Abstract
Hamartomas, also known as fibroadenolipomas, are rare, benign formations that can develop in various organs, including the breast. They present clinically as a soft, mobile nodular lesions and are generally asymptomatic. They may be discovered incidentally during imaging studies performed for other reasons. Owing to the increasingly widespread use of mammographic screening, the diagnosis of breast hamartomas is on the rise. The masses are associated with specific mammographic and sonographic features that reflect their diverse tissue components. They also appear to present reproducible features on elastography. This article reviews the typical features of breast hamartomas seen on these three imaging modalities.
Keywords: Breast hamartoma, Ultrasound, Breast elastography
Sommario
L’amartoma, o fibroadenolipoma, è una rara formazione benigna che può insorgere in diversi organi, tra i quali la mammella. Clinicamente si presenta con aspetto nodulare soffice e mobile rispetto ai piani circostanti; generalmente asintomatico, può rappresentare un riscontro occasionale nel corso di esami strumentali, in particolare la diffusione dei programmi di screening mammografico ha comportato un maggiore riscontro di tale lesione. Presenta caratteristiche mammografiche ed ecografiche peculiari, legate alle differenti componenti tissutali che lo costituiscono. Anche l’elastonosografia mostra aspetti riproducibili. Vengono presentati gli aspetti tipici di questa lesione con ecografia, mammografia ed elastosonografia.
Introduction
Hamartomas are benign formations that can develop in various organs, including the lungs, kidneys, skin, and breasts. They consist of circumscribed masses (often enclosed in a pseudocapsule) containing a mixture of different tissues from the surrounding organ [1]. Hamartoma of the breast was described for the first time in 1971 by Arrigoni et al. Depending on the predominant type of breast tissue involved, the masses were referred to as “lipofibroadenoma”, “fibroadenolipoma”, or “adenolipoma” [2]. In 1973, Davies and Riddell introduced the term myoid hamartoma to refer to those rare hamartomas that contain substantial amounts of smooth muscle tissue [3].
Breast hamartomas contain glandular epithelium, adipose tissue, and fibrous tissue in variable proportions [2]. They are characterized by slow growth and vary in size from tiny masses to tumor-like formations measuring 10–12 cm in diameter, which may occupy almost the entire breast. Hamartomas represent 4–8 % of the benign breast lesions diagnosed in women. They are extremely rare in males [1, 4]. They can develop at any age after puberty. Up to 60 % of hamartomas are subclinical, that is, they cannot be detected by palpation. Clinically evident forms present on physical examination as soft, round, or oval nodular formations that are smooth surfaced and mobile against the surrounding tissues. They are generally not associated with any symptoms. The increasing use of screening mammography has led to an increase in the diagnosis of breast hamartomas [4].
US appearance
The US presentations of hamartomas differ widely owing to the marked variability in the adipose and fibrous tissue contents. In most cases, they appear as solid, well-defined, oval formations lying parallel to the skin plane. The echo structure is inhomogeneous with hypoechoic areas intermixed with hyperechoic band-like or nodular areas, reflecting the presence of adipose, epithelial, and fibrous connective tissues (Figs. 1, 2). Some lesions have a bull’s-eye or multilayered appearance on mammography (discussed below), which is pathognomonic. Hypervascularization is absent on color Doppler imaging. The diagnosis can be difficult when the mass is small with a low fat content and the pseudocapsule is incomplete [4, 5]. Hamartomas with substantial amounts of adipose tissue sometimes resemble lipomas (Fig. 3).
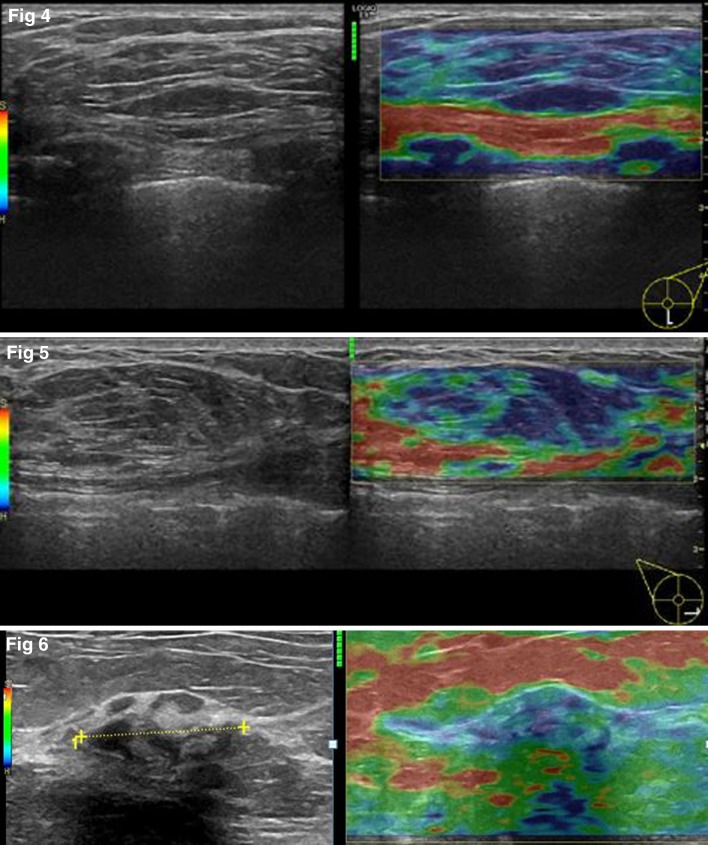
Fig. 1–2.
Ultrasonography shows a solid oval formation with inhomogeneous echo structure reflecting the presence of hypoechoic and hyperechoic tissue components, which is typical of hamartomas
Fig. 3.
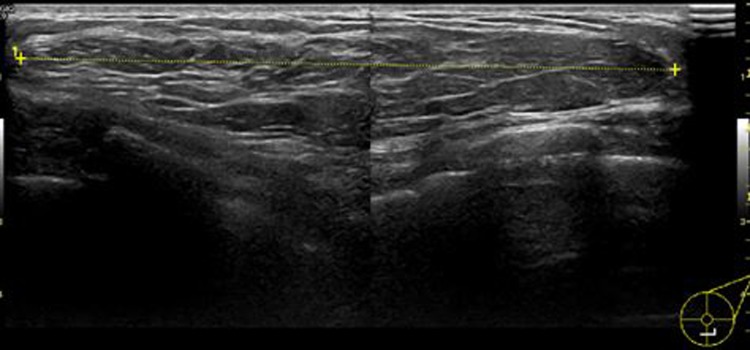
Ultrasound shows a large oval mass with large areas that are isoechoic relative to the surrounding fat tissue in a hamartoma made up predominantly of adipose tissue
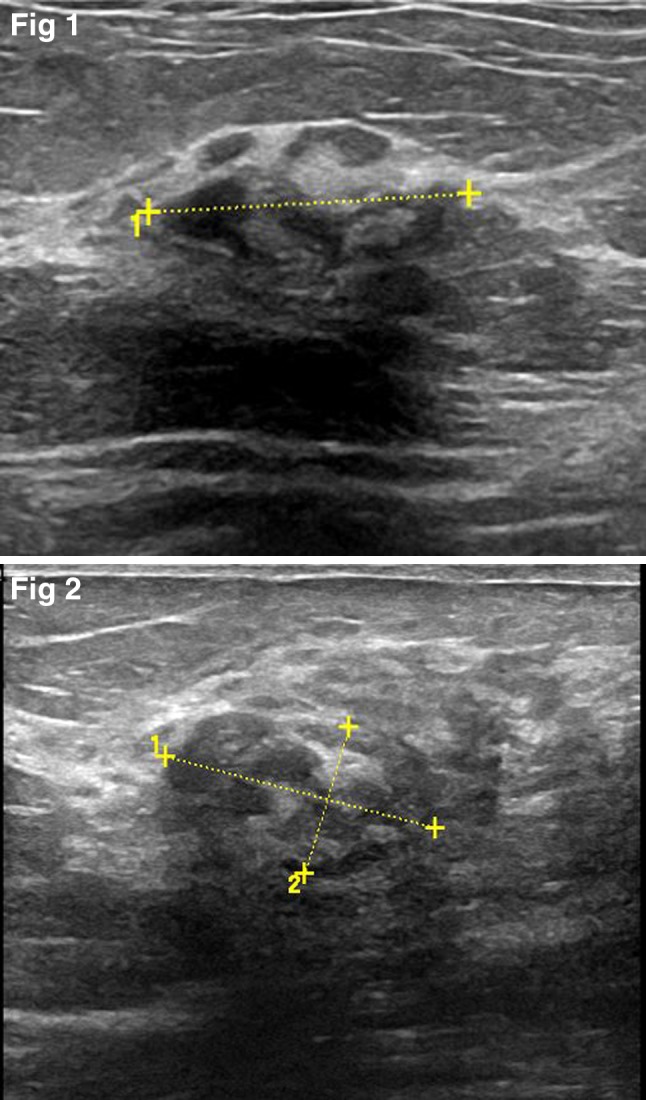
Data in the literature are limited on the specific elastographic characteristics of hamartomas, but their consistency and compressibility are known to depend on the amount of adipose tissue they contain, which is highly variable [5]. In most cases, the color pattern is indicative of a mass that is less elastic than the tissue that surrounds it. This pattern corresponds to an Italian elastosonographic score of 3 or 4 [6]. This appearance may depend on the amount of fibrous tissue present in hamartomas; in fact, the different tissues that make up the breast have distinct elastographic features, with fibrous and glandular tissues displaying greater stiffness than fat tissue [7, 8] (Figs. 4, 5, 6). The use of elastosonographic software can be helpful for defining the margins of the mass [9]. The success of elastographic assessment of hamartomas depends to some extent on their size: for optimal and reliable data collection, the mass must fit within the evaluation box. Hamartomas (and other lesions as well) that exceed the dimensions of the transducer are not suitable for elastographic studies, and such cases are by no means unusual.
Fig. 4–6.
On elastosonography, the color pattern of this hamartoma contains mainly blue and light blue, indicating that it is less elastic than the surrounding tissue (due to its relatively high content of fibrous tissue)
Mammographic Appearance
Hamartomas are typically seen on mammography as oval or round formations, which are inhomogeneous with radio-opaque and radiotransparent areas reflecting the presence of tissues that differ in density. They are well defined by a thin radio-opaque pseudocapsule. Owing to the presence of scattered nodular opacities within the radiotransparent fat tissue contained in the pseudocapsule, the mass typically resembles a slice of salami (Figs. 7, 8). The pseudocapsule is composed of breast parenchyma that has been displaced by the mass [5]. Hamartomas that contain relatively high amounts of fibrous tissue are homogeneously dense, and thus it may be difficult to differentiate them from fibroadenomas (Fig. 9). Those composed mainly of adipose tissue can mimic lipomas, foci of liponecrosis, or oil cysts [5]. The latter two lesions, however, are almost always associated with histories of surgery or other types of trauma, which can facilitate the differential diagnosis.
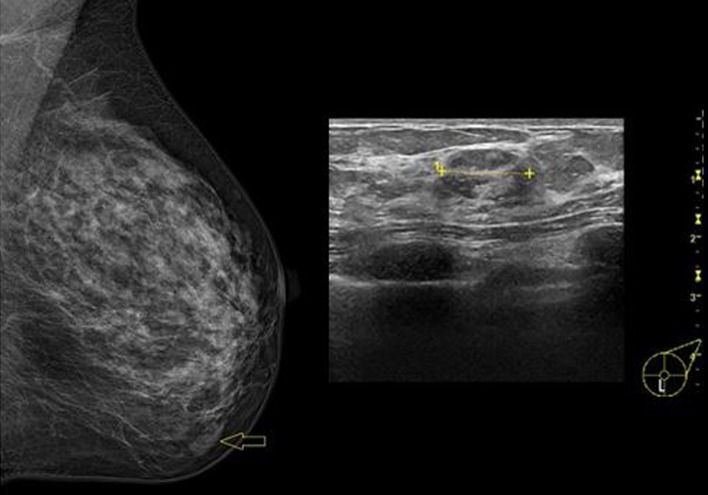
Fig. 7–8.
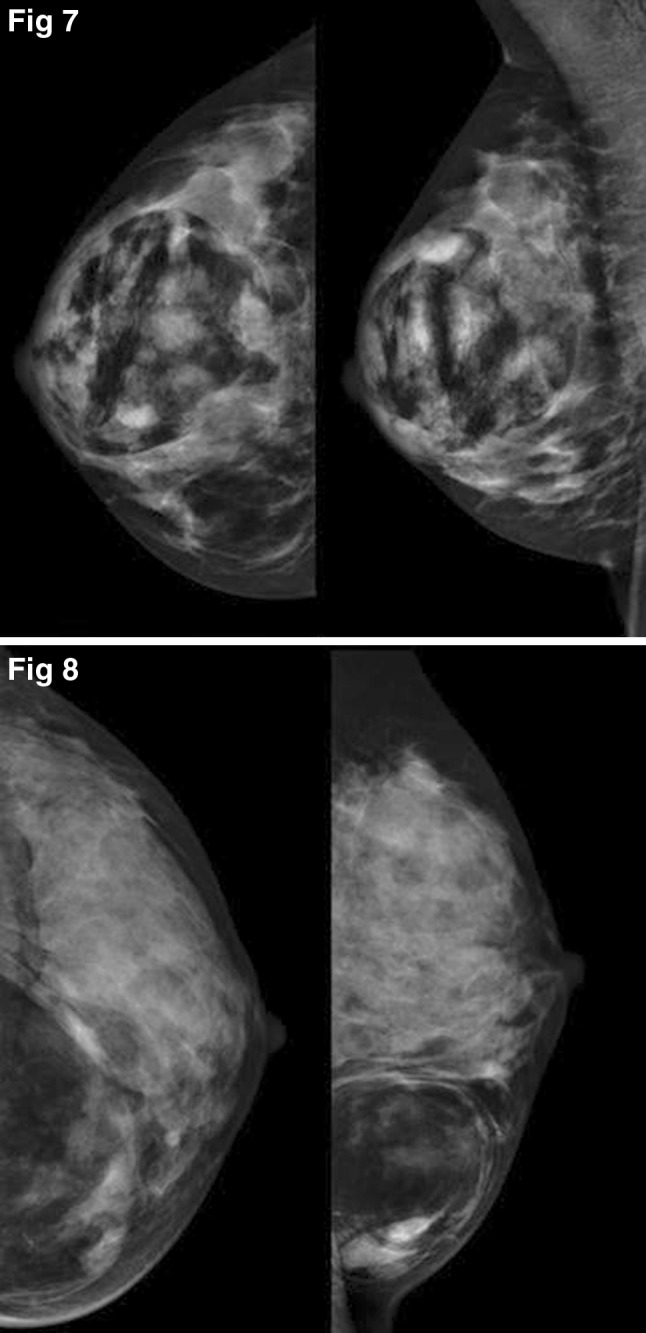
Typical appearance of a hamartoma on mammography: a well-defined mass containing a substantial amount of fat (radiotransparent) and fibroepithelial components (radio-opaque). The “slice of salami” appearance is shown in Fig. 7, while Fig. 8 provides better visualization of the pseudocapsule
Fig. 9.
Small hamartoma composed mainly of fibrous tissue: comparison of findings on mammography and ultrasound
Magnetic resonance
The presence of a typical breast hamartoma with no suspicious features on mammography or ultrasound is not an indication for MRI, although hamartomas may be discovered incidentally on MRI. On T1- and T2-weighted sequences, the mass generally exhibits heterogeneous signal intensity, reflecting the presence of glandular and adipose tissue components, and a thin capsule. After administration of contrast medium, hamartomas show a gradual, progressive enhancement with a type I time/intensity curve. The specific findings seen on diffusion-weighted sequences have not been reported. If suspicious features are noted, especially on mammography or ultrasound, contrast-enhanced MRI can be useful in establishing a diagnosis [10, 11].
Conclusions
Hamartomas are benign lesions, and when they present with typical findings on imaging studies, no further diagnostic procedures or follow-up are needed. The limited amount of data in the literature on the elastographic features of breast hamartomas indicates that they are usually less elastic than the surrounding tissues. In the presence of less typical findings on mammography or ultrasound, hamartomas may have to be differentiated from other lesions (e.g., fibroadenomas if they contain mainly fibrous tissue, lipomas when adipose tissue is predominant).
Malignant transformation of a hamartoma is a very rare event, but it can occur since the mass contains epithelial tissue. A fairly recent review of the literature [12] described 15 cases of carcinoma associated with hamartomas. In the majority of cases, the diagnosis was made as a result of mammographic or ultrasound findings of suspicious features within an otherwise typical hamartoma (specifically, microcalcifications or spiculated opacities on mammography, irregular hypoechoic lesions on sonography). In 2 cases, the presence of malignancy was discovered unexpectedly during pathological examination of a specimen removed during nodulectomy. Therefore, it is important to be able to recognize suspicious sonographic and mammographic features that may be present within a hamartoma.
In conclusion, most hamartomas have typical features on ultrasound and on mammography, which are related to the presence of fibrous, glandular, and adipose tissues. In rare cases, malignant transformation can occur as a result of cellular atypia in the epithelial component of the mass. It is therefore important to be able to recognize the sonographic and mammographic findings that should raise the suspicion of malignancy. The elastographic features of such lesions have yet to be described.
Compliance with ethical standards
Conflict of interest
The authors declare they have no conflicts of interest to disclose.
Informed Consent
The patient provided written informed consent to the inclusion of information that could potentially lead to her identification.
Human & Animal Studies
The case presented does not include any experimental procedures involving humans or animals.
References
- 1.Vergine M, Scipioni P, Santucci E, et al. Hamartoma of the breast in a young woman. Case report. Il Giornale di Chirurgia. 2013;34(5–6):161–163. doi: 10.11138/gchir/2013.34.5.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sonmez FC, et al. Hamartoma of the breast in two patients: a case report. Oncol Lett. 2013;6(2):442–444. doi: 10.3892/ol.2013.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sevim Y, et al. Breast hamartoma: a clinicopathologic analysis of 27 cases and a literature review. Clinics. 2014;69(8):515–523. doi: 10.6061/clinics/2014(08)03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farrokh D, H. Janbakhsh, Ansaripour E. Breast hamartoma: mammographic findings. Iran J Radiol. 2011;8(4):258–260. doi: 10.5812/iranjradiol.4492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masciadri N. Ferranti C benign breast lesions: ultrasound. J Ultrasound. 2011;14(2):55–65. doi: 10.1016/j.jus.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rizzatto G et al (2007) Real-time elastography of the breast in clinical practice-the Italian experience. Medix Hitachi Supplement, pp 12–15
- 7.Zhou J, Zhou C, Zhan W, Jia X, Dong Y, Yang Z. Elastography ultrasound for breast lesions: fat-to-lesion strain ratio vs gland-to-lesion strain lesion. Eur Radiol. 2014;24:3171–3177. doi: 10.1007/s00330-014-3366-8. [DOI] [PubMed] [Google Scholar]
- 8.Krouskop TA, Wheeler TM, Kallel F, Garra BS, Hall T. Elastic moduli of breast and prostate tissue under compression. Ultrason Imaging. 1998;20(4):260–274. doi: 10.1177/016173469802000403. [DOI] [PubMed] [Google Scholar]
- 9.Goddi A, Bonardi M, Alessi S. Breast elastography: a literature review. J Ultrasound. 2012;15(192e):198. doi: 10.1016/j.jus.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cucci E, Santoro A, Di Gesú C, Ciuffreda M, Maselli G, Pierro A, Sallustio G. Integrated imaging of breast hamartoma: two case reports. Breast Dis. 2015;35(1):53–57. doi: 10.3233/BD-140379. [DOI] [PubMed] [Google Scholar]
- 11.Erdem G, Karakaş HM, Işık B, Fırat AK. Advanced MRI findings in patients with breast hamartomas. Diagn Interv Radiol. 2011;17(1):33–37. doi: 10.4261/1305-3825.DIR.1892-08.2. [DOI] [PubMed] [Google Scholar]
- 12.Nami C, Eun SK. Invasive ductal carcinoma in a mammary hamartoma: case report and review of the literature. Korean J Radiol. 2010;11(6):687–691. doi: 10.3348/kjr.2010.11.6.687. [DOI] [PMC free article] [PubMed] [Google Scholar]