 patients that received oral lactoferrin 350 gm postoperatively from day 1 after SICS.
All patients were operated for cataract and their pre and postoperative (on days 7, 14, 30 and 60) dry eye status was assessed using the mean tear film break-up time (tBUT) and Schirmer test 1 (ST 1) as the evaluating parameters. Subjective evaluation of dry eye was done using Ocular Surface Disease Index (OSDI) scoring. Data was analysed for 58 patients, as 6 did not complete the follow up.
Statistical Analysis
Unpaired t-test was used to calculate the p-values.
Result
There was a statistically significant difference between the tBUT values of the Control and Lactoferrin group from day 14 onwards. The tBUT of control group on day 60 was 7.86 (±0.86) seconds as compared to 13.9(± 0.99) seconds in the lactoferrin group. The Schirmer test 1 values also showed a statistically significant difference between the two groups- 15.86 (± 5.83) seconds in the control group versus 30.9 (±1.66) in the lactoferrin group on day 60. OSDI score showed 42.8% patients complaining of at least mild dry eye symptoms in the control group, as compared to 26.6% patients in the lactoferrin group on day 60.
Conclusion
Small Incision Cataract Surgery induces dry eye postoperatively. Oral lactoferrin given postoperatively improves tear film status and dry eye after cataract surgery.
Keywords: Schirmer test 1, Tear film break-up time, SICS, Post-operative dry eye
Introduction
Both cataract and refractive surgeries are known to induce postoperative dry eyes. While vigorous treatment of dry eyes is the norm in refractive surgeries, the same is not true for cataract patients with surgeons focussing more on the visual outcome. This results in dissatisfied patients complaining of increased grittiness, foreign body sensation and dryness postoperatively despite a good visual outcome [1–4].
The postoperative dry eyes in cataract patients are multifactorial. Most patients are of the elderly age group and are thus more predisposed to developing dry eye. Furthermore, the inflammation caused by the surgery, the distortion of the ocular surface, the cutting of the corneal nerves by the incision and the preservatives in the eye drops used postoperatively, all exacerbate the condition [3,5–8].
Lactoferrin, a glycoprotein present in tears, has several functions, including anti-inflammatory and antimicrobial, as well as promotion of cell growth, antiangiogenic and antitumoural actions. Studies have reported a correlation between low tear lactoferrin levels and primary, secondary as well as non-Sjogren’s dry eyes [9]. Furthermore oral lactoferrin has been used as a treatment in Sjogren’s and non-Sjogren dry eyes with good results. But there are very few studies elaborating the use of oral lactoferrin in postoperative dry eye. Current stress on postoperative treatment of dry eyes is on lubricating agents and tear substitutes, and anti-inflammatory agents like steroids and cyclosporine eye drops.
This study was carried out with the aim of evaluating the dry eye after manual Small Incision Cataract Surgery (SICS), and the effect if any of oral lactoferrin on post cataract surgery dry eyes.
Materials and Methods
This study was a single centre, non-blinded, prospective randomised controlled trial with a concurrent parallel design, carried out on 64 patients of senile cataract presenting in our OPD (Department of Ophthalmology, Rohilkhand Medical College and hospital) for cataract surgery.
Patients with pre-existing dry eyes or any other ocular diseases or ocular injury were excluded from the study. Patients having systemic diseases predisposing to dry eyes like diabetes mellitus, rheumatoid arthritis, Sjögren’s syndrome, sarcoidosis, HIV, thyroid disorder, SLE were also excluded. Patients having undergone ocular surgery or on topical lubricants during previous 6 months were also rejected.
An informed consent was taken from all selected patients and they were allotted into two groups by simple random sampling-Control Group A -32 patients that did not receive oral lactoferrin postoperatively. Lactoferrin Group B -32 patients that received oral lactoferrin 350 mg postoperatively from day 1 after SICS.
The selected patients were evaluated for tear film status one day prior to cataract surgery (day 0) by using tBUT and ST 1.
All patients were operated for cataract by SICS using a 6mm-6.5mm sclero-corneal tunnel incision 1.5mm from the limbus. A rigid IOL was implanted at the end of surgery. All surgeries were incident free.
Oral lactoferrin 350 mg once daily was started in GROUP B patients from day 1 after surgery. Both groups continued to receive the routine postoperative medications.
Postoperative dry eye status was re-assessed using the mean tear film break-up time (tBUT) and Schirmer test 1 (ST 1) on day 7, 14, 30 and 60.
The Tear film break-up time (tBUT) was performed using a commercially available fluorescein strip moistened with sterile non-preserved saline & inserting in the inferior tarsal conjunctiva. The subject was instructed to blink 3 times, and then look straight without any blink. Tear film was observed on a slit lamp using cobalt blue filter under broad beam. The interval between the last blink and the appearance of the first corneal dry spot was recorded in seconds with a stop watch. This procedure was repeated 3 times and the mean value was taken for analysis. A tBUT value less than 10 seconds was taken as abnormal.
The Schirmer Test 1 (ST 1) was performed using standardized Whatmann filter paper (no.41) which is 5mm wide & 35mm in length. It was folded from the edge and placed in the lateral third of the lower eyelid. Eye was kept open & upwardly fixated with allowance for blinking. The distance of strip moistened from 5mm fold to the distal end of wetting on the strip was recorded after 5 min. A reading of less than 10 mm was considered abnormal.
All the tests were carried out under optimum environmental conditions to preclude any other effect on tear film status by temperature, humidity and light or air movement.
Subjective evaluation of dry eye was done using Ocular Surface Disease Index (OSDI) questionnaire scoring. The severity of dry eye status was evaluated for each patient employing the clinical parameters of tBUT and ST-1 along with the subjective scores as illustrated in OSDI questionnaire.
Statistical Analysis
Unpaired t-test was used to calculate the p-values.
Result
This study included 64 patients who underwent Manual SICS. Data was analysed for 58 patients (28 in Control Group A and 30 in Lactoferrin Group B), as 6 did not complete the follow up [Table/Fig-1].
[Table/Fig-1]:
Study group
There were 28 females and 30 male patients. The age ranged from 45 to 76 years with a mean age of 59.6 years.
The mean tear film break-up time in the Control Group A: [Table/Fig-2] showed a progressive decline from preoperative levels up to day 30. The fall was steeper in the first month and much more gradual in the second month. The mean tBUT on day 60 was 7.86 seconds (SD=0.86secs) as compared to 12.64 secs (SD= 1.7) preoperatively. In the Lactoferrin Group B: The mean tBUT value showed an initial mild decline from preoperative levels falling from 11.7 (SD =1.95) to 10.3 (SD=2.06) seconds in the first week, but thereafter showed a progressive rise being 13.9 (SD=) seconds on day 60. The p-value calculated using the unpaired t-test showed a statistically significant difference (p < 0.001) between the mean tBUT values of Group A and Group B on days 14, 30 and 60.
[Table/Fig-2]:
Analysis of mean tBUT values from day 0 to day 60
| Day 0 | Day 7 | Day 14 | Day 30 | Day 60 | |
|---|---|---|---|---|---|
| tBUT control Group A |
12.64 (1.7)secs | 11.21 (1.58) secs | 9.57 (1.09)secs | 8.43 (1.28)secs | 7.86 (0.86) secs |
| tBUT lactoferrin Group B |
11.7 (1.95)secs | 10.3 (2.06)secs | 12.10 (2.02)secs p<0.001 |
13.10 (1.37) secs p<0.0001 |
13.9 (0.99) secs p<0.0001 |
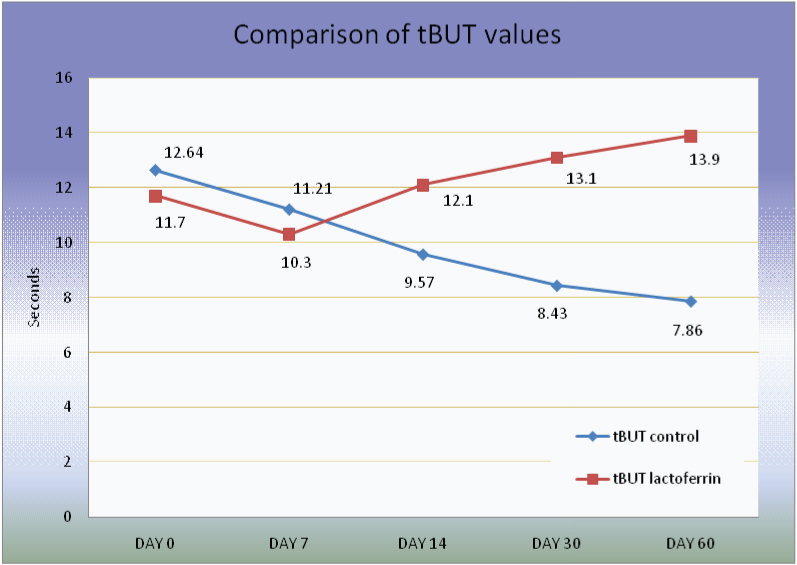 | |||||
The Schirmer test 1 values in the Control Group A revealed similar falling tear film parameters. The mean ST 1 value on day 0 was 24.64 (SD= 6.45) seconds. It declined from day 7 onwards to a final value of 15.86 (± 5.83) seconds on day 60. In the Lactoferrin Group B on the other hand the ST 1 values showed a progressive rise from day 7 onwards. There was a statistically significant difference (p < 0.001) between the mean tBUT values of Group A and Group B on days 30 and 60 [Table/Fig-3].
[Table/Fig-3]:
Analysis of mean ST 1 values from day 0 to day 60
| Day 0 | Day 7 | Day 14 | Day 30 | Day 60 | |
|---|---|---|---|---|---|
| Schirmer 1 control |
24.64 (6.45) secs |
24.07 (6.39) secs |
20.71 (5.65) secs |
17.71 (5.28) secs |
15.86 (5.83) secs |
| Schirmer 1 lactoferrin |
22.30 (5.64) secs |
27.30 (4.79) secs |
26.9 (5.13) secs |
29.30 (3.50) secs p= 0.0001 |
30.9 (1.66) secs p=0.0001 |
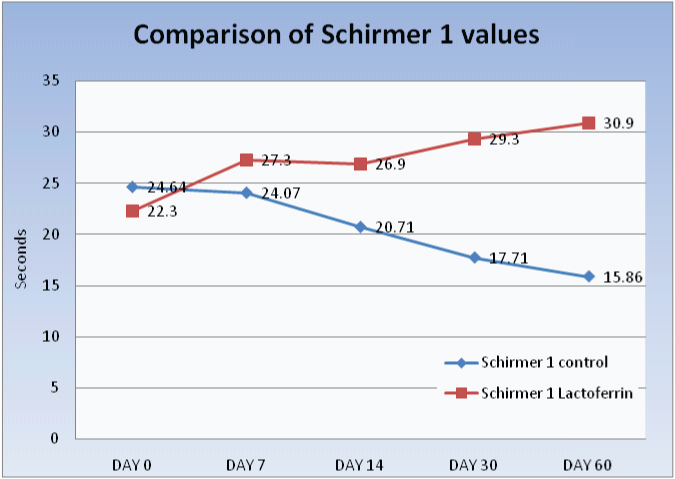 | |||||
On a subjective basis, utilising the OSDI questionnaire, 12 out of 28 patients (42.8%) in the Control Group A were found to have at least mild symptoms of dry eye on day 60. By comparison only 8 out of 30 patients (26.6%) had subjective symptoms of at least mild dry eye in the Lactoferrin Group B. None of the subjects reported any side effects related to lactoferrin (diarrhoea, loss of appetite, skin rash or constipation) during the study.
Discussion
Dry eye disease (DED) is said to affect 5% to 17% of the US population [10]. Other epidemiological studies have reported that over 6% of population over 40 and 15% over the age of 65 years suffer from dry eyes. Most studies have shown an increasing prevalence with age [11–13]. In the Indian context this prevalence can be expected to be higher taking the hot dry climate into account. A study of dry eyes by Gupta N et al., [14] of 400 consecutive patients aged 40 of years and above in North India found a prevalence of 29%, with higher prevalence in women and elderly. Patients presenting for cataract surgery are therefore more likely to be at risk for dry eyes due to elderly age group. Another study states that “the burden of DED to the patient can be substantial, impacting visual function, daily activities, social and physical functioning, workplace productivity, and quality of life” [15].
Dry eye occurring postoperatively after cataract or refractive surgeries has been established by many studies [1–4]. A study by Levitt AE showed persistence of dry eye symptoms for up till 6 months after Lasik surgery [16]. In our study, similar findings of surgically induced dry eyes were found in the control group A which persisted for up to two months after surgery. Various factors have been implicated in cataract surgery inducing dry eye, like cutting of corneal nerves, inflammation, ocular surface distortion, increased exposure time to microscope light and effect of preservatives in eye drops used postoperatively [3,5–8].
To combat this surgically induced dry eye, and reduce its severity and duration, long-term management of the tear film and ocular surface has been advocated [17]. Various modalities have been employed, including tear substitutes, and pre and postoperative anti-inflammatory drops like cyclosporine 0.05% [18,19], all reporting significant improvement in tear film stability after surgery for age related cataract.
Lactoferrin, a multifunctional glycoprotein secreted not only in tears, but also in mother’s milk, nasal secretions and saliva has anti-inflammatory and anti-microbial properties and is a component of the immune response. A study by Danjo et al., showed a significant negative correlation between dry eye and tear lactoferrin levels [9]. Oral lactoferrin has been effectively used in treating Sjogren’s and non Sjogren’s dry eyes. In a study by Dogru M et al., in Japan, 270mg/ day oral lactoferrin supplementation was given to 7 patients of Sjogren’s syndrome [20]. All patients showed improvements in dry eye symptoms and tear film stability. This improvement reverted on cessation of treatment. The use of oral lactoferrin in manual SICS induced dry eyes is not well documented. This study was therefore planned to fill this lacuna of knowledge.
Studies have shown clinically significant change in Schirmer test 1 values for many months after LASIK [21,22]. Our study found that the dry eye induced by SICS, as measured by tBUT and Schirmer test 1 continued to show decreased values as compared to preoperative levels till two months postoperatively. This compared well with a study of Cetinkaya S et al., which also demonstrated decreasing tBUT and Schirmer test 1 values for uptill one month after phacoemulsification surgery [2]. In another study by Cho YK et al., they noted that dry eye test values like tBUT and Schirmer test 1 were worse up till two months after cataract surgery, a finding that co-relates well with our study [3]. The mean tBUT values in their study changed from 10.86 seconds preoperatively to 6.8 seconds at the end of 2 months, as compared to 12.64 second and 7.86 seconds respectively in our study. The mean Schirmer test 1 values showed a decrease of 21.4% from baseline preoperative values at the end of two months. In our study they showed a decrease of 35.6% from baseline preoperative values in a similar time frame. But in the Lactoferrin Group B, such decrease in tear film parameters was not noted in our study. This group showed statistically significant higher values for tBUT and Schirmer test 1 postoperatively.
Subjective evaluation by OSDI questionnaire showed a larger percentage of patients displaying symptoms of dry eye in the control group as compared to the lactoferrin group.
This provides evidence that oral lactoferrin given postoperatively after cataract surgery favourably alters the course of postoperative dry eyes, improves the tear film parameters and subjective symptoms.
Limitations
This study used tBUT and Schirmer test 1 as evaluating parameters as they are quick, cheap and easy to perform. While tBUT is a valuable diagnostic aid for dry eye diseases, and it is generally agreed that a tBUT less than 10 seconds adequately reflects tear film instability, Schirmer test 1 on the other hand, is only moderately sensitive and does not provide good repeatability [23]. Another limitation for this study is that agreement between subjective symptoms and objective tests is not exact. Further studies may be required in future with tear protein assays which are more sensitive and specific to detect dry eyes
Conclusion
Manual small incision cataract surgery induces dry eye postoperatively. Oral lactoferrin has been shown to positively influence the tear film stability as well as alleviate dry eye symptoms of post cataract surgery patients. Therefore such patients may benefit from the addition of oral lactoferrin along with routine postoperative care and tear substitutes to give clinical as well as symptomatic relief of dry eyes postoperatively.
Financial or Other Competing Interests
None.
References
- [1].Shoja MR, Besharati MR. Dry eye after LASIK for myopia: Incidence and risk factors. Eur J Ophthalmol. 2007;17(1):1–6. doi: 10.1177/112067210701700101. [DOI] [PubMed] [Google Scholar]
- [2].Cetinkaya S, Mestan E, Acir NO, Cetinkaya YF, Dadaci Z, Yener HI. The course of dry eye after phacoemulsification surgery. BMC Ophthalmol. 2015;15(1):68. doi: 10.1186/s12886-015-0058-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cho YK, Kim MS. Dry eye after cataract surgery and associated intraoperative risk factors. Korean J Ophthalmol. 2009;23(2):65–73. doi: 10.3341/kjo.2009.23.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dodia K, Bapat S, Chudasama RK. Dry eye risk factors after phacoemulsification cataract surgery at a secondary care hospital. IJHAS. 2013;2(4):242–45. [Google Scholar]
- [5].Lane HA, Zaidman GW, Pallin DJ. Changes in corneal sensation and reflex tear secretion following excimer laser in situ keratomileusis (LASIK) Invest Ophthalmol Vis Sci. 2001;42:S493. [Google Scholar]
- [6].Linna TU, Vesaluoma MH, Perez-Santonja JJ, Petroll WM, Alio JL, Tervo TM. Effect of myopic LASIK on corneal sensitivity and morphology of sub-basal nerves. Invest Ophthalmol Vis Sci. 2000;41:393–97. [PubMed] [Google Scholar]
- [7].Slowik C, Somodi S, Richter A, Guthoff R. Assessment of corneal alterations following laser in situ keratomileusis by confocal slit scanning microscopy. Ger J Ophthalmol. 1996;5:526–31. [PubMed] [Google Scholar]
- [8].Li XM, Hu L, Hu J, Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9 Suppl 1):S16–20. doi: 10.1097/ICO.0b013e31812f67ca. [DOI] [PubMed] [Google Scholar]
- [9].Danjo Y, Lee, M, Horimoto, K, Hamano T. Ocular surface damage and tear lactoferrin in dry eye syndrome. ActaOphthalmologica. 1994;72(4):433–37. doi: 10.1111/j.1755-3768.1994.tb02791.x. [DOI] [PubMed] [Google Scholar]
- [10].Grubbs JR, Tolleson-Rinehart S, Huynh K, Davis RM. A review of quality of life measures in dry eye questionnaires. Cornea. 2014;33(2):215–18. doi: 10.1097/ICO.0000000000000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology. 1998;105:1114–19. doi: 10.1016/S0161-6420(98)96016-X. [DOI] [PubMed] [Google Scholar]
- [12].Schein OD, Munoz B, Tielsch JM, Bandeen-Roche K, West S. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124:723–28. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- [13].Bjerrum KB. Keratoconjunctivitissicca and primary Sjogren’s syndrome in a Danish population aged 30-60 years. Acta Ophthal mol Scand. 1997;75:281–86. doi: 10.1111/j.1600-0420.1997.tb00774.x. [DOI] [PubMed] [Google Scholar]
- [14].Gupta N, Prasad I, Jain R, D’Souza P. Estimating the prevalence of dry eye among Indian patients attending a tertiary ophthalmology clinic. Ann Trop Med Parasitol. 2010;104(3):247–55. doi: 10.1179/136485910X12647085215859. [DOI] [PubMed] [Google Scholar]
- [15].Pflugfelder SC. Prevalence, burden, and pharmacoeconomics of dry eye disease. Am J Manag Care. 2008;14(3 Suppl):S102–06. [PubMed] [Google Scholar]
- [16].Levitt AE, Galor A, Weiss JS, Felix ER, Martin ER, Patin DJ, et al. Chronic dry eye symptoms after LASIK: parallels and lessons to be learned from other persistent postoperative pain disorders. Mol Pain. 2015;11:21. doi: 10.1186/s12990-015-0020-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Albietz JM, Lenton LM. Management of the ocular surface and tear film before, during, and after laser in situ keratomileusis. J Refract Surg. 2004;20(1):62–71. doi: 10.3928/1081-597X-20040101-11. [DOI] [PubMed] [Google Scholar]
- [18].Chung YW, Oh TH, Chung SK. The effect of topical cyclosporine 0.05% on dry eye after cataract surgery. Korean J Ophthalmol. 2013;27(3):167–71. doi: 10.3341/kjo.2013.27.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Yao K, Bao Y, Ye J, Lu Y, Bi H, Tang X, et al. Efficacy of 1% carboxymethylcellulose sodium for treating dry eye after phacoemulsification: results from a multicenter, open-label, randomized, controlled study. BMC Ophthalmol. 2015;15:28. doi: 10.1186/s12886-015-0005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Dogru M, Matsumoto Y, Yamamoto Y, et al. Lactoferrin in Sjögren’s syndrome. Ophthalmology. 2007;114:12, 2366–67. doi: 10.1016/j.ophtha.2007.06.027. [DOI] [PubMed] [Google Scholar]
- [21].Lee JB, Ryu CH, Kim JH, Kim EK, Kim HB. Comparison of tear secretion and tear film instability after photorefractive keratectomy and laser in situ keratomileusis. Journal of Cataract and Refractive Surgery. 2000;26(9):1326–31. doi: 10.1016/s0886-3350(00)00566-6. [DOI] [PubMed] [Google Scholar]
- [22].Battat L, Macri A, Dursun D, Pflugfelder SC. Effects of laser in situ keratomileusis on tear production, clearance, and the ocular surface. Ophthalmology. 2001;108(7):1230–35. doi: 10.1016/s0161-6420(01)00623-6. [DOI] [PubMed] [Google Scholar]
- [23].Savini G, Prabhawasat P, Kojima T, Grueterich M, Espana E, Goto E. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008;2(1):31–55. doi: 10.2147/opth.s1496. [DOI] [PMC free article] [PubMed] [Google Scholar]



![[Table/Fig-1]:](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/cf94/4625269/6ec6af090ed7/jcdr-9-NC06-g001.jpg)