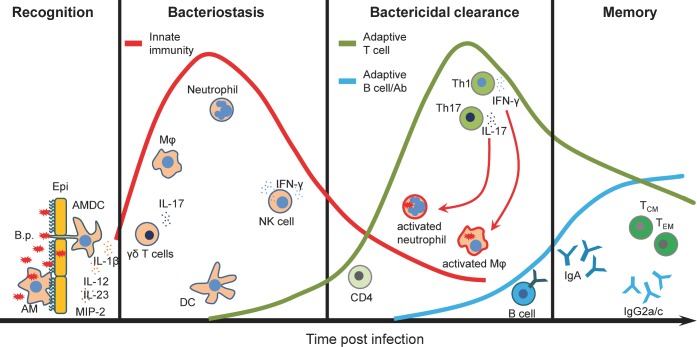
Figure 1.
Relative contribution of the cell subtypes to the induction of immune response to B. pertussis. The immune response to B. pertussis is a complex process that involves activation and recruitment of immune cells to the respiratory tract and generation of long-lasting adaptive immunity. Attachment of B. pertussis to ciliated epithelial cells and recognition by AMDCs and AMs provide a first line of immediate defense against B. pertussis infection. Secretion of cytokines and chemokines promotes recruitment of innate immune cells. Innate IL-17 together with CXCL2 (or MIP-2) secreted by activated macrophages and epithelial cells promote neutrophils recruitment. NK cells play a protective role through the secretion of IFNγ, which enhances the antimicrobial activity of macrophages as well as induces Th1 cells. Activated neutrophils and macrophages participate in an antibody-mediated phagocytosis and intracellular killing of B. pertussis. DCs migrate to the lymph nodes to present the antigen to the naive T cells. Primed T cells proliferate and differentiate into Th1 and Th17 cells that migrate to the lungs to further activate neutrophils and macrophages by production of IFNγ and IL-17, respectively. Activated B cells differentiate into plasma cells that produce B. pertussis-specific IgA or IgG2a/c antibodies (mouse). Finally, a small fraction of T and B cells become memory cells providing an effective protection after reinfection. B.p., Bordetella pertussis; Epi, epithelium; AMs, alveolar macrophages; AMDCs, airway mucosal dendritic cells; DCs, dendritic cells; Mφ, macrophages; Neu, neutrophils; Th, T helper cells; TCM, central memory T cells; TEM, effector memory T cells.