Abstract
The psychological effects of war and resulting displacement continue to negatively impact Afghan refugees. The purpose of this study was to investigate factors that are associated with and predict psychological distress symptoms among Afghan refugees. We analyzed data from a diverse sample of 130 Afghan refugees recruited through non-random sampling in the San Diego area. Participants completed self-report questionnaires consisting of a culturally validated measure of psychological distress, the Afghan Symptom Checklist [ASCL] alongside standardized measures of acculturation, social support, and perceived stress. In bivariate analyses, older age, older age at migration, female gender, being widowed, having lower education, being unemployed, unable to comfortably pay monthly bills, lower acculturation and social support, and higher levels of perceived stress were associated with psychological distress. However, only few variables – female gender, being widowed, unable to comfortably pay monthly bills, and perceived stress – remained significant in multivariate analysis. The findings from this study contribute to understanding the social determinants of distress that affect Afghans in exile even after long-term resettlement in the US. These reported outcomes support the need for continued research with Afghans, alongside the implementation of culturally relevant psychosocial interventions that emphasize prevention of post-resettlement stressors immediately upon resettlement.
Keywords: Afghan, refugee, psychological distress, acculturation, social support
INTRODUCTION
Refugees, broadly defined, are individuals who are forced to flee their homelands (and unable to return) due to fears of persecution, war, or violence (UNHCR, 2011). Of the 10.5 million refugees accounted for globally at the end of 2012, approximately one in four (2.6 million) originate from Afghanistan, a country that has continued to represent the largest source country for refugees for over 30 consecutive years (UNHCR, 2012). Outside of Iran and Pakistan where most Afghans have resettled, western nations such as the United States (US) have hosted an estimated 65,000 Afghans (US Census Bureau, 2011). This has taken place in two major resettlement waves – in response to the Soviet occupation of the 1980s, and the current military intervention post-9/11. Afghans resettling in western nations show high risk for mental health problems partly due to war traumas that are compounded by cultural adjustment problems in a backdrop of losing family, community, and their way of life (Keyes, 2000), which precipitates ongoing stress (Wojcik & Bhugra, 2010).
Cross-sectional studies conducted with Afghans have shown elevated levels of depressive and posttraumatic symptomatology associated with war traumas and older age (Malekzai et al., 1996), Pashtun ethnicity (due to more exposure to violence) (Mghir, Freed, Raskin, & Katon, 1995); female gender, social support loss (Gerritsen et al., 2006; Ichikawa et al., 2006) as well as identity loss and discrimination (Stempel, 2009); poor language skills, lower education, unemployment (Lipson, Omidian, & Paul, 1995; Gernaat et al., 2002); problematic alcohol use and acculturative stress (Haasen et al., 2008); and social disadvantages linked to asylum status and residency challenges observed among newly resettled Afghan youth (Bronstein, Montgomery, & Dobrowlski, 2012) as well as adults (Steel et al., 2011). Risk factors for psychological distress show consistency with other refugee groups as consolidated in seminal systematic reviews (Lindert, von Ehrenstein, Priebe, Mielck, & Brähler, 2009; Porter & Haslam, 2005). Additionally, many qualitative studies conducted with Afghans validate these findings by showing thematic linkages between mental health problems and post-resettlement psychosocial challenges (Lipson & Omidian, 1997, 1993; Feldmann et al., 2007; Omeri et al., 2006, 2004).
While mental health symptoms may improve over time for the majority of Afghans, ongoing daily psychosocial stressors remain a risk factor for some even after long-term resettlement (Steel, Silove, Phan, & Bauman 2002). However, with the exception of Sulaiman-Hill and Thompson’s study (2011), many of the studies cited above have been conducted with Afghans shortly after resettlement. This makes it difficult to determine if psychological distress is an acute condition that can be resolved with changes in circumstances (e.g. English language acquisition, employment, social support), or a chronic condition needing therapeutic intervention (Marshall, Schell, Elliott, Berthold, & Chun, 2005).
Much emphasis thus far has been placed on identifying and reducing traumatic symptoms through psychotherapeutic interventions developed for western populations (Murray, Davidson, & Schweitzer, 2010; Nicholl & Thompson, 2004). This may partly be explained by the lack of guiding frameworks available for scientists and clinicians interested in tailoring interventions to work with refugees (Slobodin & de Jong, 2014). A rudimentary step in developing culturally appropriate interventions may depend on understanding the ways in which psychological distress is experienced and articulated (Miller et al., 2006). This study contributes to this area by exploring psychological distress symptoms as conceptualized through the use of a culturally grounded measure of mental health, the Afghan Symptom Checklist or ASCL (Miller et al., 2006) among (former) Afghan refugees in the San Diego area. The ASCL contains symptoms corresponding with dimensions of mental health known to Afghans including 1) functioning in the community (e.g. the degree of respect towards one’s neighbors), 2) functioning in one’s family (e.g. the degree to which one maintains harmonious family relations), and 3) one’s internal state (e.g. relative state of calm or agitation). The aims of this study were to examine variables that correlate with and predict psychological distress levels. As such we hypothesized that ASCL scores would be predicted by:
socio-demographic factors: older age, older age at migration, female gender, Pashtun ethnicity, lower education, unemployment, and being unmarried
acculturation-related variables: older age at migration, years resided in the US, and lower language acculturation;
lower social support, and
higher levels of perceived stress (relating to the degree to which Afghans find the situations in their lives as stressful).
METHOD
Participants and Procedures
Inclusion criteria for this study were limited to adult Afghans currently residing in San Diego County who originally resettled in the US as refugees and asylum seekers, or as immigrants originally fleeing Afghanistan under an element of duress. Power analysis using G*Power software, version 3.1 (Faul, Erdfelder, Lang, & Buchner, 2007) estimated that a sample size of 135 participants were required based on a moderate effect size of f2 = 0.15, type I error of α = .05, and power of (1 − β) = .80.
Convenience and snowball sampling techniques were used to recruit Afghans. This was deemed the most feasible and culturally-sensitive approach given the hard-to-reach nature of this population, their low numbers in the San Diego area, and the unavailability of a sampling frame discovered through preliminary qualitative research described elsewhere (Alemi & James, 2011). The first and third authors, along with a female Afghan research assistant (RA) from the local community, trained in data collection, conducted surveys at mosques, cultural festivals, and through accessing their personal social networks.
Females completed questionnaires mainly through interviews conducted in their homes in Dari by our RA (given literacy challenges) as opposed to males who completed questionnaires in Dari and English mainly through self-administration. All instruments were translated from English to Dari using a standard translation-back-translation technique. The ethical merits of this study and all informed consent documents were reviewed and approved by Loma Linda University Institutional Review Board. Verbal consent was obtained from participants. Participation was incentivized by a small cash donation given on behalf of participants to a local mosque or charity of their choosing.
Instruments
General Psychological Distress (Dependent Variable)
As noted above, the Afghan Symptom Checklist or ASCL (Miller et al., 2006) was used for measuring the frequency of distress symptoms. This scale was developed through narratives garnered from Afghans that identified locally meaningful indicators of well-being and distress, according to Miller et al. (2006). The ASCL consists of 23 distress indicators presented in the context of the previous two weeks. Items include those recognized by western psychiatry relating to depressive symptoms as well as indigenous idioms of distress relating to ruminative sadness and somatic distress and stress induced reactivity. Five response choices for each question are offered (1=“never”, 2=“1 day/week”, 3=“2–3 days/week”, 4=“4–5 days/week”, 5=“everyday”). Scores range from ‘23 to 115’ with higher scores indicative of higher distress levels. Both English and Dari versions of the measure (provided courtesy of Ken Miller, the ASCL’s author) were presented to two key-informants from the Afghan community and few community members for assessing face validity, which lead to minor grammatical adjustments. The ASCL demonstrated excellent internal consistency (Cronbach’s α = 0.936).
Socio-demographic information
On the basis of prior mental health research with Afghan refugees, we collected data on age, gender, marital status, education (in years completed and in terms of attainment level), ethnicity, number of years resided in Afghanistan during any period of conflict (proxy for exposure to war traumas), employment status, and income. To avoid potential inconsistencies in income data given confusions over pre-tax vs. post-tax income, other income sources, along with the lack of cultural congruency of such a question we asked participants “Can you comfortably pay your bills every month with your current household income?” with a binary ‘yes/no’ response choice as demonstrated in a recent study of Korean-Americans (Song et al., 2010). Additionally subcategories within the ethnicity and employment variables were combined given their sparse numbers, for example Hazara, Nuristanis, and Uzbeks were categorized as one group; and, for employment status, disabled participants were combined with the retired subgroup. Also, because of systematic inconsistencies in the continuous education variable, we used the categorical education variable in all analyses.
Acculturation
Two separate proxy measures of acculturation were incorporated into our instrument, which included ‘age at migration’ to the US and the ‘number of years resided in the US,’ used in previous research for assessing acculturation in Latino immigrants (Thomson & Hoffman-Goetz, 2009). Additionally, we used a standardized measure of language acculturation developed and validated by Deyo, Diehl, Hazuda, and Stern (1985) in a clinical study with Mexican-Americans. Items focus on language use and preference. The first question queries respondents on the first language they learned to speak through four response choices (1=”English, 2=“English and Dari/Pashto simultaneously”, 3=“Dari or Pashto, 4=“other”) (We substituted the term “Spanish” with the terms “Dari/Pashto”). Three items that assess respondents’ perceptions on their ability to speak Dari or Pashto, speak English, and read English followed this. Response choices here are provided on a four-point scale (1=“very well”, 2=“pretty well”, 3=“not too well”, and 4=“not at all”). Furthermore, four additional items elicited responses relating to one’s language use or preference with one’s 1) spouse, 2) children, 3) parents, and 4) in family gatherings on a five-point scale (1=“only English, 2=“mostly English”, 3=“both equally”, 4=“mostly Dari/Pashto”, 5=“only Dari/Pashto”). For assuring consistency, we inserted the following statements in parentheses at the end of each respective question for those not having a spouse, “or with your fiancée or a best friend if you are not married;” for participants without children: “or with family members who are children, if you have no children”; for participants without parents: “or with older family members if you have no parents.” We followed a scoring rubric provided by Deyo et al. (1985) indicating that scores range from ‘0 to 4’ with higher scores indicative of higher levels of (language) acculturation. This acculturation scale demonstrated marginal internal consistency (Cronbach’s α = 0.685).
Perceived social support
The Lubben Social Network Scale-6 or LSNS-6 originally developed for use with elderly adults was used as a general measure of perceived social support here. The scale consists of six items used to measure the size, closeness, and frequency of contacts in an individual’s social network. As such, questions are presented on two subscales, one relating to the number of relatives, and the other to friends seen or heard from in the context of a one-month period, in which private matters could be discussed with, and who can be called on for help. The scales’ total score is an equally weighted sum of the six items. Scores range from 0 to 30 with higher scores indicative of higher levels of perceived social support. The LSNS demonstrated adequate internal consistency (Cronbach’s α = 0.866).
Perceived stress
The Perceived Stress Scale-10 (Cohen et al., 1983) was used to measure perceived stress. According to Cohen et al. (1993) respondents are measured on the degree to which they feel situations in their lives are appraised as stressful. Items on the PSS were designed to tap how unpredictable, uncontrollable, and overloaded respondents find their lives. The questions are asked in the context of the previous month. Response choices are provided on a five-point scale (0=“not at all”, 1=“almost never”, 2=“sometimes”, 3=“fairly often”, 4=“very often”). Scores on four negatively stated items (4, 5, 7, and 8) are reversed so that higher scores reflect greater perceived stress and then summed across all scale items. Scores range from ‘0 to 40’ with higher scores indicative of higher levels of perceived stress. The PSS demonstrated adequate internal consistency (Cronbach’s α = 0.811).
Data Analysis
We used SPSS, version 21.0 for all data analysis. We generated descriptive statistics for all continuous and categorical variables and applied independent samples t-tests, ANOVAs, and Pearson correlations as appropriate to identify significant associations with ASCL scores/psychological distress at the bivariate level. We evaluated standard assumptions of parametric tests (e.g. linearity, normality, homoscedasticity, multicollinearity), which warranted no data transformations, and made no data imputations for cases with missing data following complete case analysis guidelines. Four cases consisting of more than 10% missing responses were eliminated. Multiple linear regression analysis was subsequently conducted to examine the relationship between the independent variables (significant at the bivariate level) and psychological distress.
RESULTS
Socio-demographic Characteristics
A sample of 130 Afghans participated in this study in which 74 (56.9%) were male and 56 were female (43.1%) ranging in age 18 to 85 years. The mean age of the sample was 42.09 years (sd = 15.55). Participants resided in the US for approximately 17 years, had spent nearly nine years residing in Afghanistan during war before resettling in the US at close to 25 years of age. Most participants were married (n = 84, 64.6%); six were either divorced or separated, 12 were widowed, and the remainder reported being ‘never married.’ Educational levels varied widely with nearly half possessing a college education, while in contrast the other half possessed a high school diploma (n = 42, 32.3%) or less (n = 28, 21.5%). Most participants were of Pashtun ethnicity (n = 60, 46.2%), followed by Tajik (n = 38, 29.2%), while the remainder represented minority groups such as Hazara, Nuristani, and Uzbek (n = 20, 15.4%). Over half were employed, and the majority of participants (n = 93, 72.7%) were comfortable in paying monthly bills with their current household income.
Descriptive Analyses
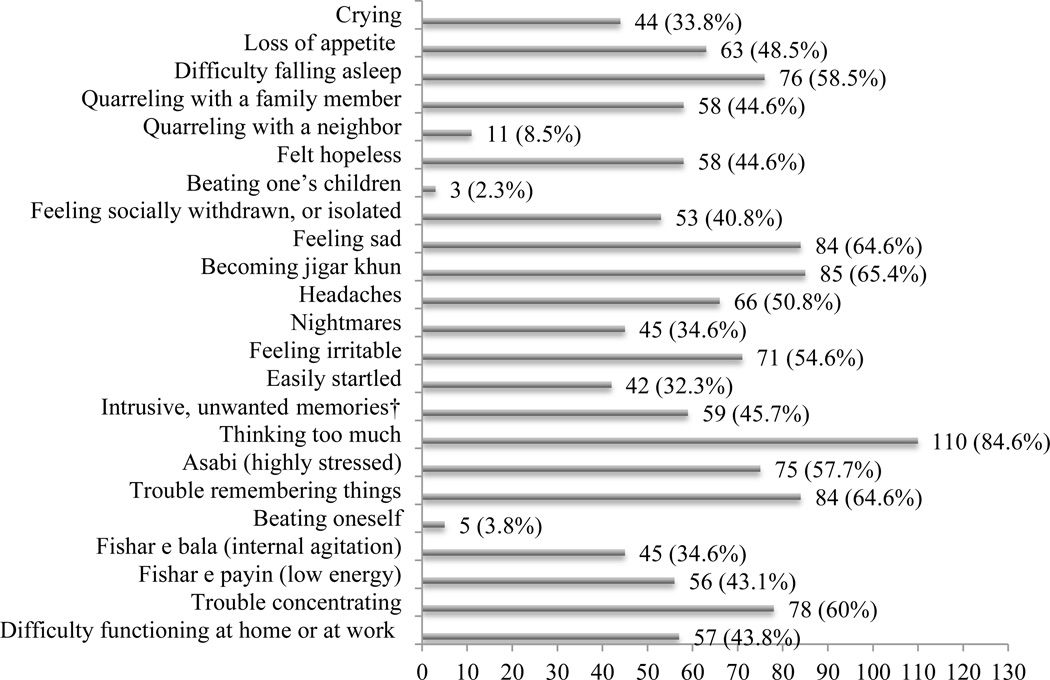
ASCL scores ranged from 23 to 88 with a mean of 41.7 (sd = 15.55). Figure 1 provides a percentage breakdown of distress symptoms occurring at least once per week. Concentration-related symptoms such as ‘thinking too much’ (rumination about one’s problems), ‘trouble remembering things’, and ‘trouble concentrating’ occurred often. Symptoms related to ruminative sadness, i.e. ‘feeling sad’ and ‘becoming jigar khun’ (a form of sadness that includes grief following interpersonal loss or a reaction to any deeply disappointing or painful experience (Miller et al., 2006)) was also common as were ‘insomnia’, ‘headaches’, ‘irritability’, and ‘feeling highly stressed,’ which over 50% of our sample reported.
Figure 1.
Frequency of reported distress symptoms occurring ≥1/week (N= 130)
Note: †n= 129
Additionally, females tended to report more distress symptoms than males across all items, with 10 items showing significantly higher rates as reported in Table 1.
Table 1.
Frequency of reported distress symptoms occurring ≥1/week (N = 130)
| M (SD) |
||
|---|---|---|
| Males | Females | |
| Crying | 1.24 | 2.09*** |
| Loss of appetite | 1.80 | 1.96 |
| Difficulty falling asleep | 1.85 | 2.50** |
| Quarreling with a family member | 1.57 | 1.86 |
| Quarreling with a neighbor | 1.09 | 1.14 |
| Felt hopeless | 1.61 | 2.27** |
| Beating one’s children | 1.01 | 1.07 |
| Feeling socially withdrawn, or isolated | 1.63 | 1.95 |
| Feeling sad | 2.02 | 2.41 |
| Becoming jigar khun (reaction to a painful experience) | 2.00 | 2.32 |
| Headaches | 1.58 | 2.13** |
| Nightmares | 1.41 | 1.66 |
| Feeling irritable | 1.66 | 2.39*** |
| Easily startled | 1.28 | 1.96*** |
| Intrusive, unwanted memories† | 1.59 | 2.20** |
| Thinking too much | 2.59 | 3.27** |
| Asabi (highly stressed) | 1.80 | 2.29* |
| Trouble remembering things | 2.05 | 2.45 |
| Beating oneself | 1.08 | 1.05 |
| Fishar e bala (internal agitation) | 1.47 | 1.88* |
| Fishar e payin (low energy) | 1.76 | 1.89 |
| Trouble concentrating | 1.95 | 2.29 |
| Difficulty meeting responsibilities at home or at work | 1.68 | 1.96 |
Note:
N = 129; 0=not at all, 1=“never”, 2=“1 day/week”, 3=“2–3 days/week”, 4=“4 to 5 days/week”, 5=“everyday”;
p <. 05;
p <. 01;
p < .001
ASCL scores were significantly higher for participants who reported being ‘widowed’ (F(3, 125) = 10.915, p < .05) than other marital groups (see Table 2) Furthermore, participants with a college degree reported significantly lower ASCL scores (F(2,127) = 6.35, p < .05) than those possessing ‘less than a high school education’ while the group possessing a high school diploma did not differ significantly from either of the two groups. Participants who reported being ‘disabled or retired’ and ‘unemployed’ showed significantly higher levels of psychological distress (F(2,126) = 13.61, p < .05) than those currently employed. Significantly higher distress levels were found in participants unable to ‘comfortably pay monthly bills’ (t(126) = 2.79, p < .05).
Table 2.
Descriptive statistics: categorical variables and dependent variable (ASCL) measured at bivariate level (N = 130)
| Variables | ASCL Score | Statistic | |||
|---|---|---|---|---|---|
| n (%) | m | sd | t or F | p-value | |
| Gender | |||||
| Female | 56 (43.1) | 46.98 | 18.02 | 3.33 | .001 |
| Male | 74 (56.9) | 37.72 | 12.05 | ||
| Marital Status | |||||
| Divorced or separated | 6(4.6) | 50.12 | 16.86 | 10.915 | .000 |
| Widowed | 12 (9.2) | 61.75 | 17.81 | ||
| Never Married | 28 (21.5) | 40.96 | 14.62 | ||
| Married | 84 (64.6) | 38.50 | 12.83 | ||
| Education | |||||
| Less than high school | 28 (21.5) | 49.81 | 18.86 | 3.022 | .003 |
| High school diploma | 42 (32.3) | 43.09 | 16.29 | ||
| Bachelor’s Degree or Higher | 60 (46.2) | 37.25 | 11.59 | ||
| Ethnicity | |||||
| Pashtun | 60 (46.2) | 41.30 | 15.96 | .637 | .592 |
| Tajik | 38 (29.2) | 39.73 | 12.79 | ||
| Hazara, Nuristani, Uzbek | 20 (15.4) | 44.85 | 16.47 | ||
| Other | 12 (9.2) | 45.91 | 20.78 | ||
| Employment† | |||||
| Disabled or Retired | 15 (11.6) | 52.60 | 22.44 | 4.331 | .000 |
| Unemployed | 38 (29.5) | 48.24 | 17.24 | ||
| Employed | 76 (58.9) | 36.42 | 10.01 | ||
| Income‡ | |||||
| Not comfortable paying monthly bills | 35 (27.3%) | 48.74 | 19.12 | 2.79 | .008 |
| Comfortable | 93 (72.7%) | 38.97 | 12.83 | ||
Note:
N = 129,
N = 128
Pearson correlations revealed weak but positive relationships between psychological distress and ‘age’ (r(126) = .188, p < .05) and ‘age at migration’ (r(123) = .262, p < .01); and, a weak but negative relationship with language acculturation (r(127) = −.184, p < .05), suggesting higher psychological distress in individuals with lower English language preference (see Table 3). Psychological distress levels were also negatively correlated with perceived social support levels; however, participants exerted a strong positive correlation (r(124) = .667, p < .01) with perceived stress.
Table 3.
Descriptive statistics: continuous variables and dependent variable (ASCL) measured at bivariate level (N = 130)
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ASCL | 41.70 | 15.55 | — | ||||||
| 2 | Age (18–85) | 42.09 | 15.66 | .188* | — | |||||
| 3 | Age at Migration (2–65) | 24.82 | 14.19 | .262** | .826** | — | ||||
| 4 | Years resided in US (<1–32) | 16.86 | 8.80 | −.032 | .426** | −.159 | — | |||
| 5 | Years resided in Afghanistan (0–40) | 8.73 | 8.49 | .166 | .097 | .366** | −.388** | — | ||
| 6 | Acculturation (0–4) | 1.24 | .68 | −.184* | −.321** | −.538** | .286** | −.389** | — | |
| 7 | Social Support (0–30) | 16.83 | 6.44 | −.249** | .036 | −.109 | .165 | −.143 | .128 | — |
| 8 | Perceived Stress (0–40) | 15.15 | 6.93 | .667** | .06 | .125 | −.048 | −.015 | −.086 | −.227* |
Note: N = 130 for ASCL; Due to missing data, N ranges from 125 to 129 for all other variables;
p < 0.01 (2-tailed);
p < .05 level (2-tailed)
Model Predicting Psychological Distress
Due to missing data, 12 cases were automatically eliminated during the regression analysis. Additionally, for ensuring meaningful interpretations, we dummy coded the marital status (widows = 0), education (less than high school diploma = 0) and employment (unemployed = 0) variables and compared them with reference groups (coded with ‘1’) that would serve as useful comparisons (Cohen, Cohen, West, & Aiken, 2003). Of the seven demographic variables entered into the regression model, three significantly contributed to the overall model, partially supporting our first research hypothesis testing the predictive relationship between socio-demographic characteristics and psychological distress levels. Specifically, being a female (t(117) = −.370, p = .020), widowed (t(117) = 3.862, p = .000), and not being able to ‘comfortably pay monthly bills’ were predictive of higher levels of psychological distress (t(117) = −2.912, p = .004). Measures of acculturation, including our proxy measure (i.e. 'age at migration') (t(117) = −.520, p = .604), along with the standardized measure of language preference did not significantly predict psychological distress (t(117) = .417, p = .678), which does not affirm our second research hypothesis testing the predictive relationship between acculturation and psychological distress. Our third research hypothesis, which tested the predictive relationship between perceived social support and psychological distress was also unsupported (t(117) = −1.100, p = .274). However, higher levels of perceived stress were found to significantly predict psychological distress (t(117) = 9.182, p = .000), affirming our fourth and final research hypothesis. Overall, results from the multiple linear regression analysis indicate that the model significantly predicts psychological distress, R2 = .630, R2adjusted = .595, F(10, 107) = 18.209, p < .001. This model accounts for 63% of the variance observed in psychological distress. A summary of coefficients is presented in Table 4.
Table 4.
Multiple Linear Regression Analysis Predicting Psychological Distress
| Unstandardized Coefficients |
Standardized Coefficients |
||||
|---|---|---|---|---|---|
| B | SE | β | t | Sig. | |
| (Constant) | 24.873 | 5.954 | 4.178 | .000 | |
| Age | .165 | .110 | .164 | 1.494 | .138 |
| Gender: femalea | −5.036 | 2.125 | −.161 | −2.370 | .020 |
| Marital Status: widowedb | 14.904 | 3.859 | .280 | 3.862 | .000 |
| Education: less than high school diplomac | −.222 | 2.624 | −.006 | −.085 | .933 |
| Employment: unemployedd | 1.131 | 2.365 | .033 | .478 | .633 |
| Income/Comfort Paying Monthly Bills?: Noe | −6.229 | 2.139 | −.182 | −2.912 | .004 |
| Age at Migration | −.071 | .137 | −.065 | −.520 | .604 |
| Acculturation | .695 | 1.669 | .032 | .417 | .678 |
| Social Support | −.173 | .157 | −.071 | −1.100 | .274 |
| Perceived Stress | 1.304 | .142 | .569 | 9.182 | .000 |
Note: N = 118 as 12 cases omitted by listwise deletion
Reference category is male
Reference category is being married
Reference category is having a college degree
Reference category is being employed
Reference category is ‘comfortably paying monthly bills’
DISCUSSION
In this study we applied a culturally grounded measure of mental health, the ASCL, to explore the frequency and types of distress symptoms among a diverse sample of former Afghan refugees residing in the San Diego area. Furthermore, we examined factors that were associated with and that contributed to predicting psychological distress levels. Psychological distress experiences included depressive- and anxiety-like symptoms, concentration-related difficulties, and somatic complaints, all of which were more common in women. The rate at which certain symptoms occurred along with group differences observed coincide with results reported among Afghans residing in Kabul (Miller et al., 2006), which further gives credence to the ASCLs cultural validity even when applied in a western context. However, overall distress levels were, as expected, comparatively lower in our sample compared to Miller et al.’s findings, possibly due to the relative safety and security of life in the US notwithstanding the many perpetual life difficulties that Afghans endure.
This was exemplified through bivariate analyses, which replicated findings from previous cross-sectional studies of Afghans resettled in western nations shortly after resettlement (Gerritsen et al., 2006; Ichikawa et al., 2006; Stempel, 2009; Sulaiman-Hill & Thompson, 2011). Specifically, our findings show that risk factors for psychological distress include a number of socio-demographic variables (e.g. female gender, older age, lower levels of education, being widowed, etc.), in addition to lower levels of acculturation, social support, and higher perceived stress. Our findings also corroborate the subjective qualitative accounts related to perceived post-resettlement stressors (employment, income, language difficulties, social support loss) previously documented with Afghans (Feldmann et al., 2007; Lipson & Omidian, 1997, 1993). This also affirms the predictive ability of our ‘perceived stress’ variable, showing that life situations appraised as uncontrollable or stressful have a negative effect on mental health.
Because our results, which are based on a sample of Afghans with long-term resettlement, show consistency with published studies of newly resettled Afghans, it suggests that circumstances for some may not have changed even decades after resettlement. This further suggests that for this population psychological distress is a chronic rather than an acute condition (Marshall et al., 2005), warranting the need for culturally relevant psychosocial interventions implemented early in the resettlement process to prevent the lasting effects of various post-resettlement deficiencies on mental health.
Such early interventions should place much focus on women, who in our study were disproportionately affected by psychological distress. Elevated psychological distress levels among women may be attributable to constant worries regarding their family’s well-being in the US and abroad, encountering more acculturation-related difficulties as compared to their male counterparts, and having to manage cultural conflicts with children (Lipson & Omidian, 1997). Moreover, intergenerational problems may also affect widows (a subgroup found here to be disproportionately affected by psychological distress) as part of having to care for many children in single parent households. While specific ethno-religious groups are known to have faced much repression in Afghanistan (Saikal, 2012), our findings did not support the association between ethnicity and psychological distress as compared to previously published research (Mghir et al., 1995). Explanations for this are that minority groups such as Hazaras were underrepresented in our sample and/or that previous studies focused on newly resettled groups whose memories of violence were relatively recent.
Our data shows that other vulnerable groups include individuals possessing lower education. While this variable was not predictive of psychological distress, facilitating education and even vocational training for Afghans could nonetheless ensure gainful employment that is non-subjugating and consistent with interests and skills (especially for men). This, along with addressing English language barriers at the outset can prove beneficial in terms of navigating health and social systems of care, and for ultimately securing adequate income, which was a variable predictive of psychological distress here. English language barriers have been documented as a major source of socio-economic burden, and of distress-related outcomes for Afghans (Gernaat et al., 2002; Lipson, Omidian, & Paul, 1995). Surprisingly, the language acculturation variable was not predictive of psychological distress, possibly due to low scale reliability. We, in addition, found that acculturation proxy measures were not predictive of psychological distress either. However, attention should be given to Afghans of older age (significant only at the bivariate level) who may be at higher risk for mental health problems as influenced by the acculturation process.
Language barriers have the potential to propagate first generation Afghans’ perceived sense of cultural dislocation, status dissonance, and social isolation as observed in prior studies (Omeri et al., 2006, 2004; Sulaiman-Hill & Thompson, 2011). However, because Afghans generally desire to maintain their own culture and identity, while possibly accepting the need to improve their livelihoods in the US, mental health models promoting Berry’s (1986) notion of cultural integration (valuing relations with the dominant group and ones’ own culture) could help promote and sustain mental health. This is further supported by the theory of demoralization, which suggests that borrowing values from both cultures and applying them judiciously are more conducive to mental health than indiscriminately subscribing to either culture (de Figueiredo, 2014). Cultural integration may depend on promoting social support through improving ties and social capital within communities, alongside facilitating bonds or cultural exchanges with non-Afghan communities (Strang & Ager, 2010). This could help reduce feelings of alienation and promote a sense of belonging, which may help ensure increases in self-esteem and environmental mastery.
Practice Implications
Future research should replicate the results of this study with larger and more representative samples, and to consider measuring physical health and disability-related variables, as well as quality of life. This, along with the focus on reducing the many idioms and indicators of distress documented here could provide for effective parameters of success in terms of evaluating culturally relevant intervention approaches. Though requisite to developing psychosocial interventions for Afghans, the preventive measures described above, for example, placing focus on specific demographic subgroups in terms of improving English language proficiency, employment prospects, and social supports early-on could prove useful in helping to sustain mental health across the life course. Non-stigmatizing community-based centers and places of worship can provide the necessary infrastructure for delivering such interventions.
Limitations of this Study
There are several limitations to this study. First, the cross-sectional design does not allow for implying causal inferences. Secondly, the limited sample size, which was based on non-random sampling procedures, limits generalizability. The small population of Afghans in the San Diego area, unfamiliarity with the research process and completing surveys, along with literacy challenges (or the shame associated with exposing this among males) provide some explanation for this. Other potential sources of bias include problems with our measurement procedures and instruments. The comprehension of questionnaire items between males and females may have varied as most males completed questionnaires through self-administration as opposed to females who were interviewed. Also, we used a unidimensional acculturation measure with low scale reliability, which was limited to assessing language preference and not other factors such as behaviors, values, beliefs, and attitudes.
Contributor Information
Dr Qais Alemi, Email: qalemi@llu.edu, Loma Linda University, Social Work & Social Ecology, 1898 Business Ctr. Dr., San Bernardino, 92408 United States.
Dr Sigrid James, Email: ssjames@llu.edu, Loma Linda University, Social Work & Social Ecology, San Bernardino, United States.
Ms Hafifa Siddiq, Email: hafifasiddiq@ucla.edu, University of California Los Angeles, Nursing, Los Angeles, United States.
Dr Susanne Montgomery, Email: smontgomery@llu.edu, Loma Linda University, Social Work & Social Ecology, San Bernardino, United States.
References
- Alemi Q, James S. Identifying strategies of gaining access to the Afghan refugee population: a qualitative study; Paper presented at the American Public Health Association 139th Annual Meeting and Exposition; Washington, DC. 2011. Oct, [Google Scholar]
- Bentley JA, Thoburn JW, Stewart DG, Boynton LD. Post-Migration Stress as a Moderator Between Traumatic Exposure and Self-Reported Mental Health Symptoms in a Sample of Somali Refugees. Journal of Loss & Trauma. 2012;17(5):452–469. [Google Scholar]
- Bronstein I, Montgomery P. Sleeping patterns of Afghan unaccompanied asylum-seeking adolescents: a large observational study. PLoS ONE. 2013;8(2):e56156. doi: 10.1371/journal.pone.0056156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronstein I, Montgomery P, Dobrowolski S. PTSD in asylum seeking male adolescents from Afghanistan. Journal of Traumatic Stress. 2012;25(5):551–557. doi: 10.1002/jts.21740. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Routledge: 2013. [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7,000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–1314. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- Feldmann CT, Bensing J, Ruijter A. Worries are the mother of many diseases: general practitioners and refugees in the Netherlands on stress, being ill and prejudice. Patient Education and Counseling. 2007;65(3):369–380. doi: 10.1016/j.pec.2006.09.005. [DOI] [PubMed] [Google Scholar]
- de Figueiredo JM. Explaining the ‘immigration advantage’ and the ‘biculturalism paradox’: an application of the theory of demoralization. International Journal of Social Psychiatry. 2014;60(2):175–177. doi: 10.1177/0020764013477018. [DOI] [PubMed] [Google Scholar]
- Keyes EF. Mental health status in refugees: an integrative review of current research. Issues in mental health nursing. 2000;21(4):397–410. doi: 10.1080/016128400248013. [DOI] [PubMed] [Google Scholar]
- Gerritsen A, Bramsen I, Deville� W, van Willigen L, Hovens J, Ploeg H. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Social Psychiatry & Psychiatric Epidemiology. 2006;41(1):18–26. doi: 10.1007/s00127-005-0003-5. [DOI] [PubMed] [Google Scholar]
- Haasen C, Sinaa M, Reimer J. Alcohol use disorders among Afghan migrants in Germany. Substance Abuse. 2008;29(3):65–70. doi: 10.1080/08897070802218828. [DOI] [PubMed] [Google Scholar]
- Ichikawa M, Nakahara S, Wakai S. Effect of post-migration detention on mental health among Afghan asylum seekers in Japan. Aust NZ J Psychiatr. 2006;40(4):341–346. doi: 10.1080/j.1440-1614.2006.01800.x. 2006. [DOI] [PubMed] [Google Scholar]
- Lindert J, Ehrenstein OS, Priebe S, Mielck A, Brähler E. Depression and anxiety in labor migrants and refugees—a systematic review and meta-analysis. Social Science & Medicine. 2009;69(2):246–257. doi: 10.1016/j.socscimed.2009.04.032. [DOI] [PubMed] [Google Scholar]
- Lipson JG. Afghan refugee health: some findings and suggestions. Qualitative Health Research. 1991;1(3):349–369. [Google Scholar]
- Lipson J, Omidian PA. Afghan refugee issues in the US social environment. Western Journal of Nursing Research. 1997;19(1):110–119. doi: 10.1177/019394599701900108. [DOI] [PubMed] [Google Scholar]
- Lipson J, Omidian P, Paul S. Afghan health education project: a community survey. Public Health Nursing. 1995;12(3):143–150. doi: 10.1111/j.1525-1446.1995.tb00002.x. [DOI] [PubMed] [Google Scholar]
- Malekzai A, Niazi JM, Paige SR, Hendricks SE, Fitzpatrick D, Leuschen M, Millimet C. Modification of CAPS-1 for diagnosis of PTSD in Afghan refugees. Journal of Traumatic Stress. 1996;9(4):891–898. doi: 10.1007/BF02104111. [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL, Elliott MN, Berthold SM, Chun CA. Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA. 2005;294(5):571–579. doi: 10.1001/jama.294.5.571. [DOI] [PubMed] [Google Scholar]
- Mghir R, Raskin A. The psychological effects of the war in Afghanistan on young Afghan refugees from different ethnic backgrounds. International Journal of Social Psychiatry. 1999;45(1):29–40. doi: 10.1177/002076409904500104. [DOI] [PubMed] [Google Scholar]
- Mghir R, Freed W, Raskin A, Katon W. Depression and posttraumatic stress disorder among a community sample of adolescent and young adult Afghan refugees. Journal of Nervous Mental Disease. 1995;183:24–30. doi: 10.1097/00005053-199501000-00005. [DOI] [PubMed] [Google Scholar]
- Omeri A, Lennings C, Raymond L. Beyond asylum: implications for nursing and health care delivery for Afghan refugees in Australia. Journal of Transcultural Nursing. 2006;17(1):30–39. doi: 10.1177/1043659605281973. [DOI] [PubMed] [Google Scholar]
- Omeri A, Lennings C, Raymond L. Hardiness and transformational coping in asylum seekers: the Afghan experience. Diversity in Health Social Care. 2004;1:21–30. [Google Scholar]
- Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons. JAMA. 2005;294(5):602–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- Saikal A. Afghanistan: the status of the Shi'ite Hazara minority. Journal of Muslim Minority Affairs. 2012;32(1):80–87. [Google Scholar]
- Stempel C. Social and experiential influence on the mental health of first generation Afghans in Northern California. Paper presented at Global Knowledge Conference: Afghan and Iranian Diaspora Cultures and Communities in the Bay Area; Hayward, CA. 2009. [Google Scholar]
- Sulaiman-Hill CR, Thompson SC. Thinking too much—psychological distress, sources of stress and coping strategies of resettled Afghan and Kurdish refugees. Journal of Muslim Mental Health. 2011;6(2):63–86. [Google Scholar]
- Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Social Science & Medicine. 2009;69(7):983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]