Abstract
Objectives
Infants are at high risk of developing chronic, life-threatening disease as a result of hepatitis B virus infection. Universal vaccination of infants against hepatitis B virus, before discharge from the hospital after delivery is recommended as a measure to eradicate infection and associated mortality and morbidity. The purpose of this study was to determine rates of perinatal hepatitis B vaccine (Hep B) administration at a tertiary care center in Iowa and to assess the impact of maternal factors on Hep B uptake.
Methods
Data concerning mother-infant pairs that received care at one institution from 1/2009-4/1/2013 were extracted from the system’s electronic medical record. Characteristics of study participants were compared using chi-square tests. Multivariate logistic regression was used to assess the association between each factor and vaccination status, controlling for other characteristics.
Results
Of 5,663 mother-infant pairs, 5,175 (91.4%) infants received Hep B within 7 days after delivery. The majority of those not vaccinated had a medical indication to delay vaccination. Single women were significantly more likely to have an infant not vaccinated, after adjustment for all other factors. Women of minority groups were significantly less likely to have an infant who lacked Hep B at hospital discharge than Caucasian women.
Conclusions
Significant improvements have occurred in Hep B rates in the state and region. Infants of single mothers may be at the greatest risk for lacking vaccination at hospital discharge.
Keywords: Hepatitis B Virus, Vaccination, Immunization, Infant Health
Introduction
The vaccination of newborn infants in the hospital with a hepatitis B vaccine (Hep B) is a principal element in The Advisory Committee on Immunization Practices’ (ACIP) strategy to eradicate hepatitis B virus (HBV) infection in the United States. The current recommendation, since 2005, is that all medically stable infants weighing ≥ 2,000g be vaccinated prior to hospital discharge. This recommendation is included in the 2013 recommended immunization schedule for persons age 0-18, supported also by the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and the American Congress of Obstetricians and Gynecologists (ACOG) (1).
Acute hepatitis B has the propensity to become a chronic infection and lead to cirrhosis of the liver and hepatocellular carcinoma (HCC). Infants, are at especially high risk; 90% or greater of those infected will develop chronic disease (2, 3). Infants are most likely to become infected by vertical transmission from the mother at the time of delivery or by horizontal transmission from any infected person, usually a person living in the home and/or coming into frequent contact with the infant (2, 3). Screening of all pregnant women for HBV infection (HbsAg-positive) is recommended. Prophylactic treatment with hepatitis B immune globulin (HBIG) is indicated for infants born to HbsAg-positive women and women whose HBV status is unknown. The administration of Hep B to all infants prior to discharge provides a secondary method of prevention for those infants who are not identified by the maternal screening process and protection from other contacts in the first weeks of life (1-4). Studies have found completion of a 3 or 4-dose schedule of Hep B vaccination without administration of HBIG ≤ 12 hours after delivery prevents 70% – 95% of HBV infections among infants whose mothers are infected (3). Additionally, administration of the first dose of Hep B after delivery, prior to discharge, has been shown to be associated with the completion of the recommended Hep B series during childhood (5).
The incidence of HBV in persons < 15 years of age decreased by 98%, from 1.2 cases per 100,000 in 1990 to 0.02 cases per 100,000 in 2007 (6). However, there remains room for improvement as perinatal HBV infections persist in the US. Reports by the CDC conclude that complete elimination of HBV will require improved preventive practices (2, 7). Thus, particularly in an era in which it is not uncommon for parents to refuse or delay vaccination for their children (8, 9), it is crucial to continue to monitor Hep B rates. The National Immunization Survey (NIS) estimated that, between 2003 and 2005, only 23.1% of infants born in Iowa were vaccinated with Hep B by day 3 of life, substantially lower than the national average of 50.1% during the same period (4). The primary purpose of this study was to identify maternal factors associated with lack of Hep B prior to hospital discharge after birth at a tertiary care center in the state of Iowa. This study also sought to determine current rates of perinatal Hep B administration to assess whether rates have increased since 2005.
Methods
Data Extraction
The University of Iowa Hospitals and Clinics (UIHC) is a tertiary referral center that performs high-risk deliveries and has a level IV neonatal intensive care unit (NICU). To collect data, programming was developed through collaboration with the Institute for Clinical and Translational Science (ICTS) at the University of Iowa that allowed review of de-identified, linked mother-baby records. Data was extracted from the records of every mother-baby pair in which the woman delivered at the UIHC from January 1, 2009 – April 1, 2013. Inclusion criteria required that the mother had at least one in-person encounter at one of 13 selected departments providing prenatal care within this healthcare system in the nine months prior to delivery.
Information extracted from the mother’s patient records included: the mother’s age, marital status, race, ethnicity, and insurance provider, all at the time of data extraction. Hep B vaccination - administration of the Hep B within 7 days of birth and prior to hospital discharge - was obtained from the infant’s hospital admission record. Although most infants are discharged by the third day of life - and thus would receive vaccination by DOL 3 as is recommended, because of the high acuity of many patients who deliver at this institution, data was collected on vaccination up to day of life (DOL) 7 to account for infants who had a slightly extended hospital stay and would have, appropriately, had vaccination later. Infants who got the vaccination on DOL 7 but as an outpatient were not considered compliant with ACIP recommendations. At the institution in question, in the absence of parental refusal, infants receive Hep B on DOL 60 or prior to discharge, whichever occurs first. Under circumstances when the mother’s HBV status is unknown, vaccination may be done as soon as possible once the infant is stabilized. Maternal data reported are from the time the data was extracted rather than date of delivery, thus some data may have changed slightly in the 1-3 year interval. This predominately affects maternal age data. This was necessary because in order to perform an anonymous data extraction, the date of delivery and the mother’s date of birth could not be known to investigators. Due to the large sample size of this study and the broad categories used for age group, marital status, and insurance type, this affects relatively few data sets and impact on the study was deemed to be minimal. A subsequent extraction and analysis were later performed, which did assess for impact of the date of delivery and proximity of the families residence to the hospital in question.
An electronic medical record review of 100 randomly selected mother-infant pairs in which the infant did not receive Hep B by DOL 7 and 100 randomly selected pairs in which the infant did receive Hep B by DOL 7 assessed for variables related to the infant’s health and disposition at the time of birth and DOL 7. The Institutional Review Board (IRB) of the University of Iowa Human Subjects Office approved all components of data extraction and analysis involved in this study (IRB # 201311711).
Statistical Analysis
Characteristics of the study participants were compared according to Hep B status (yes/no) using chi-square tests. Univariate logistic regression was used to assess the association between each demographic factor (maternal age, maternal race, maternal ethnicity, marital status, and type of health insurance) and vaccination status. Additionally, multivariate logistic regression was conducted for each of the demographic factors, controlling for the other four factors. All analyses were performed using SAS 9.3 (SAS Institute, Cary, NC, USA).
Results
A total of 5,663 mother-newborn pairs were included in this study. Characteristics of the study population are shown in Table 1. A total of 5,175 (91.4%) infants received Hep B prior to discharge and by DOL 7. The proportion of women whose infants received Hep B was similar across all maternal age groups. Caucasian and African-American women were the least likely to have infants who were vaccinated (90.5%) whereas Asian women were the most likely to have infants vaccinated (96.3%). Additionally, married women (92.7%) and those with employer or school-based health insurance (92.3%) were most likely to have an infant that received Hep B after birth. Results of the unadjusted and adjusted logistic regression analyses are presented in Table 2. Single women were significantly more likely to have an infant not vaccinated in the hospital after adjustment for age, race, ethnicity, and health insurance provider (aOR 1.72, 95% CI 1.35, 2.19) when compared to married women. No significant association was observed for maternal age or health insurance provider.
Table 1.
Characteristics of Women Whose Infants Received and Did Not Receive Hepatitis B Vaccination in the Hospital After Birth
| Infants That Were Vaccinated | Infants That Were Not Vaccinated | % Infants Vaccinated (95% CI) | p value | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| All Births (%) | n | % (95% CI) | n | % (95% CI) | |||
| Maternal Age Group | |||||||
|
| |||||||
| 15-20 | 149 (2.6) | 128 | 2.5 (2.1 - 2.9) | 21 | 4.3 (2.5 - 6.1) | 85.9 (80.3 - 91.5) | 0.06 |
| 21-30 | 2394 (42.3) | 2189 | 42.3 (41.0 - 43.7) | 205 | 42 (37.6 - 46.4) | 91.4 (90.3 - 92.5) | |
| 31-40 | 2796 (49.4) | 2567 | 49.6 (48.2 - 51.0) | 229 | 46.9 (42.5 - 51.3) | 91.8 (90.8 - 92.8) | |
| 41-53 | 324 (5.7) | 291 | 5.6 (5.0 - 6.2) | 33 | 6.8 (4.6 - 9.0) | 89.8 (86.5 - 93.1) | |
| TOTAL | 5663 (100) | 5175 | 100 | 488 | 100 | ||
|
| |||||||
| Marital Status | |||||||
|
| |||||||
| Married | 4016 (70.9) | 3721 | 71.9 (70.7 - 73.1) | 295 | 60.5 (56.2 - 64.8) | 92.7 (91.9 - 93.5) | < 0.0001 |
| Single | 1413 (25) | 1241 | 24 (22.8 - 25.2) | 172 | 35.3 (31.1 - 39.5) | 87.8 (86.1 - 89.5) | |
| Other | 234 (4.1) | 213 | 4.1 (3.6 - 4.6) | 21 | 4.3 (2.5 - 6.1) | 91 (87.3 - 94.7) | |
| TOTAL | 5663 (100) | 5175 | 100 | 488 | 100 | ||
|
| |||||||
| Race | |||||||
|
| |||||||
| Caucasian | 4189 (74) | 3789 | 73.2 (72.0 - 74.4) | 400 | 82 (78.6 - 85.4) | 90.5 (89.6 - 91.4) | < 0.0001 |
| African-American | 388 (6.9) | 351 | 6.8 (6.1 - 7.5) | 37 | 7.6 (5.3 - 10.0) | 90.5 (87.6 - 93.4) | |
| Hispanic | 409 (7.2) | 390 | 7.5 (6.8 - 8.2) | 19 | 3.9 (2.2 - 5.6) | 95.4 (93.4 - 97.4) | |
| Asian | 377 (6.7) | 363 | 7 (6.3 - 7.7) | 14 | 2.9 (1.4 - 4.4) | 96.3 (94.4 - 98.2) | |
| Other | 300 (5.3) | 282 | 5.5 (4.9 - 6.1) | 18 | 3.7 (2.0 - 5.4) | 94 (91.3 - 96.7) | |
| TOTAL | 5663 (100) | 5175 | 100 | 488 | 100 | ||
|
| |||||||
| Ethnicity | |||||||
|
| |||||||
| Non-Hispanic | 4398 (77.7) | 4041 | 78.1 (77.0 - 79.2) | 357 | 73.2 (69.3 - 77.1) | 91.9 (91.5 - 93.1) | <0.0001 |
| Hispanic | 336 (5.9) | 319 | 6.2 (5.5 - 6.9) | 17 | 3.5 (1.9 - 5.1) | 94.9 (92.6 - 97.3) | |
| Unknown | 929 (16.4) | 815 | 15.8 (14.8 - 16.8) | 114 | 23.4 (19.6 - 27.2) | 87.7 (85.6 - 89.8) | |
| TOTAL | 5663 (100) | 5175 | 100 | 488 | 100 | ||
|
| |||||||
| Health Insurance Status | |||||||
|
| |||||||
| Employer/School | 0.01 | ||||||
| Based | 2517 (44.5) | 2323 | 44.9 (53.4 - 46.3) | 194 | 39.8 (35.5 - 44.1) | 92.3 (91.3 - 93.3) | |
| State Assisted/VA | 817 (14.4) | 727 | 14.1 (13.2 - 15.1) | 90 | 18.4 (15.0 - 21.8) | 89 (86.9 - 91.2) | |
| None/None on File | 2329 (41.1) | 2125 | 41.1 (39.8 - 42.4) | 204 | 41.8 (37.4 - 46.2) | 91.2 (90.1 - 92.4) | |
| TOTAL | 5663 (100) | 5175 | 100 | 488 | 100 | ||
Table 2.
Odds of Infants Born within the University of Iowa Hospitals and Clinics healthcare system not receiving Hepatitis B Vaccination Prior to Hospital Discharge
| N | Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI)a | |
|---|---|---|---|
| Maternal Age Group | |||
| 15-20 | 149 | 1.00 (Ref) | 1.00 (Ref) |
| 21-30 | 2394 | 0.57 (0.35 - 0.93) | 0.67 (0.41 - 1.10) |
| 31-40 | 2796 | 0.54 (0.34 - 0.88) | 0.75 (0.45 - 1.26) |
| 41-53 | 324 | 0.69 (0.39 - 1.24) | 0.94 (0.51 - 1.75) |
|
| |||
| Marital Status | |||
| Married | 4016 | 1.00 (Ref) | 1.00 (Ref) |
| Single | 1413 | 1.75 (1.43 - 2.13) | 1.72 (1.35 - 2.19) |
| Other | 234 | 1.24 (0.78 - 1.98) | 1.25 (0.78 - 2.02) |
|
| |||
| Race | |||
| Caucasian | 4189 | 1.00 (Ref) | 1.00 (Ref) |
| African-American | 388 | 1.00 (0.70 - 1.42) | 0.78 (0.53 - 1.13) |
| Hispanic | 409 | 0.46 (0.29 - 0.74) | 0.29 (0.14 - 0.61) |
| Asian | 377 | 0.37 (0.21 - 0.63) | 0.41 (0.24 - 0.71) |
| Other | 300 | 0.61 (0.37 - 0.98) | 0.40 (0.24 - 0.67) |
|
| |||
| Ethnicity | |||
| Non-Hispanic | 4398 | 1.00 (Ref) | 1.00 (Ref) |
| Hispanic | 336 | 0.60 (0.37 - 0.99) | 1.55 (0.69 - 3.46) |
| Unknown | 929 | 1.58 (1.27 - 1.98) | 1.84 (1.45 - 2.35) |
|
| |||
| Health Insurance | |||
| Employer/School Based | 2517 | 1.00 (Ref) | 1.00 (Ref) |
| State Assisted/VA | 817 | 1.48 (1.14 - 1.93) | 1.11 (0.82 - 1.49) |
| None/Not on File | 2329 | 1.15 (0.94 - 1.41) | 0.99 (0.80 - 1.24) |
Univariate and multivariate regression models are modelling the outcome of no vaccination
Models adjusted for all other demographics in this table
Secondary extraction and analyses showed that infants born to women with a primary residence greater than 20 miles from the institution in question or outside of the state were significantly more likely to lack vaccination within 7 days of life (aOR of 3.21, 95% CI 2.55, 4.03 and 2.63, 95% CI 1.71, 4.04 respectively). This group may have delivered at this institution due to a high-risk status and have infants who were more likely to spend greater than 7 days in the hospital’s NICU, which does not vaccinate for Hep B until infants are stable and shortly before discharge and so this extraction did not identify them as receiving the vaccine. A randomized electronic record review of 200 mother-infant pairs (100 in which the infant received Hep B by DOL 7 and 100 in which the infant did not receive Hep B by DOL 7) revealed that 74% (95% CI 66.6,81.7) of those infants who did not receive Hep B by DOL 7, compared to 13% (95% CI 6.5, 18.5) of those infants that did receive Hep B by DOL 7, were either admitted or were deceased (4 infants) on the 7th day after delivery. Of the 70 infants who were inpatient, 1 infant remained in the mother-baby care unit while the other 69 were admitted to intensive care units.
The majority of infants admitted to intensive care units at this institution would not be considered stable enough to receive vaccination and/or would not meet the weight requirement of 2000g. These infants represent a group for which delay of vaccination would be indicated rather than due to parental decision or provider’s preference to delay vaccination. By extrapolating these results to the larger study population one can estimate that of the 488 infants to lack Hep B on DOL 7, 361 (74%) had a medical indication to delay vaccination and 127 infants (26%), or 2.24% of the total study population did not receive vaccination when it was medically indicated.
The relationship between maternal marital status and infant disposition (admission to the hospital vs. discharge) on DOL 7 was examined among the 200 patient sample used for electronic medical record review. Among all 200 infants, the odds of an infant that was admitted (or deceased) 7 days after delivery also having a single mother was 2.78 (p = 0.002). Among those infants who did not receive Hep B by DOL 7, the odds of an infant that was admitted having a single mother was 4.79 (p = 0.008). There was no significant association between infants’ disposition on DOL 7 and marital status among those infants that had received Hep B, OR 0.32 (p = 0.289).
Discussion
Overall Hep B Vaccination Rates
During the period from January 1, 2009 – April 1, 2013, a significant majority (91.4%) of newborns born at a Midwestern tertiary care center received the Hep B within 7 days after birth and prior to hospital discharge. Data suggests that 26% of those not vaccinated, or 2.24% of the entire study population, did not get vaccination in the setting of medical indication. The NIS found that of births 2003 – 2005, 42.8% and 52.5% of infants were vaccinated by day 1 and day 6 of life, respectively (4). However, in Iowa only 20.2% and 23.1% of infants were vaccinated by day 1 and day 3 respectively (4). Findings of the present study suggest that in-hospital Hep B rates within the state have increased dramatically. As shown in Figure 1, during the 2003-2005 study period, the incidence of acute, symptomatic hepatitis B in Iowa ranged from 0.6 – 1.1 cases per 100,000 population (average of 0.8 per 100,000). From 2009-2012, the incidence ranged from 1.2 (a ten-year high in 2009) to 0.4 cases per 100,000 population (average of 0.65). Though data is not sufficient to prove a correlation between vaccination rates of infants and disease incidence, this does demonstrate at positive association over time. Unfortunately data from 2013 and prevalence rates from the CDC were not available. It is important to consider also that the CDC estimates the actual number of acute cases of hepatitis B to be 6.5 times the number of reported cases (10).
Figure 1.
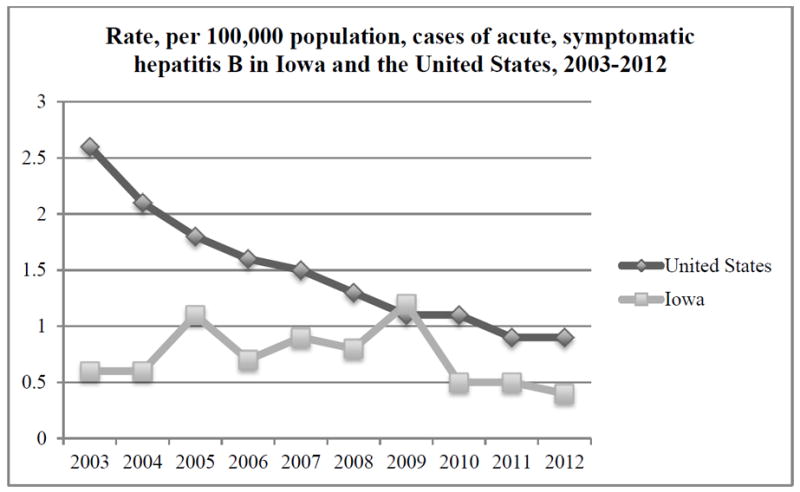
Data adapted from incidence reports of the Centers for Disease Control and Prevention Viral Hepatitis Statistics & Surveillance Program.
In 1999, in response to concerns raised by the US Food and Drug Administration (FDA) regarding the presence of the thimerosal and ethyl mercury in the vaccine, the AAP and the US Public Health Service (USPHS) issued a joint statement recommending healthcare providers postpone the birth-dose of Hep B. Within the same year, Hep B without thimerosal was available and the recommendation to postpone vaccination was lifted. An analysis of data from the NIS found that reductions in vaccination at birth persisted after this period (11). The findings of the present study suggest that hospitals and parents in Iowa were slow to return to vaccination at birth, but rates have now increased beyond the latest national estimates (4, 12).
To explain why 13% of those that did get Hep B vaccination in the electronic medical record review were still admitted on DOL 7, one probable explanation is that, though admitted, they were admitted to a low acuity neonatal intensive care unit and vaccination occurred as part of the preparation for discharge, as per NICU practices.
Impact of Maternal Marital Status
The odds that infants born to single women will lack Hep B upon hospital discharge were found to be nearly twice that of infants born to married women, after controlling for all other factors, including insurance provider. To the authors’ knowledge, this finding has not been previously documented. Repeated studies have documented an increased risk of preterm birth among single women (13). Single women referred to this institution for prenatal care and delivery may be more likely to have infants for whom it is medically indicated to delay vaccination with Hep B beyond the first week of life. The inclusion criteria that women in the study have had at least one prenatal visit at this institution limited the impact of this cofounding issue by excluding all those who were transferred only for impending preterm labor.
Why single women were less likely to have infants vaccinated with Hep B in the hospital remains unclear. Analysis of the electronic medical record review suggests that this observation can be partially explained by the phenomenon that single women are also more likely to deliver an infant that requires inpatient treatment for greater than 7 days. However, there may be other reasons single women are more likely to have unvaccinated infants also. As has been proposed an explanation for the higher risk of preterm birth among single women, these women may lack some of the social and emotional support of married women (13). The postpartum time is generally acknowledged as an overwhelming and stressful time for all parents. Single women in particular may struggle with the burden of yet another decision to make while they are in the hospital and, without a partner for emotional support, may lack confidence in their decisions. Therefore, single women may choose to defer vaccination until a later time.
Impact of Mothers’ Race & Ethnicity
Women who identified as Hispanic, Asian, or another racial group were significantly more likely than Caucasians to have infants that were vaccinated prior to discharge. No significant difference was found between African-Americans and Caucasians. The majority of past studies have found no significant impact of maternal race and ethnicity on likelihood of children’s Hep B or overall vaccination status (12, 14, 15). Caucasian women in this population may perceive their infants to be at low risk of coming into contact with the virus early during infancy. Likewise, it is possible that providers also view Caucasian women and their infants as low-risk and are, therefore, less insistent on the importance of vaccination for newborns. Women who are of a minority group (this population was 74% Caucasian) may perceive their own environments to convey a greater risk to the newborn or providers may perceive it as such. This theory is supported by the fact that infants with Asian mothers were the most likely to be vaccinated and those of Asian ancestry are documented to be at a greater risk for HBV exposure (16, 17).
Impact of Maternal Insurance Status
Importantly, no significant impact of presence or lack of health insurance or type of insurance was observed. Willis et al (12), who performed a nation-wide study, found that the most significant predictors of newborn vaccination were residence in a state with a policy to provide the newborn Hep B at no cost for those without insurance and delivery at a hospital with a written policy for universal Hep B vaccination at birth. The state of Iowa participates in the Vaccines for Children (VFC) program (a federal program that provides free vaccinations to children who are uninsured, underinsured, insured by Medicaid or American Indian or Alaska Native (18).
Impact of Maternal Age
The effect of maternal age on likelihood of infant Hep B was not found to be significant after controlling for other factors. Past studies have documented similar findings (11, 12). Education and income are cofounders for the impact of maternal age but the VFC program largely negates the impact of income. This may partially explain the lack of effect of maternal age observed.
Study Strengths and Limitations
Adding to the strength of this study is its large sample size. However, there are some important differences between the study population the rest of the state, which could hamper the study’s generalizability. In 2011, 87% of births in Iowa were among Caucasian women, while 74% in the women in the present study population were Caucasian. Supplemental Table 1 provides natality data from the state during the period of study. Though a limitation in the sense of generalizability, this is a strength in that it was possible to assess the Hep B rate in minority groups that are underrepresented in other hospitals across the state. The study site is a major tertiary care center for Eastern Iowa, and, therefore, women experiencing high-risk pregnancies or pregnancy complications, for which African-American’s are more susceptible, are referred to the hospital of study. Likewise, the study institution is located alongside a large undergraduate and graduate university. Thus, the local population is more urban and more diverse in terms of both race and socioeconomic status than the majority of the state.
Additionally, the present study did not assess for the influence of maternal education and data was not collected on which mothers were screened for HBV during pregnancy. Women who were screened and tested negative might have chosen to not vaccinate their infant, as their perceived threat was low.
Conclusions
A majority of infants born at a tertiary care center in Iowa are receiving Hep B within 7 days after birth and prior to discharge from the hospital. Most vaccinations likely occur within the first or second day of life as most healthy infants rarely remain in the hospital beyond this time. This study has documented substantial and important improvements in vaccination rates in this region from less than a decade previously (4). In order to eliminate HBV, universal vaccination must remain the goal. Providers need to remain vigilant of vaccine uptake, particularly for infants of single mothers. For families who may perceive their newborns to be at low risk, education on the resilience of the virus in the environment and the severity of illness among newborns may make a meaningful impact. Also, education for providers on the risks of perinatal HBV infection and the evidence supporting vaccination at birth should remain a priority of public health and training programs. Future research in this area should investigate how perceptions of risk impact parents’ and providers’ decisions about vaccines. Additionally, surveillance of vaccine uptake in more rural parts of the state and region are important to insure that professional guidelines are followed outside of large teaching hospitals and healthcare systems such as the one involved in this study.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the contribution of Monika Ahuja, Lead Database Administrator for the Institute for Clinical and Translational Science at the University of Iowa. The authors would also like to acknowledge the efforts of Nancy Weathers, Leigh McDonald and Allison Momany for their assistance with data collection. Compensation was provided to all those who made contributions to this study but who are not authors.
Sources of Funding and Support: The Institute for Clinical and Translational Science at the University of Iowa is supported by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant 2 UL1 TR000442-06. The CTSA program is led by the NIH’s National Center for Advancing Translational Sciences (NCATS). This publication's contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention. Advisory Committee on Immunization Practices (ACIP) Recommended Immunization Schedules for Persons Aged 0 Through 18 Years and Adults Aged 19 Years and Older — United States, 2013. Morbidity and Mortality Weekly Report. 2013;62:1–19. [PubMed] [Google Scholar]
- 2.Shepard CW, Finelli L, Fiore AE, Bell BP. Epidemiology of hepatitis B and hepatitis B virus infection in United States children. Pediatr Infect Dis J. 2005;24(9):755–60. doi: 10.1097/01.inf.0000177279.72993.d5. [DOI] [PubMed] [Google Scholar]
- 3.Mast EE, Margolis HS, Fiore AE, Brink EW, Goldstein ST, Wang SA, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1: immunization of infants, children, and adolescents. MMWR Recomm Rep. 2005;54(RR-16):1–31. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Newborn hepatitis B vaccination coverage among children born January 2003-June 2005--United States. MMWR Morb Mortal Wkly Rep. 2008;57(30):825–8. [PubMed] [Google Scholar]
- 5.Yusuf HR, Daniels D, Smith P, Coronado V, Rodewald L. Association between administration of hepatitis B vaccine at birth and completion of the hepatitis B and 4:3:1:3 vaccine series. JAMA. 2000;284(8):978–83. doi: 10.1001/jama.284.8.978. [DOI] [PubMed] [Google Scholar]
- 6.Daniels D, Grytdal S, Wasley A. Centers for Disease C, Prevention. Surveillance for acute viral hepatitis - United States, 2007. MMWR Surveill Summ. 2009;58(3):1–27. [PubMed] [Google Scholar]
- 7.Smith EA, Jacques-Carroll L, Walker TY, Sirotkin B, Murphy TV. The national Perinatal Hepatitis B Prevention Program, 1994-2008. Pediatrics. 2012;129(4):609–16. doi: 10.1542/peds.2011-2866. [DOI] [PubMed] [Google Scholar]
- 8.Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(Suppl 2):135–46. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bardenheier B, Yusuf H, Schwartz B, Gust D, Barker L, Rodewald L. Are parental vaccine safety concerns associated with receipt of measles-mumps-rubella, diphtheria and tetanus toxoids with acellular pertussis, or hepatitis B vaccines by children? Arch Pediatr Adolesc Med. 2004;158(6):569–75. doi: 10.1001/archpedi.158.6.569. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. [2015 February 1];Viral Hepatitis Statistics & Surveillance. [updated August 28, 2014] Available from: http://www.cdc.gov/hepatitis/Statistics/index.htm.
- 11.Luman ET, Fiore AE, Strine TW, Barker LE. Impact of thimerosal-related changes in hepatitis B vaccine birth-dose recommendations on childhood vaccination coverage. JAMA. 2004;291(19):2351–8. doi: 10.1001/jama.291.19.2351. [DOI] [PubMed] [Google Scholar]
- 12.Willis BC, Wortley P, Wang SA, Jacques-Carroll L, Zhang F. Gaps in hospital policies and practices to prevent perinatal transmission of hepatitis B virus. Pediatrics. 2010;125(4):704–11. doi: 10.1542/peds.2009-1831. [DOI] [PubMed] [Google Scholar]
- 13.Behrman RE, Butler AS, editors. Preterm Birth: Causes, Consequences, and Prevention. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC): 2007. [PubMed] [Google Scholar]
- 14.Hurie MB, Saari TN, Davis JP. Impact of the Joint Statement by the American Academy of Pediatrics/US Public Health Service on thimerosal in vaccines on hospital infant hepatitis B vaccination practices. Pediatrics. 2001;107(4):755–8. doi: 10.1542/peds.107.4.755. [DOI] [PubMed] [Google Scholar]
- 15.Luman ET, McCauley MM, Shefer A, Chu SY. Maternal characteristics associated with vaccination of young children. Pediatrics. 2003;111(5 Pt 2):1215–8. [PubMed] [Google Scholar]
- 16.Strong C, Lee S, Tanaka M, Juon HS. Ethnic differences in prevalence and barriers of HBV screening and vaccination among Asian Americans. J Community Health. 2012;37(5):1071–80. doi: 10.1007/s10900-012-9541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu KQ. Hepatitis B virus (HBV) infection in Asian and Pacific Islander Americans (APIAs): how can we do better for this special population? Am J Gastroenterol. 2008;103(7):1824–33. doi: 10.1111/j.1572-0241.2008.01878.x. [DOI] [PubMed] [Google Scholar]
- 18.Iowa Department of Public Health. Bureau of Immunization & TB Des Moines. [2013 November 6];IA2013. Available from: http://www.idph.state.ia.us/immtb/Immunization.aspx?prog=Imm&pg=Vfc.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


