Abstract
Aims/Introduction
We investigated the relationship between the frequency of self-monitoring of blood glucose (SMBG) and glycemic control in type 1 diabetes mellitus patients on continuous subcutaneous insulin infusion (CSII) or on multiple daily injections (MDI) using data management software.
Materials and Methods
We recruited 148 adult type 1 diabetes mellitus patients (CSII n = 42, MDI n = 106) and downloaded their SMBG records to the MEQNET™ SMBG Viewer software (Arkray Inc., Kyoto, Japan). The association between the SMBG frequency and the patients' hemoglobin A1c (HbA1c) levels was analyzed using the χ2-test and linear regression analysis was carried out to clarify their relationship.
Results
The odds ratio of achieving a target HbA1c level of <8% (63.9 mmol/mol) was significantly higher in subjects with SMBG frequencies of ≥3.5 times/day compared with those with SMBG frequencies of <3.5 times/day in the CSII group (odds ratio 7.00, 95% confidence interval 1.72–28.54), but not in the MDI group (odds ratio 1.35, 95% CI 0.62–2.93). A significant correlation between SMBG frequency and the HbA1c level was detected in the CSII group (HbA1c [%] = –0.24 × SMBG frequency [times/day] + 8.60 [HbA1c {mmol/L} = –2.61 × SMBG frequency {times/day} + 70.5], [r = –0.384, P = 0.012]), but not in the MDI group.
Conclusions
A SMBG frequency of <3.5 times per day appeared to be a risk factor for poor glycemic control (HbA1c ≥8%) in type 1 diabetes mellitus patients on CSII.
Keywords: Continuous subcutaneous insulin infusion, Self-monitoring of blood glucose, Type 1 diabetes mellitus
Introduction
The optimal frequency of self-monitoring of blood glucose (SMBG) in patients with type 1 diabetes mellitus is unclear. In Japan, the insurance reimbursements for SMBG allowing ≥120 times per month (approximately ≥4 times a day) for type 1 diabetes mellitus were approved in 2008. The association between the frequency of SMBG and glycemic control in type 1 diabetes mellitus has been examined in several observational studies; however, in most of the previous studies, patients on continuous subcutaneous insulin infusion (CSII) and those on multiple daily injections (MDI) were not separated, and the frequency of SMBG was measured using self-reported questionnaires or based on insurance reimbursement data.1–5 Thus, using data management software, we investigated the relationship between the frequency of SMBG and glycemic control in type 1 diabetes mellitus patients on CSII or on MDI separately.
Materials and Methods
Study Design and Participants
A total of 148 adult type 1 diabetes mellitus patients were recruited from those who regularly visited National Hospital Organization (NHO) Kyoto Medical Center, Kyoto, Japan. The inclusion criterion was patients whose SMBG data were downloaded to the data management software. The exclusion criterion was those who were aged younger than 20 years. Data were collected between July 2012 and June 2013.
Ethics
The study was approved by the ethical committee of NHO Kyoto Medical Center.
Assessment of SMBG Frequency
Each participant was provided with a GLUCOCARD G+ Meter (Arkray Inc., Kyoto, Japan). MEQNET™ SMBG Viewer software (Arkray Inc., Kyoto, Japan) was used as the data management software. The SMBG data were downloaded to the software during hospital visits, and the mean SMBG frequency (times/day) for a 30-day period was calculated from the downloaded data.
Hemoglobin A1c Measurement
The patients' hemoglobin A1c (HbA1c) levels were measured using an ADAMS A1c HA-8180 automatic glycohemoglobin analyzer (Arkray Inc., Kyoto, Japan). The detection range of this device is 3–20% (14–191 mmol/mol).
Statistical Analysis
For continuous variables, Student's t-test was used to compare the means of the two study arms. For categorical variables, the χ2-test was used to compare proportions. Odds ratios (95% confidence intervals [CI]) showing the relative likelihood of the target HbA1c level being achieved were calculated for each SMBG frequency cut-off level using the χ2-test. Cut-off values of 1.5, 2.5, 3.5 and 4.5 times per day were used to classify the SMBG frequency data, which was collected as continuous values. A target HbA1c level of <8% was used as ‘Objective when intensification of therapy considered difficult,’ and a target HbA1c level of <7% was used as ‘Objective when aiming to prevent complications,’ according to the guidelines of the Japan Diabetes Society.6 In the MDI group, subanalysis was carried out after excluding patients with HbA1c >10%. To clarify the relationship between the patients' HbA1c levels and the frequency of SMBG, we carried out linear regression analysis. The correlation between the frequency of SMBG and age, sex, body mass index (BMI) and diabetes duration was tested with Pearson's correlation analysis. The association between achieving HbA1c <7%, and age, sex, BMI, diabetes duration and the SMBG frequency was tested by logistic regression analysis. The Statistical Package for the Social Sciences (SPSS 20.0; IBM Corp., Armonk, NY, USA) program was used for all analyses. Two-tailed P-values of <0.05 were considered significant.
Results
With regard to the patients' backgrounds, those on CSII were significantly younger, lower in HbA1c levels and measured their blood glucose more frequently than those on MDI (Table1). The mean HbA1c level was significantly different at cut-off values of 2.5 times/day and 3.5 times/day in the CSII group, but not in the MDI group (Table2). In the CSII group, the odds ratio of achieving a target HbA1c level of <8% (63.9 mmol/mol) was significantly higher in participants with SMBG frequencies of ≥3.5 times/day compared with those with SMBG frequencies of <3.5 times/day, but not in the MDI group (Table3). When the target HbA1c was set at <7% (53.0 mmol/mol), none of the SMBG frequency cut-off values had significant effects on the likelihood of the target HbA1c level being achieved in the CSII group or in the MDI group. We also tested the odds ratio of achieving the target HbA1c in patients on MDI after excluding 11 patients with HbA1c >10%, and the odds ratio of achieving a target HbA1c level of <8% (63.9 mmol/mol) was significantly higher in patients with SMBG frequencies of ≥1.5 times/day compared with <1.5 times/day (Table4).
Table 1.
Baseline characteristics of study population
| Variables | CSII (n = 42) | MDI (n = 106) | P-value (CSII vs MDI) |
|---|---|---|---|
| Age (years) | 40.1 (12.1) | 51.9 (17.5) | <0.001* |
| Male (%) | 33.3 | 47.2 | 0.144 |
| Body mass index (kg/m2) | 21.9 (2.5) | 21.4 (2.7) | 0.272 |
| Diabetes duration (years) | 12.2 (9.3) | 12.8 (12.1) | 0.792 |
| HbA1c | |||
| % | 7.6 (0.9) | 8.2 (1.6) | 0.020* |
| mmol/mol | 59.9 (10.1) | 66.5 (16.9) | |
| SMBG frequency (times/day) | 4.0 (1.5) | 3.2 (1.3) | 0.002* |
Data are means (standard deviation) or percentage. *P < 0.05.
Table 2.
Association of self-monitoring of blood glucose frequency and hemoglobin A1c levels
| CSII group (n = 42) | MDI group (n = 106) | |||
|---|---|---|---|---|
| SMBG frequency times/day | HbA1c | P-value | HbA1c | P-value |
| % | % | |||
| mmol/mol | mmol/mol | |||
| <4.5 | 7.8 (1.0) | 0.104 | 8.3 (1.6) | 0.108 |
| 61.9 (10.9) | 67.6 (17.3) | |||
| ≥4.5 | 7.3 (0.7) | 7.6 (1.2) | ||
| 56.7 (8.0) | 60.0 (13.2) | |||
| <3.5 | 8.2 (0.9) | 0.001* | 8.4 (1.7) | 0.197 |
| 66.2 (9.9) | 68.3 (18.7) | |||
| ≥3.5 | 7.3 (0.8) | 8.0 (1.3) | ||
| 56.1 (8.2) | 63.9 (13.7) | |||
| <2.5 | 8.5 (0.9) | 0.010* | 8.5 (1.6) | 0.298 |
| 69.5 (9.7) | 69.7 (17.8) | |||
| ≥2.5 | 7.5 (0.9) | 8.2 (1.5) | ||
| 58.3 (9.4) | 65.6 (16.7) | |||
| <1.5 | 8.2 (n = 2) | NA | 8.4 (0.8) | 0.745 |
| 65.6 | 68.0 (8.7) | |||
| ≥1.5 | 7.6 (0.9) | 8.2 (1.6) | ||
| 59.6 (10.3) | 66.3 (17.7) | |||
Data are means (standard deviation). *P < 0.05. CSII, continuous subcutaneous insulin infusion; MDI, multiple daily injections; NA, not available.
Table 3.
Odds ratio of achieving the target hemoglobin A1c in patients on continuous subcutaneous insulin infusion and on multiple daily injections
| SMBG frequency times/day | Target of HbA1c | Odds ratio (95% confidence interval) | P-value | |
|---|---|---|---|---|
| CSII (n = 42) | ≥4.5 | <8% (<63.9 mmol/L) | 3.71 (0.85–16.21) | 0.102 |
| <7% (<53.0 mmol/L) | 1.63 (0.43–6.17) | 0.510 | ||
| ≥3.5 | <8% (<63.9 mmol/L) | 7.00 (1.72–28.54) | 0.008* | |
| <7% (<53.0 mmol/L) | 5.13 (0.96–27.36) | 0.084 | ||
| ≥2.5 | <8% (<63.9 mmol/L) | 4.55 (0.72–28.61) | 0.164 | |
| <7% (<53.0 mmol/L) | NA | NA | ||
| ≥1.5 | <8% (<63.9 mmol/L) | 1.86 (0.11–32.01) | 1.000 | |
| MDI (n = 106) | <7% (<53.0 mmol/L) | NA | NA | |
| ≥4.5 | <8% (<63.9 mmol/L) | 2.33 (0.74–7.37) | 0.170 | |
| <7% (<53.0 mmol/L) | 1.84 (0.52–6.57) | 0.465 | ||
| ≥3.5 | <8% (<63.9 mmol/L) | 1.35 (0.62–2.93) | 0.553 | |
| <7% (<53.0 mmol/L) | 0.83 (0.30–2.30) | 0.800 | ||
| ≥2.5 | <8% (<63.9 mmol/L) | 1.84 (0.72–4.67) | 0.248 | |
| <7% (<53.0 mmol/L) | 1.12 (0.33–3.76) | 1.000 | ||
| ≥1.5 | <8% (<63.9 mmol/L) | 3.27 (0.83–12.83) | 0.124 | |
| <7% (<53.0 mmol/L) | 2.61 (0.32–21.50) | 0.689 |
*P < 0.05. HbA1c, hemoglobin A1c; CSII, continuous subcutaneous insulin infusion; MDI, multiple daily injections; NA, not available (as no patient achieved the target of hemoglobin A1c <7% in patients on continuous subcutaneous insulin infusion with self-monitoring of blood glucose frequency < 2.5 times per day); SMBG, self-monitoring of blood glucose.
Table 4.
Odds ratio of achieving the target hemoglobin A1c in patients on multiple daily injections after excluding patients with hemoglobin A1c >10%
| SMBG frequency times/day | Target of HbA1c | Odds ratio (95% confidence interval) | P-value | |
|---|---|---|---|---|
| MDI (n = 95) | ≥4.5 | <8% (<63.9 mmol/L) | 2.32 (0.67–8.00) | 0.174 |
| <7% (<53.0 mmol/L) | 1.76 (0.49–6.37) | 0.385 | ||
| ≥3.5 | <8% (<63.9 mmol/L) | 1.21 (0.53–2.75) | 0.644 | |
| <7% (<53.0 mmol/L) | 0.76 (0.27–2.14) | 0.603 | ||
| ≥2.5 | <8% (<63.9 mmol/L) | 2.03 (0.79–5.18) | 0.137 | |
| <7% (<53.0 mmol/L) | 0.93 (0.3–2.93) | 0.907 | ||
| ≥1.5 | <8% (<63.9 mmol/L) | 4.33 (1.09–17.24) | 0.027* | |
| <7% (<53.0 mmol/L) | 3.05 (0.37–25.00) | 0.280 |
*P < 0.05. HbA1c, hemoglobin A1c; MDI, multiple daily injections; SMBG, self-monitoring of blood glucose.
The SMBG frequency was correlated with the HbA1c level in the CSII group (HbA1c [%] = −0.24 × SMBG frequency [times/day] + 8.60 [HbA1c {mmol/L} = −2.61 × SMBG frequency {times/day} + 70.5], [r = −0.384, P = 0.012]), but not in the MDI group (HbA1c [%] = [−0.16 × SMBG frequency {times/day}] + 8.75, [HbA1c {mmol/mol} = −1.73 × SMBG frequency {times} + 72.1 mmol/mol], [r = −0.132, P = 0.177]; Figure1a,b).
Figure 1.
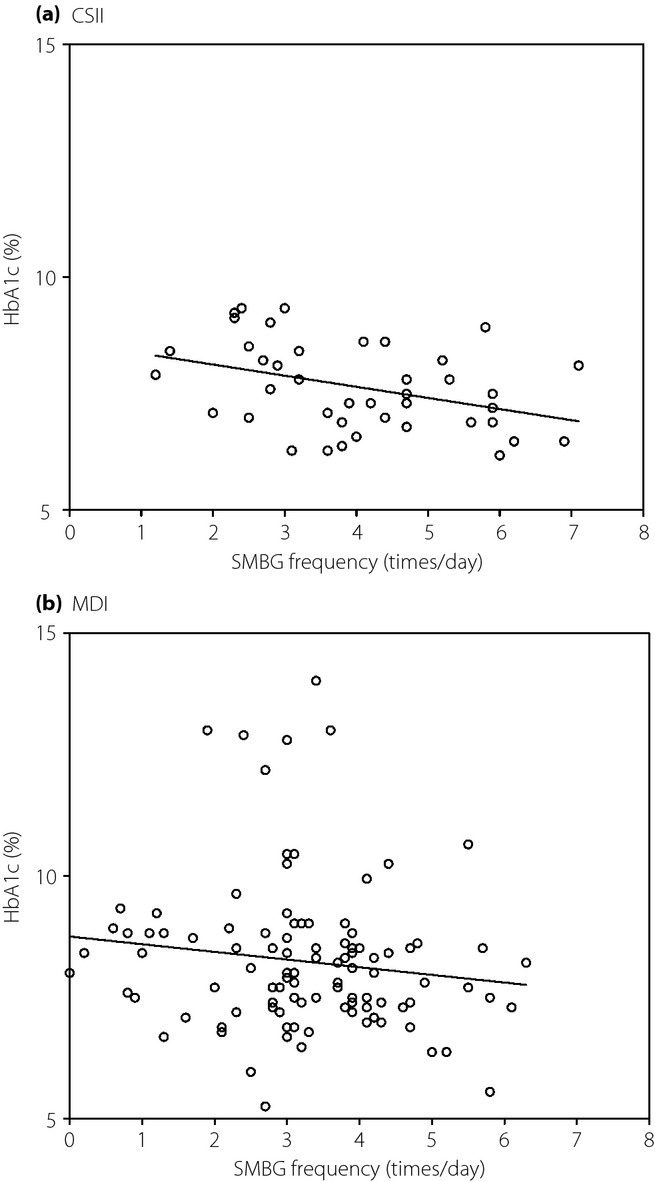
Linear regression analysis of the relationship between the frequency of self-monitoring of blood glucose (SMBG) and the patients' hemoglobin A1c (HbA1c) levels. (a) Continuous subcutaneous insulin infusion (CSII). HbA1c (%) = −0.24 × SMBG frequency (times/day) + 8.60, HbA1c (mmol/L) = −2.61 × SMBG frequency (times/day) + 70.5, r = −0.384, P = 0.012 (<0.05). (b) Multiple daily injections (MDI). HbA1c (%) = −0.16 × SMBG frequency (times/day) + 8.75, HbA1c (mmol/mol) = −1.73 × SMBG frequency (times/day) + 72.1, r = −0.132, P = 0.177. The y-axes of the graphs represent the HbA1c levels (%).
The correlation between the frequency of SMBG, and age, sex, BMI and diabetes duration was examined in both groups, and age was positively correlated with SMBG frequency in the MDI group (Table5). Logistic regression analysis between achieving HbA1c <7%, and age, sex, BMI, diabetes duration and SMBG frequency was carried out (Table6).
Table 5.
Correlation between the self-monitoring of blood glucose frequency and age, sex, body mass index and diabetes duration
| CSII n = 42 | MDI n = 106 | |||
|---|---|---|---|---|
| r | P-value | r | P-value | |
| Age | 0.23 | 0.151 | 0.24 | 0.014* |
| Sex (male) | –0.04 | 0.819 | 0.10 | 0.306 |
| BMI | –0.18 | 0.263 | –0.10 | 0.315 |
| Diabetes duration | 0.28 | 0.069 | 0.02 | 0.825 |
*P < 0.05. BMI, body mass index; CSII, continuous subcutaneous insulin infusion; MDI, multiple daily injections.
Table 6.
Logistic regression analysis between achieving hemoglobin A1c <7% and age, sex, body mass index, diabetes duration and the self-monitoring of blood glucose frequency
| CSII | MDI | |||
|---|---|---|---|---|
| Odds ratio (95% confidence interval) | P-value | Odds ratio (95% confidence interval) | P-value | |
| Age | 0.86 (0.76–0.98) | 0.024* | 0.97 (0.93–1.00) | 0.069 |
| Sex (male) | 1.94 (0.31–12.21) | 0.482 | 2.24 (0.72–6.99) | 0.165 |
| BMI | 1.03 (0.73–1.45) | 0.869 | 0.92 (0.73–1.16) | 0.486 |
| Diabetes duration | 1.05 (0.96–1.15) | 0.292 | 0.97 (0.92–1.03) | 0.374 |
| SMBG frequency | 2.19 (1.10–4.37) | 0.027* | 1.33 (0.86–2.05) | 0.196 |
*P < 0.05. CSII, continuous subcutaneous insulin infusion; MDI, multiple daily injections; SMBG, self-monitoring of blood glucose.
Discussion
In the present study, data management software was used to assess the actual SMBG frequency of type 1 diabetes mellitus patients on CSII or on MDI.
For those on CSII, the cut-off values of 2.5 times/day and 3.5 times/day were associated with significant difference in the mean HbA1c, but not at 4.5 times/day. There is a possibility that the present study was not powered enough for the latter cut-off value. No cut-off value was associated with significant difference in the mean HbA1c for those on MDI.
In the CSII group, those with SMBG frequencies of <3.5 times per day were more likely to fail to achieve a target HbA1c level of <8% (63.9 mmol/mol), suggesting that a SMBG frequency of <3.5 times per day is a risk factor for poor glycemic control in pump users. At the same time, the optimal SMBG frequency for achieving a HbA1c level of <7% (53.0 mmol/mol) among pump users was not elucidated. Conversely, for patients on MDI, none of the examined SMBG frequency thresholds were found to be associated with glycemic control. After excluding the patients with HbA1c >10%, those with SMBG frequencies of <1.5 times per day were more likely to fail to achieve a target HbA1c level of <8% (63.9 mmol/mol) in the MDI group. One hypothesis for the potential heterogeneity in the HbA1c levels in the MDI group is that patients who have a severe problem in diabetes self-management with low adherence were not prescribed insulin pump because of the safety concern. The traditional SMBG frequency of four times per day for type 1 diabetes mellitus, which was used in the Diabetes Control and Complications Trial, appears to be necessary to avoid poor glycemic control for the CSII group in the present study.7 Whether this applies to the MDI group in this study remains inconclusive.
A negative correlation between the frequency of SMBG and the patients' HbA1c levels was observed in the CSII group, but not in the MDI group. In the MDI group, age was positively correlated to SMBG frequency, but not in the CSII group. In the CSII group, the younger patients were more likely to achieve a HbA1c level of <7% (53.0 mmol/mol), but not in the MDI group. The reasons why the SMBG frequency was not correlated with the HbA1c level in the MDI group remain unclear. One possibility is that the negative correlation between SMBG frequency and the HbA1c level in the MDI group was weaker than that in the CSII group, and the current study was not powered enough. The other possibility is that the type 1 diabetes mellitus patients on MDI in Japan might not be familiar with the patient-driven dose adjustment, because of the issues related to diabetes self-management education. For example, carbohydrate counting is relatively new in Japan, and the first textbook written in Japanese was published in 2006. The treatment choice between CSII and MDI in the present study was basically similar to the Diabetes Control and Complications Trial, that is, either by the patient's preference or by the need to change the insulin delivery method. Patient's autonomy was the key factor to the treatment choice between CSII and MDI. Nevertheless, the present findings do not exclude the possibility that the relationship between SMBG frequency and HbA1c levels in type 1 diabetes mellitus patients might differ between patients on CSII and those on MDI. The mechanisms responsible for such differences remain unclear and need to be addressed in future studies. One possibility is that it might be easier to adjust the insulin dosage according to the results of SMBG using insulin pumps than conventional insulin pens or syringes, because of the difference in the flexibility of insulin delivery. Another possibility is that the role of SMBG in the MDI group might rely more on the lifestyle modification than insulin dose adjustment.
It is worth noting that SMBG is important in patients on CSII for reasons other than glycemic control. For example, as only rapid-acting insulin analogs that decay within 4–6 h are used in CSII, regular measurements of blood glucose levels ≥4 times/day are essential to ensure the safety of CSII, so that any failure in the insulin pump system is detected as soon as possible.
The strengths of the present study include the use of downloaded SMBG data, and separate analyses of patients in the CSII group and in the MDI group. The limitations of this study include its relatively small sample size, the fact that it was a single-centered cross-sectional study, and lacking information about insulin dosage, frequency of hypoglycemia, hypoglycemia severity, kidney function, complication status, socioeconomic status and quality of life.
Considering the fact that glucose measurements are carried out depending on the clinical needs of individual patients, it would be ethically difficult to carry out a randomized controlled trial in which the study participants were allocated to different fixed SMBG frequencies for a certain period. A larger multicenter prospective cohort study might be a reasonable alternative approach to investigating the optimal SMBG frequencies for patients with type 1 diabetes mellitus on CSII or on MDI.
Acknowledgments
The authors thank all of their colleagues who were involved in caring for the type 1 diabetes mellitus patients at the Diabetes Center and the Division of Preventive Medicine, Clinical Research Institute, NHO Kyoto Medical Center.
Disclosure
The present study was supported by a Grant-in-Aid from NHO. TM received a lecture fee, and NS received a lecture fee and a research grant from Arkray Inc., Kyoto, Japan. The other authors declare no conflict of interest.
References
- Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med. 2001;111:1–9. doi: 10.1016/s0002-9343(01)00742-2. [DOI] [PubMed] [Google Scholar]
- Schütt M, Kern W, Krause U, et al. Is the frequency of self-monitoring of blood glucose related to long-term metabolic control? Multicenter analysis including 24,500 patients from 191 centers in Germany and Austria. Exp Clin Endocrinol Diabetes. 2006;114:384–388. doi: 10.1055/s-2006-924152. [DOI] [PubMed] [Google Scholar]
- Ziegler R, Heidtmann B, Hilgard D, et al. Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2011;12:11–17. doi: 10.1111/j.1399-5448.2010.00650.x. [DOI] [PubMed] [Google Scholar]
- Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36:2009–2014. doi: 10.2337/dc12-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minder AE, Albrecht D, Schäfer J, et al. Frequency of blood glucose testing in well educated patients with diabetes mellitus type 1: how often is enough? Diabetes Res Clin Pract. 2013;101:57–61. doi: 10.1016/j.diabres.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 2012. Treatment guide for diabetes 2012–2013 edited by Japan diabetes society [article online] http://www.jds.or.jp/modules/en/index.php?content_id=1 (last accessed on March 20, 2015)
- The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]


