Abstract
Objectives:
To evaluate the impact of CBCT imaging when placing dental implants in the anterior edentulous mandible, using a “before–after” study design.
Methods:
Eight dental practitioners, who regularly place dental implants in independent dental practice in the North West of England, were presented with realistic simulations of four edentulous cases. The practitioners were asked to assess case difficulty, select implants and then drill osteotomies in preparation for dental implants in the lower canine regions to support a complete overdenture. In the “before” part of the study, a panoramic and a trans-symphyseal view were available. In the “after” part of the study, a CBCT image was added. Perception of case difficulty, implant selection and the incidence of perforations or “near miss perforations” of the lingual cortical plate were recorded. Two cases were regarded as “regular” and two as “challenging”.
Results:
In challenging cases, the availability of CBCT led practitioners to select narrower implants and to assess cases as more difficult. In the challenging cases only, there were fewer perforations of the lingual cortical plate after the availability of CBCT, but this difference was not statistically significant. There were no perforations in the regular cases either before or after the availability of CBCT.
Conclusions:
Perception of case difficulty and implant selection are of importance only if they change the outcome for the patient. This study provided weak evidence that CBCT is helpful in avoiding perforations in challenging cases. The availability of CBCT had no impact in regular cases.
Keywords: patient simulation, dental implants, radiography, dental cone beam computed tomography
Introduction
The McGill consensus of 20021 and the York consensus of 20092 both reviewed the place of two implant mandibular overdentures in the treatment of edentulism. The McGill group concluded that “there is now overwhelming evidence that a two implant overdenture should become the first choice of treatment for the edentulous mandible.”1 Similarly, the York group commented that “a two implant supported mandibular overdenture should be the minimum offered to edentulous patients as a first choice of treatment.”2 Whilst the placement of dental implants in the anterior edentulous mandible has been recommended as a safe procedure, perhaps suitable for novices to implant surgery, there is a risk of perforation of the lingual surface. Perforation has the potential to traumatize lingual vessels causing severe bleeding and a life-threatening upper airway obstruction.3−21
An appreciation of the form of the anterior mandible is required to avoid perforation. CBCT can be used with specialist planning software to give pre-operative, cross-sectional images. It has been suggested that such imaging is advisable, or should be routine, to reduce the likelihood of such an event.4,22,23 Nonetheless, a pre-operative appreciation of the form of the anterior mandible may also be gained through conventional radiography, such as panoramic, lateral cephalometric or trans-symphyseal views.24,25
Fryback and Thornbury26 proposed six levels of evaluation of diagnostic imaging: technical efficacy, diagnostic accuracy efficacy, diagnostic thinking efficacy, therapeutic efficacy, patient outcome efficacy and societal efficacy. Whilst many studies have been conducted to investigate technical and diagnostic accuracy efficacy of CBCT, few studies address the higher levels and none addresses patient outcome when placing dental implants.27
The majority of dental implant placements in the UK are carried out in the independent practice environment.28 Nevertheless, research is almost exclusively conducted in university schools of dentistry with hospital-based dentists.27 It appears, therefore, that such research is most often being conducted with those who do not represent the majority of implant-placing dentists.
A preliminary aim of this study was to develop a life-like dental simulation, which provides drillable models of edentulous mandibles and that could be used to obtain a range of corresponding radiological images. The primary aim of this study was to evaluate the impact of CBCT imaging on the incidence of perforation of the lingual cortical plate when placing dental implants in the anterior edentulous mandible, using a “before–after” study design. Secondary research objectives addressed the impact of CBCT on the pre-operative assessment of case difficulty and choice of dental implant. This research was carried out amongst implant practitioners in independent dental practice in the North West of England.
Methods and materials
Ethical approval for this study was granted by the University of Leeds, Leeds, UK, Dental Research Ethics Committee.
Development of a dental simulation phantom
The simulation consisted of four components. The first of these was a suitably shaped water bath to be used to contain edentulous mandible specimens and mimic the attenuation of X-rays that occurs in clinical imaging. Secondly, a material was developed that reproduced the look, radio-opacity and feel of bone when drilling and was used to make casts of the mandible specimens. Thirdly, the oral surface of the mandible models was covered in a material that simulated the alveolar ridge mucosa. Finally, a phantom head was used into which the mandibular models could be fixed for simulated implant surgery.
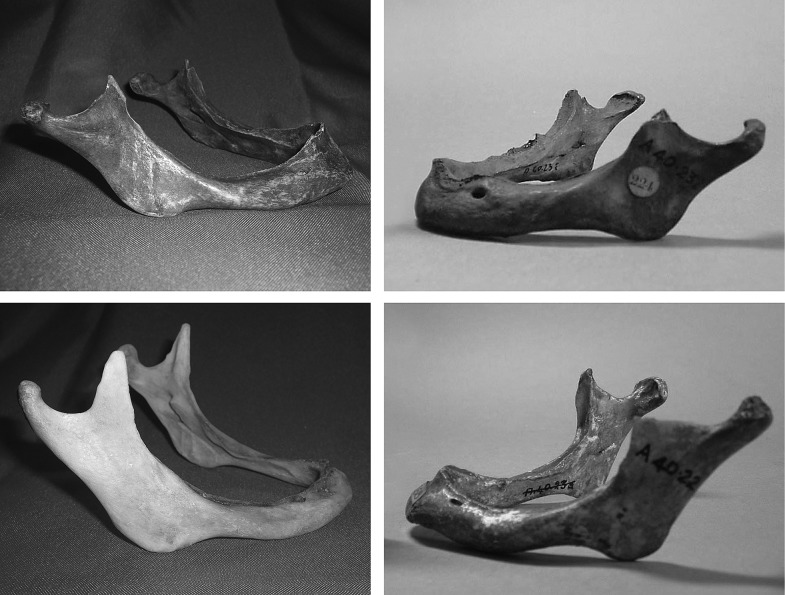
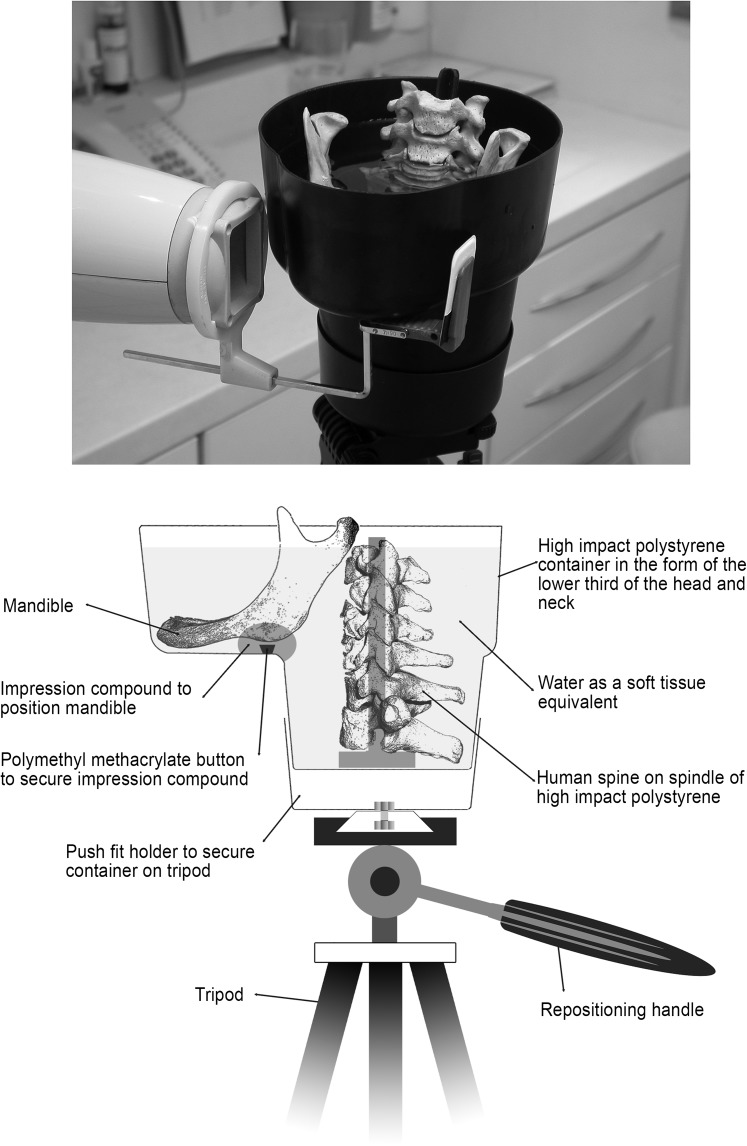
Four edentulous mandible specimens were acquired from historical collections, representing a range of difficulty of implant placement (Figure 1). For the purpose of radiological imaging, the mandibles were positioned in a radiographic phantom in the form of the lower third of the head and the neck and containing water as a soft-tissue equivalent, as previously described by Shelley et al29 in 2011 (Figure 2). The phantom allows part of a human cervical spine and a mandible to be positioned within it and is supported by a tripod system.
Figure 1.
The four edentulous mandibles selected for reproduction in the dental simulation.
Figure 2.
The anatomical water phantom used for acquisition of the images.
The material used for the mandibular model consisted of a mixture of barium sulphate (APC Pure, Manchester, UK), sodium bicarbonate (Tesco Stores Ltd, Cheshunt, UK) and water added to polyurethane casting resin (SG2000 Fast Cast Polyurethane Resin System; MB Fibreglass, Newtownabbey, UK). The proportions by weight were polyurethane resin, 64%; barium sulphate, 32%; water, 3.2%; and sodium bicarbonate, 0.8%. Impressions were taken of the full volume of the anterior part of the mandible specimens using a clinical, addition-cured, silicone putty impression material (Provil® novo Putty fast set; Heraeus Kulzer GmbH, Hanau, Germany). Duplicates of the mandible specimens were cast from these impressions using the barium sulphate and resin material. Figure 3 is a section through one of the mandible models, showing the bone-like texture achieved.
Figure 3.

Sectioned cast of a mandible in the bone analogue material.
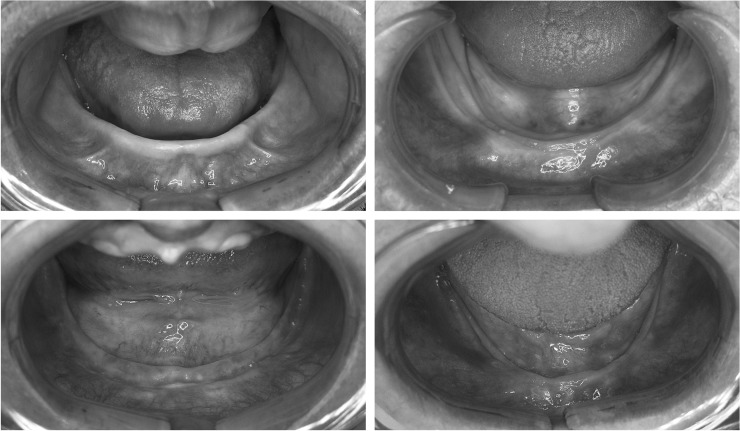
Four edentulous patients from the first author's dental practice were recruited, and with their consent, clinical reference photographs of lower edentulous ridges were taken that represented a plausible match to the four dried edentulous mandible specimens (Figures 1 and 4). These photographs were used as references to create wax master models representing soft tissue overlying the duplicate mandibles, crafted by hand in modelling wax (Kemdent Anutex Eco Modelling Wax; Associated Dental Products Ltd, Swindon, UK). An example is shown in Figure 4. Three implant dentists, all on the UK's specialist list for oral surgery with considerable experience of dental implant placement, were asked to recreate the exposure of bone produced by raising surgical flaps in the wax models. They were told that the case had been planned to receive dental implants in the lower canine regions and asked to reveal the bone to the same extent that they would do in the clinical situation. In addition, four textbooks of surgical implantology were consulted.24,30–32 The results of the surgical flap exercise, together with the advice in the textbooks, were used to make a judgment on a typical flap for each of the cases. Final wax master models were made, one for each of the four mandibles, with the bone exposed as suggested by this preliminary study.
Figure 4.
Clinical reference photographs of edentulous ridges.
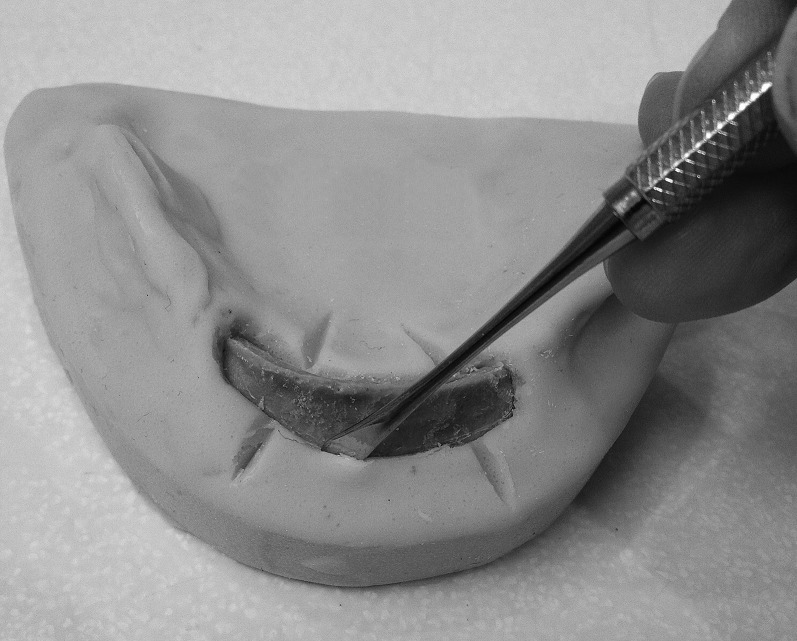
Each master wax model was invested in commercially available, synthetic die stone (Skillstone Gold+; Skillbond Direct Ltd., High Wycombe, UK). Silicone rubber (Smooth-Sil® 940 platinum cure silicone rubber; Smooth-On Inc., Pennsylvania, PA) with a shore hardness of 40, which was, subjectively, similar to soft tissue and that was also found to be largely radiolucent, was then poured around the duplicate mandibles. Figure 5 shows a final drillable model and illustrates how the soft-tissue analogue material can be separated from the duplicate mandible with a periosteal elevator in a similar way to clinical surgery.
Figure 5.
Final drillable model, with a periosteal elevator being used to raise the soft-tissue silicone substitute material.
For the purpose of conducting implant surgery on the models in a way that mimicked the clinical situation, a commercially available phantom head (Nissin Dental Simulation System, Simple Manikin II; Nissin Dental Products Inc., Kyoto, Japan) was acquired into which the mandible models could be fixed. A model of an edentulous upper ridge was also placed to reproduce the clinical situation more effectively. The phantom head could be secured to a dental chair head rest by means of Velcro® straps (Velcro Ltd, Middlewich, UK) and could be posed in a comfortable position for operators by means of universal joints.
Trial of the dental simulation phantom
A panoramic radiograph, a trans-symphyseal radiograph25,33 and CBCT images were obtained for each of the mandible specimens. Digital panoramic images were acquired using a SOREDEX® CRANEX® 3 Ceph (Soredex, Tuusula, Finland) operated at 64 kV, 4 mA for 11.0 s. Conventional trans-symphyseal images were acquired using a Trophy Atlantis™ Intraoral X-ray system (Trophy Radiologie, Marne-la-Vallée, France) operated at 60 kV, 7 mA, 0.74 s on AGFA Dentus® M2 film E/F speed size 2 (Agfa-Gevaert NV, Mortsel, Belgium) and processed in a Durr Periomat Plus® automatic film processor (Dürr Dental AG, Bietigheim-Bissingen, Germany). CBCT images were acquired using an 3D Accuitomo 170 (J Morita Manufacturing Corporation, Kyoto, Japan) operated at 90 kV, 4.0 mA for 17.5 s.
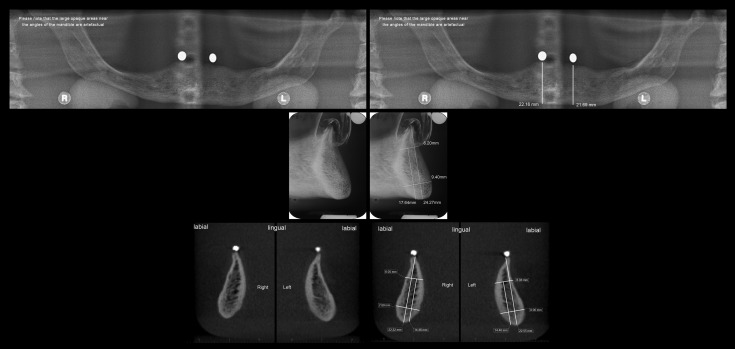
Two dentists, both experienced implant surgeons working in primary dental care, were presented with the complete dental simulation, with four drillable models and a set of radiographic images for each. For two of the cases, the participants were presented with the panoramic and trans-symphyseal images only. For the other cases, they were presented with the panoramic, trans-symphyseal and CBCT images. They also had available an implant motor and a set of implant surgery instruments. The trans-symphyseal images were available on both conventional film and as digitized images. For these images, a manufacturer's transparency was available so that direct measurements could be made. The digital images were available with pre-made measurements and, for clarity, without them. The implant dentists could also fully explore the CBCT images and take their own measurements using the proprietary software “One Volume Viewer” (J Morita Manufacturing Corporation). A full set of images for one of the mandibles is presented in Figure 6.
Figure 6.
A full set of images, for one of the four mandibles, presented to participants. Top row—panoramic radiographs without and with measurements; middle row—trans-symphyseal view without and with measurements; bottom row—CBCT cross-sectional images at the sites of implant placement without and with measurements. L, left; R, right.
The two implant dentists were asked to consider the available images and then prepare osteotomies for implant placements in the lower canine regions, selecting implants and drilling the osteotomies for the Neoss Dental Implant System (Neoss Ltd, Harrogate, UK). They were then asked to complete an evaluation survey. The dentists were asked the following three questions: “Do you think that the presentation of the case and the artefacts is a reasonable reproduction of clinical circumstances and would you suggest any improvements?”, “Is the method of presentation of the images sensible and would you suggest any improvements?”, “Do you have any general comments about the way the study has been conducted or any suggestions to improve the process from the participant's point of view?”.
At the completion of this trial, the practitioners agreed that the dental simulation was a realistic reproduction of clinical circumstances and did not offer any suggestions for improvements. One found it helpful to have the CBCT viewing software available so that the surgical site could be explored, although the other dentist felt that pre-prepared sections provided sufficient information. One panel member completed the exercise in 40 min and the other in 60 min, including time for setting up the materials.
Implementation of the before–after study
Eight participants, all implant practitioners in the North West of England, were recruited to the study. An attempt was made to choose practitioners with demographic characteristics that represented those of the region as a whole.34 A sample size calculation suggested a sample size of 33 matched pairs of data (α = 0.05 1−β = 0.8). It was anticipated that 8 participants would generate 64 matched pairs of data. Therefore, this was considered to be within a reasonable margin of error with regard to sample size.
For each mandible specimen, two conventional images were taken, a panoramic and a trans-symphyseal view.25 These were assigned to the “before” part of the study. A CBCT image data set was acquired. This, along with the conventional images, was assigned to the “after” part of the study. For the digital images, a preliminary study had suggested typical measurements that might be useful in planning implant placement, and these were pre-marked on those images. The full set of images, with exposure factors and mode of presentation, are listed in Table 1.
Table 1.
Images available with exposure factors and mode of presentation
| Image | Exposure factors | Presentation |
|---|---|---|
| CBCT image (presented in after part of the study only) | 3D Accuitomo; voltage, 90 kV; current, 4.0 mA; time, 17.5 s | Displayed on Sony® Vaio PCG-71911M laptop computer. Pre-prepared sections at the sites of the proposed implants were prepared with and without pre-made measurements. “One Volume Viewer” viewing software available to explore images |
| Panoramic view (presented in both before and after parts of the study) | SOREDEX® CRANEX® 3 Ceph; voltage, 64 kV; current, 4.0 mA; time, 11 s | Digital image displayed on Sony Vaio PCG-71911M laptop computer with and without pre-made measurements |
| Trans-symphyseal view (presented in both before and after parts of the study) | Trophy Atlantis™; focus/film distance, 20 cm; voltage, 60 kV; current, 7 mA; time, 0.739 s Film AGFA Dentus® M2; E/F speed, size 2 Durr Periomat Plus® automatic film processor |
Conventional film displayed on a light box. Manufacturer's transparencies available to take measurements directly from film. Images were also digitized at 300 dpm on a CanoScan 8800F digital scanner and displayed on Sony Vaio PCG-71911M laptop computer with and without pre-made measurements |
One Volume Viewer and 3D Accuitomo was obtained from J Morita Manufacturing Corporation, Kyoto, Japan; Trophy Atlantis from Trophy Radiologie, Marne-la-Vallée, France; AGFA Dentus from Agfa-Gevaert NV Mortsel, Belgium; Durr Periomat Plus automatic film processor from Dürr Dental AG, Bietigheim-Bissingen, Germany; CanoScan 8800F from Canon Inc., Tokyo, Japan; SOREDEX CRANEX 3 Ceph from Soredex, Tuusula, Finland; Sony Vaio PCG-71911M from Sony Corporation, Tokyo, Japan.
For each of the four cases, a fictional case history and a photograph were provided. The photographs of real patients were selected as a plausible match to the four mandibles. The four case histories were very similar and deliberately bland so that there was no medical history or other factors that might dictate the treatment plan or affect the drilling of osteotomies. They were also written to be unmemorable so that they were unlikely to be recognized when presented for a second time. In a preliminary study, a panel of four dentists had ordered the cases by anticipated surgical difficulty. They were all experienced implant dentists and were not included in the eight who took part in the main study. Following this, two cases were assigned as being “regular” and two as “challenging”.
The eight participants were visited at their practices on two occasions, 4 weeks apart. The intention was that the participants would not remember the details of the cases and so not recognize that the same cases were being presented with different images. For each visit, the cases were randomized to be either a “before” or an “after” case. The cases were disguised by having different identification numbers in the before and after parts of the study. In all other respects, the cases were identical. At the second visit, the participants were told that there were four new cases. They were, therefore, blinded to the fact that the same cases were presented at the second visit but with different images available. At each visit, the participants were provided with the materials listed in Table 2.
Table 2.
Items available for participants at each visit
| Items available | Details |
|---|---|
| A set of implant surgery instruments | |
| Dental implant motor with handpieces | |
| Full set of digital images | Panoramic view Digitized trans-symphyseal view CBCT images with viewing software (after part of the study only) |
| Conventional radiographs | Trans-symphyseal view |
| X-ray viewer | Light box to view conventional trans-symphyseal radiographs |
| Manufacturer's transparencies | For assessment of conventional trans-symphyseal radiographs |
| Dental simulation | The same four cases at each visit presented in a phantom head |
| Information sheets | Reminder sheet for implant drill markings Drilling guide—straight implants Drilling guide—tapered implants Copy of the anonymization and confidentiality policy Information sheet for the first or second visit |
| Recording sheets | Case histories with data recording form |
Each case history was presented with a questionnaire. The participants were asked to score case difficulty on a ten-point scale based on the history, photographs and available images. The ten-point scale ranged from 1, representing very easy, to 10, representing very difficult. The participants were offered a selection of dental implants (Neoss Ltd) and asked to choose from these for each site. The implant selection included tapered or straight design, lengths from 7 to 15 mm and widths from 3.25 to 5.50 mm. It was recognized that some operators might change their pre-operative selection of implant as a result of their findings when drilling osteotomies.35 Therefore, a second choice was available if the participants' final selection was different from their pre-operative selection. They were then asked to use the implant surgery equipment and instruments listed in Table 2 to prepare osteotomies for two dental implants in the canine regions of the dental simulations. Lastly, the participants were asked to record their final choice of dental implant.
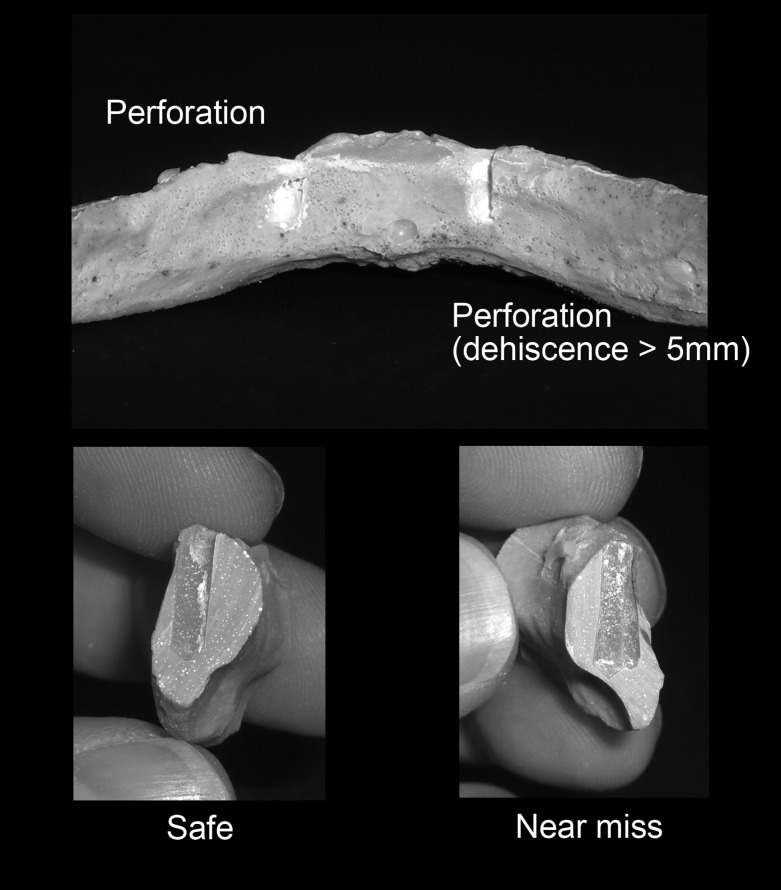
Following completion of all of the practical exercises by the participants, the duplicate mandibles were stripped from the silicone soft-tissue analogue and explored for perforations or near misses. Where there were no perforations, the mandibles were sectioned at the sites of the osteotomies and examined for near misses. A blunt-ended probe with a linear scale was used to assist in measurement, and each osteotomy was classified as “perforation”, “near miss” or “safe” as shown in Table 3.
Table 3.
Classification of the outcome of osteotomy preparation
| Outcome | Definition | Example |
|---|---|---|
| Perforation | A discrete defect of the lingual surface or a dehiscence of the lingual surface >5 mm from the level of the crest of the ridge. A dehiscence was defined as a vertical defect, with no superior border, in the superior/inferior dimension |
 
|
| Near miss | An osteotomy that was closer than 1 mm from the lingual surface of the duplicate mandible |  |
| Safe | An osteotomy that was no closer than 1 mm from the lingual surface of the duplicate mandible. Perforations or dehiscences through the labial surface were recorded as safe |
|
Statistical analysis
Data were inputted into SPSS® statistics 19 (SPSS Inc., Chicago, IL). McNemar's test was used to test the null hypothesis that there was no difference in the proportion of perforations or “near miss perforations” before or after the availability of CBCT. The Wilcoxon signed-rank test was used to test the null hypothesis that there was no significant change in the pre-operative selection of implant dimensions after the availability of CBCT. A paired sample t-test was used to test the null hypothesis that there was no difference in the mean pre-operative assessment of difficulty of implant placement before and after the availability of CBCT. In all cases, statistical significance (α) was set at p = 0.05.
Results
Perforations and near miss perforations
Examples of osteotomies are shown in Figure 7. The results, including both perforations and near misses for all cases, are presented in Table 4. There was no significant difference in the proportions of perforations or “near miss perforations” before or after the availability of CBCT when all cases were considered together (p = 0.21). A similar lack of significant difference was seen when considering perforations only (p = 0.18). The results were then separated into those for the regular cases and those for the challenging cases. These are presented in Tables 5 and 6. There was only one near miss for the regular cases and no perforations. Therefore, no separate analysis was carried out for these results. There was no significant difference in the proportion of perforations or near miss perforations before or after the availability of CBCT when considering the challenging cases alone (p = 0.302). Similarly, there was no significant difference in the proportion of perforations alone, before or after the availability of CBCT when considering the challenging cases (p = 0.18).
Figure 7.
Examples of perforations, a near miss and safe osteotomies.
Table 4.
Perforations and near misses before and after the availability of CBCT for all cases
| Outcome | Number | % |
|---|---|---|
| Before | ||
| Perforations | 11 | 17.2 |
| Near misses | 7 | 10.9 |
| Safe | 46 | 71.9 |
| Total sites | 64 | 100.0 |
| After | ||
| Perforations | 6 | 9.4 |
| Near misses | 6 | 9.4 |
| Safe | 52 | 81.2 |
| Total sites | 64 | 100.0 |
Table 5.
Perforations and near misses before and after the availability of CBCT for regular cases
| Outcome | Number | % |
|---|---|---|
| All dentists—before | ||
| Perforations | 0 | 0.0 |
| Near misses | 1 | 3.1 |
| Safe | 31 | 96.9 |
| Total sites | 32 | 100.0 |
| All dentists—after | ||
| Perforations | 0 | 0.0 |
| Near misses | 0 | 0.0 |
| Safe | 32 | 100.0 |
| Total sites | 32 | 100.0 |
Table 6.
Perforations and near misses before and after the availability of CBCT for challenging cases
| Outcome | Number | % |
|---|---|---|
| Before | ||
| Perforations | 11 | 34.4 |
| Near misses | 6 | 18.7 |
| Safe | 15 | 46.9 |
| Total sites | 32 | 100.0 |
| After | ||
| Perforations | 6 | 18.7 |
| Near misses | 6 | 18.7 |
| Safe | 20 | 62.5 |
| Total sites | 32 | 100.0 |
Implant selection
In the case of selection of implant length, the number of times a longer implant was selected, after the availability of CBCT, was always approximately equal to the number of times a shorter implant was selected. Similarly, in terms of implant design, the number of times that a change from straight to tapered design was made, after the availability of CBCT, was always approximately equal to the number of times that a change was made from tapered to straight. Therefore, no further analysis was carried out for these results. Larger differences were noted for the selection of implant width, and these were subject to statistical analysis. The results for the pre-operative and final selection of implant width are shown in Tables 7 and 8. There was no significant change in the pre-operative selection of implant width after the availability of CBCT when considering all cases (p = 0.053; Z = −1.931). When considering challenging cases alone, however, there was a significant difference, with narrower implants being selected more frequently (p = 0.007; Z = −2.696). The same pattern was observed when looking at the final selection of implant width after the availability of CBCT. There was no significant difference seen when considering all cases (p = 0.131; Z = −1.512), but narrower implants were more frequently used for the challenging cases (p = 0.021; Z = −2.309)
Table 7.
Changes in pre-operative selection of implant width after the availability of CBCT: all four cases, two regular cases and two challenging cases
| Cases | Changes after availability of CBCT |
|||
|---|---|---|---|---|
| Number of decisions | Total number of changes | Number of times wider implant selected | Number of times narrower implant selected | |
| All four cases | 64 | 28 | 8 | 20 |
| Two regular cases | 32 | 14 | 6 | 8 |
| Two challenging cases | 32 | 14 | 2 | 12 |
Table 8.
Changes in final selection of implant width after the availability of CBCT: all four cases, two regular cases and two challenging cases
| Cases | Changes after availability of CBCT |
|||
|---|---|---|---|---|
| Number of decisions | Total number of changes | Number of times wider implant selected | Number of times narrower implant selected | |
| All four cases | 64 | 28 | 10 | 18 |
| Two regular cases | 32 | 16 | 8 | 8 |
| Two challenging cases | 32 | 12 | 2 | 10 |
Pre-operative assessment of case difficulty
The results for the pre-operative assessment of case difficulty before and after the availability of CBCT are shown in Table 9. There was no significant difference in the mean pre-operative assessment of difficulty of implant placement before and after the availability of CBCT for all cases (p = 0.062; t = −1.939). When the challenging cases were considered alone, however, there was a significant increase in the level of difficulty selected by the participating dentists (p = 0.006; t = −3.174). A summary of these statistical analyses is presented in Table 10.
Table 9.
Mean case difficulty scores before and after availability of CBCT
| Mean difficulty scores |
||||||
|---|---|---|---|---|---|---|
| Before availability of CBCT |
After availability of CBCT |
Difference between means | SD of difference between means | |||
| Mean | SD | Mean | SD | |||
| Regular cases | 7.00 | 1.83 | 7.00 | 1.51 | 0.00 | 1.41 |
| Challenging cases | 7.69 | 1.74 | 8.63 | 1.45 | 0.94 | 0.30 |
| All cases | 7.34 | 1.79 | 7.81 | 1.67 | 0.47 | 1.37 |
SD, standard deviation.
Table 10.
Summary of statistical analyses
| Analysis | Statistical test | p-value |
|---|---|---|
|
Perforations and near miss perforations before and after | ||
| Perforations and near misses all cases | McNemar test | p = 0.21 |
| Perforations only all cases | McNemar test | p = 0.18 |
| Perforations and near misses challenging cases alone | McNemar test | p = 0.302 |
| Perforations only challenging cases alone | McNemar test | p = 0.18 |
|
Implant selection before and after | ||
| Decrease in implant width selected. Pre-operative selection all cases | Wilcoxon signed-rank test | p = 0.053 |
| Decrease in implant width selected. Pre-operative selection challenging cases | Wilcoxon signed-rank test | p = 0.007 |
| Decrease in implant width selected. Final selection all cases | Wilcoxon signed-rank test | p = 0.131 |
| Decrease in implant width selected. Final selection challenging cases | Wilcoxon signed-rank test | p = 0.021 |
|
Pre-operative assessment of case difficulty before and after | ||
| Mean pre-operative assessment of case difficulty all cases | Paired sample t-test | p = 0.062 |
| Mean pre-operative assessment of case difficulty challenging cases | Paired sample t-test | p = 0.006 |
Discussion
When considering all cases, the results showed that there were fewer perforations and near misses after the availability of CBCT. Nevertheless, analysis favours acceptance of the null hypothesis that there is no significant difference in the proportion of lingual perforations or near miss perforations before or after the availability of CBCT images. It was noted that there were no incidences of perforations in the two regular cases and only a single near miss. All perforations, and all but one near miss, were performed on the challenging cases. Nevertheless, the evidence was weak that the availability of CBCT had an effect on the incidence of perforation or near miss perforation.
The American Academy of Oral and Maxillofacial Radiology (AAOMR) published their most recent guidelines in 2012. These guidelines state that “AAOMR recommends that cross-sectional imaging be used for the assessment of all dental implant sites and that CBCT is the imaging method of choice for gaining this information”.36 In the same year, however, the European Association of Osseointegration (EAO) published their guidelines, “E.A.O. guidelines for the use of diagnostic imaging in implant dentistry”. These take an alternative position to those of the AAOMR and state that, “If the clinical assessment of implant sites indicates that there is sufficient bone width and the conventional radiographic examination reveals the relevant anatomical boundaries and adequate bone height and space, no additional imaging is required for implant placement.”37 Other guidelines take a similar position to that of the EAO. For example, “Selection Criteria in Dental Radiography” is published by the Faculty of General Dental Practice (GDP) (UK). The latest guidelines were published in 2013 and state that in the case of the anterior edentulous mandible, CBCT examination is recommended in cases of severe resorption or clinical doubt on the shape of the alveolar ridge.33
The results of this study do not support the position of the AAOMR. Taking into account all cases, there was no statistically significant difference in perforations or near misses after the availability of CBCT. If regular cases are looked at in isolation, there were no perforations either with or without the availability of CBCT. This weakens the position of those who advocate that CBCT should be used for all implant sites. If the challenging cases are looked at in isolation, however, there were fewer perforations after the availability of CBCT. This might be thought to support the position of the EAO, FGDP (UK) and others that CBCT may be advisable in demanding cases. Nonetheless, the difference in perforations before and after the availability of CBCT was not statistically significant, and it must be acknowledged that this was likely to have been a chance finding. Furthermore, some participants, in some sites, did not perforate before the availability of CBCT but perforated the same sites after the availability of CBCT. Therefore, at the very least, it can be concluded that the availability of CBCT is no guarantee against perforation.
Conversely, however, this raises the question of whether this evidence should lead practitioners to abandon CBCT as an imaging modality when planning dental implant placement in the anterior edentulous mandible. First, this was a relatively small sample of dentists and mandibles. On that basis alone, the results should be interpreted with caution. Secondly, in the FGDP (UK) Selection Criteria in Dental Radiography, the authors comment that the choice of radiographic technique is complicated by a number of factors, including the experience of the practitioner.33 Our sample size was not calculated to account for demographic variables and, therefore, results for individual practitioners are not presented. Nevertheless, when CBCT was available, it was observed that some individuals created fewer perforations whilst others did not. Some, therefore, may be regarded as “responders” and others as “non-responders” to the availability of CBCT. Furthermore, in a 2011 study, Dimitrijevic et al38 investigated the depth and distance perception of dentists and dental students and commented that “ability to perform perceptual tasks varied enormously”. They conclude that “Some dentists … have great difficulty in accurately gauging depths and distances”. It remains a common sense position, therefore, that CBCT is helpful for some dentists and some cases. Based on this evidence, it would be inappropriate to suggest that CBCT should not be used in the pre-operative assessment of dental implant sites in the edentulous anterior mandible. In short, these results suggest that there is no case for routine prescription of CBCT for the pre-operative assessment of all implant cases. Nevertheless, it would be premature to suggest that CBCT has no place in the assessment of the anterior edentulous mandible when planning dental implant placement.
It is perhaps unsurprising that the availability of CBCT made no statistically significant difference to the selection of implant width when considering regular and challenging cases together. Nevertheless, where bone width is reduced, such as in the challenging cases, then this may begin to dictate the implant width.
It might be considered logical that implant length is unaffected by the availability of CBCT. Correcting for magnification, a panoramic view can be measured for the height of the mandible at the site of the proposed dental implants. Notwithstanding, the panoramic view does not show lingual concavities that might restrict the height available in which to safely place a dental implant. It may be reasoned, therefore, that the trans-symphyseal view is providing much of the information required to make a judgment on implant length. Furthermore, the lengths of the implant system provided are in 2-mm increments. Therefore, there would have to be a substantial difference in judgment made before and after the availability of CBCT for the selection of implant length to change. By contrast, the widths of the implant system provided are in 0.50- or 0.25-mm increments. It is, therefore, more likely that the more precise measurements offered by a CBCT image, at exactly the site of the proposed implant placement, would lead to a change in selection of implant width.
These results show that for challenging cases, practitioners assess the cases to be more difficult when presented with CBCT images than when presented only with conventional images. This difference in perception of difficulty is most likely to be represented by the difference between the information provided by the trans-symphyseal view and that provided by the CBCT view. The trans-symphyseal view provides an approximation of a cross-sectional image but, in reality, is a superimposition of the mandible from approximately canine to canine region. This obscures some detail and is probably most representative of the cross section at the midline. By contrast, the CBCT view provides a true cross-sectional image exactly at the site of the intended implant. For example, lingual concavities at the canine regions, but not at the midline, will be demonstrated on the CBCT view but may be obscured on the trans-symphyseal view.
Every effort was made to reproduce realistic clinical circumstances as far as possible. Nevertheless, dentistry carried out on a dental simulation can never be the same as dentistry carried out on a patient. For example, the drilling exercise was carried out without the presence of bleeding or saline coolant. There were no difficulties with local anaesthesia, patient co-operation or movement during the procedures. There were limitations on the time available to carry out the exercise although this may well also apply in clinical circumstances. Also, dentists may have taken longer to consider the images and plan their osteotomies in advance if these had been real patients. Notwithstanding, these same circumstances existed for both the “before” and “after” parts of the study and for all participants. The study design therefore controlled for these factors.
One important factor may be that the procedures were risk free. The participants did not have real concern of causing a perforation and possible haemorrhage on dental simulation. This may well have affected the preparation of osteotomies. On the other hand, however, the exercise was observed by the first author (AMS) and the participants would naturally have wished to prepare the best osteotomies they could in front of another dentist.
This study goes further than any previous investigations by encompassing Fryback and Thornbury's hierarchy of efficacy of diagnostic imaging Levels 3, 4 and 5. The investigation of assessment of case difficulty was appropriate to Level 3, diagnostic thinking efficacy. The investigation of selection of implant length, width and design was appropriate to Level 4, therapeutic efficacy. The investigation of perforations of the lingual surface of the mandible, and thus potentially fatal haemorrhage, was appropriate to Level 5, patient outcome efficacy. A novel method of conducting a before–after study was used that presents reproducible simulated cases in a phantom head. The method could easily be adapted to other parts of the jaws, for example, the posterior mandible or maxilla, for similar before–after studies. It may also be useful in education of dentists.
In conclusion, when placing dental implants in the edentulous anterior mandible, the results suggest that the availability of CBCT has no overall impact on the incidence of perforations of the lingual surface of bone. There is weak evidence that CBCT may be helpful in the more challenging cases for some dentists. The findings of this investigation tend to support the recommendations of the EAO and FGDP (UK) regarding selected use of cross-sectional imaging.33,37
References
- 1.Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology 2002; 19: 3–4. [PubMed] [Google Scholar]
- 2.Thomason JM, Feine J, Exley C, Moynihan P, Muller F, Naert I, et al. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients—the York Consensus Statement. Br Dent J 2009; 207: 185–6. doi: 10.1038/sj.bdj.2009.728 [DOI] [PubMed] [Google Scholar]
- 3.Pigadas N, Simoes P, Tuffin JR. Massive sublingual haematoma following osseo-integrated implant placement in the anterior mandible. Br Dental J 2009; 206: 67–8. doi: 10.1038/sj.bdj.2009.2 [DOI] [PubMed] [Google Scholar]
- 4.Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol 2004; 75: 631–45. [DOI] [PubMed] [Google Scholar]
- 5.Del Castillo-Pardo de Vera JL, López-Arcas Calleja JM, Burgueño-García M. Hematoma of the floor of the mouth and airway obstruction during mandibular dental implant placement: a case report. Oral Maxillofac Surg 2008; 12: 223–6. doi: 10.1007/s10006-008-0134-4 [DOI] [PubMed] [Google Scholar]
- 6.Boyes-Varley JG, Lownie JF. Haematoma of the floor of the mouth following implant placement. SADJ 2002; 57: 64–5. [PubMed] [Google Scholar]
- 7.Darriba MA, Mendonça-Caridad JJ. Profuse bleeding and life-threatening airway obstruction after placement of mandibular dental implants. J Oral Maxillofac Surg 1997; 55: 1328–30. [DOI] [PubMed] [Google Scholar]
- 8.Flanagan D. Important arterial supply of the mandible, control of an arterial hemorrhage, and report of a hemorrhagic incident. J Oral Implantol 2003; 29: 165–73. [DOI] [PubMed] [Google Scholar]
- 9.Givol N, Chaushu G, Halamish-Shani T, Taicher S. Emergency tracheostomy following life-threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J Periodontol 2000; 71: 1893–5. [DOI] [PubMed] [Google Scholar]
- 10.Isaacson TJ. Sublingual hematoma formation during immediate placement of mandibular endosseous implants. J Am Dent Assoc 2004; 135: 168–72. [DOI] [PubMed] [Google Scholar]
- 11.Kalpidis CD, Konstantinidis AB. Critical hemorrhage in the floor of the mouth during implant placement in the first mandibular premolar position: a case report. Implant Dent 2005; 14: 117–24. [DOI] [PubMed] [Google Scholar]
- 12.Krenkel C, Holzner K. Lingual bone perforation as causal factor in a threatening hemorrhage of the mouth floor due to a single tooth implant in the canine region. [In German.] Quintessenz 1986; 37: 1003–8. [PubMed] [Google Scholar]
- 13.Laboda G. Life-threatening hemorrhage after placement of an endosseous implant: report of case. J Am Dent Assoc 1990; 121: 599–600. [DOI] [PubMed] [Google Scholar]
- 14.Mason ME, Triplett RG, Alfonso WF. Life-threatening hemorrhage from placement of a dental implant. J Oral Maxillofac Surg 1990; 48: 201–4. [DOI] [PubMed] [Google Scholar]
- 15.Mordenfeld A, Andersson L, Bergström B. Hemorrhage in the floor of the mouth during implant placement in the edentulous mandible: a case report. Int J Oral Maxillofac Implants 1997; 12: 558–61. [PubMed] [Google Scholar]
- 16.Niamtu J, 3rd. Near-fatal airway obstruction after routine implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 597–600. [DOI] [PubMed] [Google Scholar]
- 17.Panula K, Oikarinen K. Severe hemorrhage after implant surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 87: 2. [DOI] [PubMed] [Google Scholar]
- 18.Ratschew C, Czernicky W, Watzek G. Life threatening haemorrhage following implant placement in the mandible. [In German.] Dtsch Zahnarztl Z 1994; 49: 65–7. [Google Scholar]
- 19.ten Bruggenkate CM, Krekeler G, Kraaijenhagen HA, Foitzik C, Oosterbeek HS. Hemorrhage of the floor of the mouth resulting from lingual perforation during implant placement: a clinical report. Int J Oral Maxillofac Implants 1993; 8: 329–34. [PubMed] [Google Scholar]
- 20.Weibrich G, Foitzik C, Kuffner H. Life threatening oral hemorrhage after implantation into the distal right mandible. [In German.] Mund Kiefer Gesichtschir 2002; 6: 442–5. [DOI] [PubMed] [Google Scholar]
- 21.Woo BM, Al-Bustani S, Ueeck BA. Floor of mouth haemorrhage and life-threatening airway obstruction during immediate implant placement in the anterior mandible. Int J Oral Maxillofac Surg 2006; 35: 961–4. [DOI] [PubMed] [Google Scholar]
- 22.Hofschneider U, Tepper G, Gahleitner A, Ulm C. Assessment of the blood supply to the mental region for reduction of bleeding complications during implant surgery in the interforaminal region. Int J Oral Maxillofac Implants 1999; 14: 379–83. [PubMed] [Google Scholar]
- 23.Longoni S, Sartori M, Braun M, Bravetti P, Lapi A, Baldoni M, et al. Lingual vascular canals of the mandible: the risk of bleeding complications during implant procedures. Implant Dent 2007; 16: 131–8. [DOI] [PubMed] [Google Scholar]
- 24.Hobkirk JA, Watson RM, Searson LJJ. Introducing dental implants. Edinburgh, UK: Churchill Livingstone; 2003. [Google Scholar]
- 25.Shelley AM, Horner K. A transymphyseal x-ray projection to assess the anterior edentulous mandible prior to implant placement. Dent Update 2008; 35: 689–94. [DOI] [PubMed] [Google Scholar]
- 26.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. [DOI] [PubMed] [Google Scholar]
- 27.Shelley AM, Glenny AM, Goodwin M, Brunton P, Horner K. Conventional radiography and cross-sectional imaging when planning dental implants in the anterior edentulous mandible to support an overdenture: a systematic review. Dentomaxillofac Radiol 2014; 43: 20130321. doi: 10.1259/dmfr.20130321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gibson RL, Barclay CW. Dental implantology education: a survey of opinion and experience of 106 general dental practitioners. Br Dent J 2006; 201: 367–70. [DOI] [PubMed] [Google Scholar]
- 29.Shelley AM, Brunton P, Horner K. Subjective image quality assessment of cross sectional imaging methods for the symphyseal region of the mandible prior to dental implant placement. J Dent 2011; 39: 764–70. doi: 10.1016/j.jdent.2011.08.008 [DOI] [PubMed] [Google Scholar]
- 30.Lindhe J, Lang NP, Karring T. Clinical periodontology and implant dentistry . Vol. 2. Oxford, UK: Blackwell Munksgard; 2008. [Google Scholar]
- 31.Palmer R, Howe LC, Palmer P. A clinical guide to implants in dentistry. London, UK: British Dental Association; 2008. [Google Scholar]
- 32.Palmer R, Smith BJ, Howe LC, Palmer PJ. Implants in clinical dentistry. London, UK: Martin Dunitz; 2002. [Google Scholar]
- 33.FGDP (UK). Selection criteria in dental radiography. 3rd edn. London, UK: Faculty of General Dental Practitioners (UK) Royal College of Surgeons of England; 2013. [Google Scholar]
- 34.Shelley AM, Wardle L, Goodwin MA, Brunton P, Horner K. A questionnaire study to investigate custom and practice of imaging methods for the anterior region of the mandible prior to dental implant placement. Dentomaxillofac Radiol 2013; 42: 20120179. doi: 10.1259/dmfr.20120179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schropp L, Wenzel A, Kostopoulos L. Impact of conventional tomography on prediction of the appropriate implant size. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 458–63. [DOI] [PubMed] [Google Scholar]
- 36.Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 817–26. doi: 10.1016/j.oooo.2012.03.005 [DOI] [PubMed] [Google Scholar]
- 37.Harris D, Horner K, Gröndahl K, Jacobs R, Helmrot E, Benic GI, et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A concensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res 2012; 11: 1243–53. doi: 10.1111/j.1600-0501.2012.02441.x [DOI] [PubMed] [Google Scholar]
- 38.Dimitrijevic T, Kahler B, Evans G, Collins M, Moule A. Depth and distance perception of dentists and dental students. Oper Dent 2011; 36: 467–77. doi: 10.2341/10-290-L [DOI] [PubMed] [Google Scholar]