Abstract
Epitopes on the surface of the foot-and-mouth disease virus (FMDV) capsid have been identified by monoclonal antibody (mAb) escape mutant studies leading to the designation of four antigenic sites in serotype A FMDV. Previous work focused on viruses isolated mainly from Asia, Europe and Latin America. In this study we report on the prediction of epitopes in African serotype A FMDVs and testing of selected epitopes using reverse genetics. Twenty-four capsid amino acid residues were predicted to be of antigenic significance by analysing the capsid sequences (n = 56) using in silico methods, and six residues by correlating capsid sequence with serum–virus neutralization data. The predicted residues were distributed on the surface-exposed capsid regions, VP1–VP3. The significance of residue changes at eight of the predicted epitopes was tested by site-directed mutagenesis using a cDNA clone resulting in the generation of 12 mutant viruses involving seven sites. The effect of the amino acid substitutions on the antigenic nature of the virus was assessed by virus neutralization (VN) test. Mutations at four different positions, namely VP1-43, VP1-45, VP2-191 and VP3-132, led to significant reduction in VN titre (P value = 0.05, 0.05, 0.001 and 0.05, respectively). This is the first time, to our knowledge, that the antigenic regions encompassing amino acids VP1-43 to -45 (equivalent to antigenic site 3 in serotype O), VP2-191 and VP3-132 have been predicted as epitopes and evaluated serologically for serotype A FMDVs. This identifies novel capsid epitopes of recently circulating serotype A FMDVs in East Africa.
Introduction
Foot-and-mouth disease (FMD) is a highly infectious, rapidly spreading and internationally important livestock disease. It has significant socio-economic consequences due to losses in production and constraints on export of live animals and associated products to disease-free countries. FMD is caused by FMD virus (FMDV) that belongs to the family Picornaviridae, genus Aphthovirus. The virus exists as seven distinct serotypes (A, O, C, Asia1, South African Territory (SAT)-1, SAT-2 and SAT-3) that differ genetically and antigenically with multiple strains in different continents. Globally, most outbreaks of FMD are caused by serotype O followed in frequency by serotype A (Rweyemamu et al., 2008; Chitray et al., 2014; Wekesa et al., 2014), which is endemic in many developing countries of Africa and Asia. FMDV serotype A continues to cause outbreaks in East Africa (Bari et al., 2014; Wekesa et al., 2014). It is a small, non-enveloped virus containing a single-stranded positive-sense RNA genome. The genome has a single ORF that encodes four capsid (structural) proteins and 10 non-structural proteins (Grubman & Baxt, 2004). As an RNA virus, it is characterized by the frequent emergence of new variants responsible for recurring disease outbreaks.
The genetic heterogeneity of the FMDV arises from lack of proofreading mechanisms during virus replication resulting in new variants, including those with changes in antigenically important sites of the virus (VP1-3) that may improve viral fitness. These sites are commonly investigated in vitro by epitope mapping using mAb (Thomas et al., 1988; Bolwell et al., 1989; Kitson et al., 1990; Crowther et al., 1993; Mateu et al., 1995; Mahapatra et al., 2011; Grazioli et al., 2013). Four antigenic sites (equivalent to sites 1, 2, 4 and 5 of serotype O) were described for serotype A; site 1 (G-H loop of VP1) is linear and trypsin-sensitive, whereas the others are conformational and trypsin-resistant (Thomas et al., 1988; Bolwell et al., 1989; Saiz et al., 1991; Mahapatra et al., 2011). Escape mutants are also studied using polyclonal antibodies in serotypes O and C (Rojas et al., 1992; Schiappacassi et al., 1995; Kumar et al., 2004; Sarangi et al., 2013). In addition, the location of antibody binding sites (epitopes) can be inferred from correlating the antibody cross-reactivity of viruses to their capsid sequence similarities (Reeve et al., 2010).
Epitopes can also be predicted from three-dimensional (3D) structural data alone, from aligned sequence data alone, or by using both sequence data and three-dimensional structural data. More than 90 % of B-cell epitopes are conformational (Barlow et al., 1986), where distantly located residues on a sequence come together during protein folding, and prediction of these epitopes is better performed by combining structural and sequence information. Various structure-based epitope prediction programs are available freely (Rubinstein et al., 2009; Kringelum et al., 2012; Qi et al., 2014). DiscoTope (Kringelum et al., 2012), for example, uses a combination of statistical difference in amino acid composition between epitope and non-epitope residues, structural proximity and physico-chemical properties of neighbourhood amino acids, and a surface measure. All structure-based methods retrieve data from the protein database (PDB) file and conduct blast searches for closely related sequences. DiscoTope, Epitopia and SEPPA were recently applied to FMDV epitope prediction by Borley et al. (2013).
The importance of predicted residues for antibody binding can be tested by introducing specific mutations into a cDNA clone of the virus of interest. This approach is widely applied in emerging virus investigations including those into influenza (Yang et al., 2013), FMDV (Blignaut et al., 2011; Asfor et al., 2014; Opperman et al., 2014) and human immunodeficiency virus type 1 (HIV-1) (Evans et al., 2014).
Epitopes of many FMDV serotype A strains originating from Asia, Europe and Latin America are well characterized using monoclonal antibody resistant (mar) studies (Thomas et al., 1988; Baxt et al., 1989; Saiz et al., 1991; Mahapatra et al., 2011). However, there are no reports for analysis of epitopes using serotype A isolates originating from East Africa. In this study, we studied viruses from East Africa and report prediction of epitopes, including amino acid residues not reported previously for serotype A viruses. Eight of the predicted epitopes were tested using a cDNA clone and their antigenic impact was assessed by virus neutralization (VN) test, revealing neutralizing epitopes at positions VP1-43, -45, VP2-191 and VP3-132.
Results and Discussion
Antibodies play an important role in conferring protection against FMDV, including the protective effect of vaccination (Pay and Hingley, 1987; McCahon et al., 1989), which is derived from antibodies directed towards the surface of the inactivated capsids. Identification of the epitopes and understanding their immunodominance in antigenically and genetically diverse FMDVs is of utmost importance for vaccine strain selection and novel vaccine development to achieve adequate protection against the disease (Doel, 1996; Paton et al., 2005; Parida, 2009).
Epitope prediction
Studies on the critical amino acid residues for neutralization of serotype A FMDV have used mainly mar-mutant approaches with viruses from the Middle East (A22) (Bolwell et al., 1989), India (A/IND/17/77) (Tosh et al., 1999), Europe [A5 (Saiz et al., 1991), A10 (Thomas et al., 1988), A12 (Baxt et al., 1989)] and South America (A24) (Mahapatra et al., 2011). Consequently, there is no information available on the epitopes present on the serotype A viruses isolated from Africa. Therefore, as an initial step, we analysed a collection of East African serotype A viruses (i) by using two freely available software programs to predict epitopes from capsid amino acid sequences with and without structural information [in this case, the A1061 PDB file (1ZBE)] and (ii) by correlating differences in neutralizing serum titres between virus pairs with capsid amino acid sequence changes.
Epitopes predicted by in silico methods.
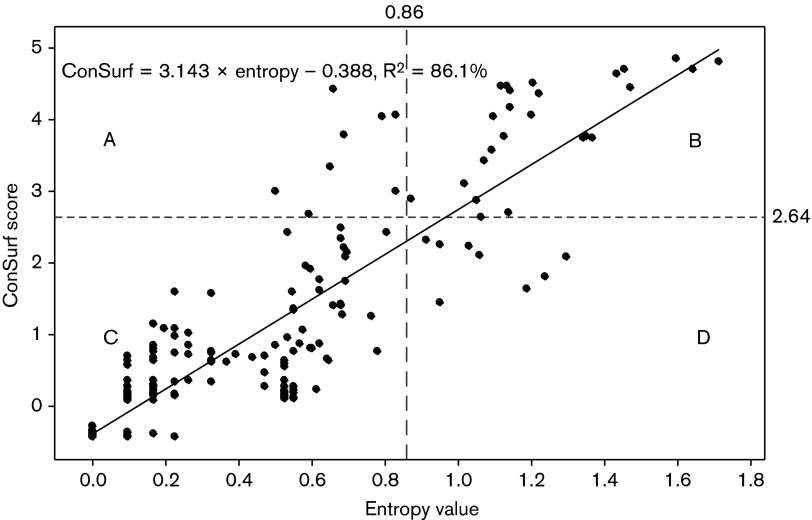
The results of Shannon entropy and ConSurf analysis are presented in Table 1. High Shannon entropy signifies amino acid variability and high values have been reported for variable epitopes in HIV (Liu et al., 2013; Evans et al., 2014), influenza (Pan & Deem, 2011) and neutralization escape FMD viruses (Piatti et al., 1995; Maree et al., 2011). In Shannon entropy analysis, use of a threshold of 0.86 (half of the highest score) resulted in the selection of 33 candidate amino acid residues to be of antigenic significance.
Table 1. List of capsid amino acid residues and their scores from entropy and ConSurf analysis.
Amino acids are arranged according to their order in the P1 sequence. The predicted amino acid residues are mostly located close to known epitopes except for residue VP2-191 that is 5 aa apart from VP2-196. nr, No reference antigenic site reported; GHL, VP1 G-H loop.
| P1 position | Viral protein (VP) | VP position | Entropy value | ConSurf score | Epitope reported previously | Residue located on external surface |
| 159 | 2 | 74 | 1.1 | 3.985 | nr | Yes |
| 163 | 2 | 78 | 1.156 | 4.458 | nr | Yes |
| 171 | 2 | 86 | 1.183 | 4.472 | nr | Yes |
| 173 | 2 | 88 | 0.867 | 3.644 | nr | Yes |
| 218 | 2 | 133 | 1.37 | 4.662 | nr | Yes |
| 219 | 2 | 134 | 1.704 | 4.802 | 134 | Yes |
| 276 | 2 | 191* | 1.627 | 4.789 | nr | Yes |
| 292 | 2 | 207 | 1.018 | 3.65 | nr | No |
| 338 | 3 | 35 | 0.988 | 3.523 | nr | No |
| 373 | 3 | 70 | 1.031 | 4.541 | 70 | Yes |
| 374 | 3 | 71 | 1.348 | 5.29 | 71 | Yes |
| 434 | 3 | 131* | 0.931 | 3.074 | nr | Yes |
| 523 | 3 | 220* | 1.25 | 5.034 | nr | Yes |
| 566 | 1 | 42 | 1.096 | 2.529 | nr | Yes |
| 567 | 1 | 43* | 1.222 | 2.996 | nr | Yes |
| 568 | 1 | 44* | 1.42 | 3.555 | nr | Yes |
| 569 | 1 | 45* | 1.554 | 3.861 | nr | Yes |
| 623 | 1 | 99 | 1.585 | 4.287 | nr | Yes |
| 625 | 1 | 101 | 1.078 | 2.38 | nr | Yes |
| 663 | 1 | 139 | 1.177 | 2.855 | 139 | GHL |
| 666 | 1 | 142 | 1.185 | 2.915 | 142 | GHL |
| 673 | 1 | 149 | 1.263 | 3.132 | 149 | GHL |
| 721 | 1 | 197 | 1.484 | 3.783 | nr | Yes |
| 722 | 1 | 198 | 1.343 | 3.3 | 198 | Yes |
Residues selected for site-directed mutagenesis study.
The highest antigenicity score in ConSurf was 5.29 and the top scoring 33 amino acid positions were compared with the entropy prediction results. Out of these, 24 were selected by both methods showing good agreement (86 %) between the two prediction methods (Fig. 1). All the 24 predicted residues were located on the outer surface of the virus capsid (Fig. 2b) except two residues, VP2-207 and VP3-35, which were internal (Fig. 2c). Eleven, eight and five predicted residues are present in VP1, VP2 and VP3, respectively (Table 1). Out of these, seven (29.2 %) have been previously reported in serotype A viruses; VP1-139/141/142, -149 (Thomas et al., 1988), VP1-198 (Saiz et al., 1991), VP3-70 (Thomas et al., 1988) and VP2-134 were reported to be of antigenic significance in serotype A viruses previously (Saiz et al., 1991) or to influence mAb binding in serotype O (Mahapatra et al., 2008). Previously, in silico epitope predictions performed using the A1061 crystal structure identified six (VP1-196/197/198, VP2-191 and VP3-70/71) of the 24 residues (Borley et al., 2013). Because ConSurf predicts epitopes with reference to the 3D structure and also by comparing evolutionary conservation rates of the aligned amino acid sequences, it is expected that it might provide more specific predictions of epitopes than would entropy analysis. Accordingly, ConSurf selected VP1-148 (data not shown), a neutralizing conformational epitope reported earlier for serotype A (Mahapatra et al., 2011).
Fig. 1. Scatter plot of Shannon entropy and ConSurf values showing areas of concordant high values (top right box, B) corresponding to the 24 commonly predicted amino acids. The cut-off values are indicated by black dotted lines. The high R2 value (86.1 %) indicates good correlation of the two prediction results. The graph was drawn using Minitab V.16 statistical software.
Fig. 2. A1061 (1ZBE) structure showing (a) the critical residues of reported epitopes; epitopes predicted in this study (b) external surface, (c) internal surface. Red, green and blue colours indicate residues in VP1, VP2 and VP3, respectively.
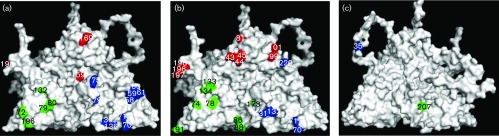
This is the first report, to our knowledge, to predict that residues at VP1-43/44/45 could have potential antigenic significance in serotype A FMDV. In addition, the neighbouring residue VP1-46 is also highly variable and together they form a cluster of residues on the capsid surface. Many of the previously identified regions of high amino acid variability on the P1 sequence of serotypes A and O FMDVs correspond to known antigenic sites and these positions are conserved structurally between the two serotypes (Fry et al., 2005; Chitray et al., 2014). This region corresponds to antigenic site 3 in serotype O (Kitson et al., 1990). In serotype O the stability of antigenic site 3 has been considered important for the stability of the VP1 G-H loop, and any destabilization in VP1 residues 43 to 45 may distort the conformation of the flexible VP1 G-H loop (Fry et al., 2005). Opperman et al. (2014) also recently reported the binding of monoclonal antibodies to closely located residues VP1-48 to -50 in the SAT2 serotype of FMDV. In addition, both ConSurf and entropy analysis predicted VP1-99 and -101 to be of antigenic significance whilst VP1-110 was predicted by entropy analysis only. A recent study in SAT2 FMDVs also suggested the presence of epitopes at VP1-109 and -111 (Opperman et al., 2014). In VP2, of the eight residues predicted by both methods only two (VP2-134 and VP2-191) were indicated to be of antigenic significance. The remaining six residues were newly predicted (Table 1) in silico to be of antigenic importance but their relevance so far could not be confirmed by other methods. The amino acid at position VP2-191 is located at the threefold axis of the capsid and is among the top four amino acids predicted by both in silico methods. This residue has been recently reported to be a neutralizing epitope linked to antigenic site 2 in serotype O FMDV (Asfor et al., 2014). In VP3, a total of five residues were predicted of which three (35, 71 and 131) were newly predicted. VP3-70 was previously reported by mar-mutant studies (Thomas et al., 1988). Recently, VP3-220 has been indicated to be of antigenic significance in serotype A viruses (Upadhyaya et al., 2014) and is located close to other newly predicted residues (VP1-99 and VP1-101) on the outer surface of the capsid (Fig. 2b).
Epitopes predicted by correlating sequence and serology data.
A total of six residues were predicted as epitopes by correlating serum titres and changes in capsid amino acid sequences, namely residues VP1-81, -138, -148 and -159, VP2-79 and VP3-132. Of these, four residues, VP1-138, -159 (Thomas et al., 1988), VP1-148 (Mahapatra et al., 2011) and VP2-79 (Saiz et al. 1991), were reported previously using mar-mutant studies or are within the VP1 G-H loop. Though VP3-135 has been reported by mar-mutant studies in SAT1 virus (Grazioli et al., 2006), residues VP1-81 and VP3-132 have not been reported previously in serotype A viruses and were good candidates for further investigation using a cDNA clone.
Among all the epitopes predicted by the in silico methods, residue VP2-191 was among the top four predicted epitopes and has not been reported previously by mar-mutant studies. VP1-43, -44 and -45, equivalent to antigen site 3 in serotype O virus, was predicted by both the in silico methods and was therefore selected for further investigation. In addition, the epitopes at VP1-81 and VP3-132 uniquely predicted by correlating sequence and serology data were taken forward for further investigation. VP3-131 predicted by ConSurf is located next to VP3-132 on the external surface and was taken forward for further investigation. VP3-220 predicted by both the in silico methods was also selected for further investigation.
Generation of full-length genome plasmids
The capsid-coding region of serotype A FMDV (A-EA-2007) was cloned successfully into the plasmid pT7S3-O1Kwt to generate the full-length genome plasmid pT7S3/A-EA-2007. This plasmid was used as the template to introduce further mutations in the capsid-coding region. A total of eight residues (VP1-43, -44, -45, -81, VP2-191 and VP3-131, -132, -220) were selected for this purpose as they were indicated to have an impact on the antigenicity of the virus by comparison of capsid sequences with in vitro virus cross-neutralization data or by epitope prediction using capsid sequence and viral crystal structure, and were novel (not reported previously). A total of 12 single mutant plasmids involving seven residues were generated (Table 2). The capsid coding regions of all the plasmids were sequenced on both strands and no unwanted mutations were observed.
Table 2. List of O1K/A-EA-2007 mutant viruses generated in this study and their associated amino acid substitutions.
Positions different from rO1K/A-EA-2007 are shaded.
| Virus | Capsid amino acid substitutions | ||||||
| VP1 | VP2 | VP3 | |||||
| 43 | 44 | 45 | 191 | 131 | 132 | 220 | |
| rO1K/A-EA-2007 | N | S | L | T | E | T | Q |
| rO1K/A-EA-2007M1 | A | S | L | T | E | T | Q |
| rO1K/A-EA-2007M2 | N | A | L | T | E | T | Q |
| rO1K/A-EA-2007M3 | N | P | L | T | E | T | Q |
| rO1K/A-EA-2007M4 | N | S | P | T | E | T | Q |
| rO1K/A-EA-2007M5 | N | S | L | A | E | T | Q |
| rO1K/A-EA-2007M6 | N | S | L | D | E | T | Q |
| rO1K/A-EA-2007M7 | N | S | L | T | A | T | Q |
| rO1K/A-EA-2007M8 | N | S | L | T | D | T | Q |
| rO1K/A-EA-2007M9 | N | S | L | T | E | A | Q |
| rO1K/A-EA-2007M10 | N | S | L | T | E | S | Q |
| rO1K/A-EA-2007M11 | N | S | L | T | E | T | A |
| rO1K/A-EA-2007M12 | N | S | L | T | E | T | T |
Rescue and characterization of recombinant viruses from full-length genome plasmids
Live infectious viruses were recovered successfully from all the cDNA clones following electroporation. FMDV-specific cytopathic effect (CPE) was observed 18–24 h post-electroporation. Extensive CPE was observed at both the first and second passages. At least two independent clones of each virus were rescued. However, only one clone in each case was used for further characterization. In order to establish that the expected viruses had been rescued, reverse transcription (RT)-PCR was carried out on the RNA extracted from infected BHK-21 cells using primer pair L460F and EUR2B52R/NK72 that produced a 2500 bp fragment (encompassing C-terminal part of L, P1, 2A and N-terminal part of 2B) of expected size (data not shown). No PCR products were generated in parallel reactions in which the enzyme reverse transcriptase was omitted, indicating that the products amplified were not generated from the transfected plasmid DNA. The PCR products were sequenced on both the strands and no additional nucleotide substitutions were observed in any of the mutants generated in this study.
The parent virus A-EA-2007 represents genotype VII of serotype A FMDV circulating in East Africa. Previously, chimeric viruses containing capsid-coding regions derived from serotype A/Turkey 2/2006 or O/UKG/34/2001 FMDV with the backbone of serotype O1K cDNA clone (pT7S3-O1K) have been generated successfully (Bøtner et al., 2011). These chimeric viruses retained the characteristics (in terms of receptor utilization, antigenicity, pathogenicity, etc.) from the parent from which the capsid was derived. In addition, successful switching of capsids from other serotypes of FMDV for the purpose of recombinant vaccine development and evaluation has been reported (van Rensburg et al., 2004; Blignaut et al., 2011; Zheng et al., 2013).
The mutants were stable genetically at least up to third passage as confirmed by full capsid sequencing. Standard multi-step growth curves were carried out to compare the growth of the recombinant viruses with that of the parent virus. All the viruses grew at a similar rate and to a similar titre, indicating the mutations in the antigenic sites had no adverse effects on the replication efficiency of these viruses in vitro (Fig. S1, available in the online Supplementary Material). The ability of FMDVs to tolerate changes at these positions is consistent with the observation of high amino acid variability at these residue positions in the 115 field viruses analysed [56 sequences reported before those of Bari et al. (2014) and the remaining 59 sequences downloaded from GenBank; data not shown]. BHK-21 cells infected with the parent or recombinant viruses were stained following infection and photographed. Both the parent and the recombinant viruses exhibited variable size plaques with no clear differences between them (data not shown). This corroborates the findings in a recent study of serotype O FMD mutant viruses (Seago et al., 2012; Lawrence et al., 2013; Asfor et al., 2014).
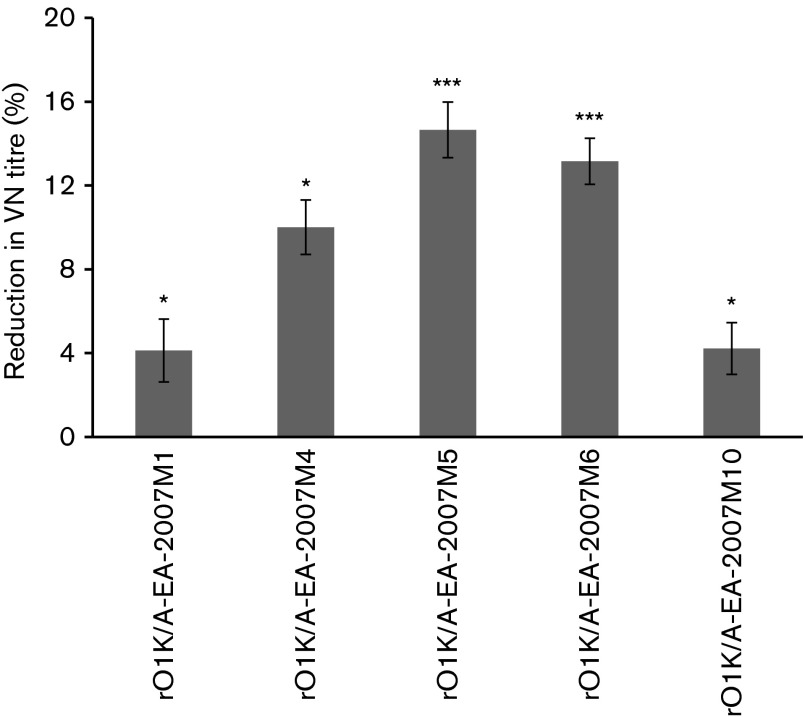
Serological reactivity of rO1K/A-EA-2007 mutant viruses
The impact of the amino acid substitutions on sero-reactivity was assessed by VN test using the pooled post-vaccination serum (bovine) raised against rO1K/A-EA-2007 antigen. The main goal was to quantify the reduction in neutralization following mutations in the capsid of FMDV. Therefore, it was crucial to determine the VN titre of the sera against all the mutant viruses at a fixed virus dose (100 TCID50). Therefore, a two-dimensional micro-neutralization test (2D-VNT) was carried out using five different doses of the virus encompassing 100 TCID50 for this purpose. The resultant VN titres at each virus dose were used to calculate the serum titre at 100 TCID50 by regression analysis. Because getting consistent results was very important for the evaluation of the mutant viruses, each test was conducted in duplicate and repeated at least eight times. Test results showing evidence of a reduction in serum titre after mutagenesis were repeated eight more times for further confirmation. Among the 12 mutants generated in this study, only five mutants, i.e. rO1K/A-EA-2007M1 (VP1-L43A), rO1K/A-EA-2007M4 (VP1-L45P), rO1K/A-EA-2007M5 (VP2-T191A), rO1K/A-EA-2007M6 (VP2-T191D) and rO1K/A-EA-2007M10 (VP3-T132S), exhibited significant reductions in serum titre (Fig. 3). The substitution of threonine at VP2-191 to alanine or aspartic acid exhibited relatively greater (15 % and 12.5 %, respectively) reductions in serum titre as compared with the parent virus. This agrees with the report of Crowther et al. (1993) who reported ~15 % reduction in serum titre as a result of a single amino acid change. In line with this, recently, Asfor et al. (2014) evaluated this epitope for serotype O FMDV using a cDNA clone and reported ~ 30 % reduction in serum titre. Hence this residue could represent a novel epitope across several serotypes. The residues VP1-43 to -45 are in an equivalent position to antigenic site 3 in serotype O (Kitson et al., 1990). Though mar-mutant studies have been carried out in several type A viruses, this region has never been reported to be of antigenic significance. However, VP1-45 has been indicated to impact on the antigenic nature of the serotype A viruses from the Middle East (Jamal et al., 2011; Upadhyaya et al., 2014). In addition, analysis of 115 serotype A capsid sequences revealed amino acids VP1-42 to -46 to be highly variable (data not shown). The substitution of threonine at position VP3-132 led to significant reduction in serum titre whereas substitution to alanine did not have much impact, indicating certain residue changes are more powerful than others. Mutations in epitopes may also have the opposite effect, i.e. neutralizing titres may increase after mutation of capsid residues. In fact, Opperman et al. (2014) reported significantly higher VN titres in SAT epitope-replaced mutants that were related to higher avidity index. However, we did not observe significantly higher VN titre in the mutant viruses in this study. In our previous study on serotype O epitope mutants (Asfor et al., 2014) we also did not observe higher VN titre than the homologus virus. This could be due to a different serotype or strain of the virus.
Fig. 3. Percentage reduction in serum titre of selected rO1K/A-EA-2007 mutant viruses that showed significant reduction in serum titre compared with the parent rO1K/A-EA-2007 virus. 2D-VNT was carried out using bovine serum raised against rO1K/A-EA-2007 viral antigen. Error bars indicate sd for the respective mutant. The significance of the test differences were calculated from a total of 16 repeats except for rO1K/A-EA-2007M6 for which only 12 VN test results were used. * and *** indicate significant difference (from parent rO1K/A-EA-2007 virus) at P<0.05 and P<0.001, respectively.
In conclusion, we have predicted epitopes for serotype A viruses from Africa and tested a new epitope/antigenic site (VP1-43/45) for serotype A FMDVs that is equivalent to antigenic site 3 in serotype O. Substitution of threonine (amino acid found in genotype IV viruses) at position VP2-191 with either alanine or aspartic acid confirmed the antigenic significance of this residue as well as mutations at VP1-43, VP1-45 and VP3-132. These residues are novel epitopes that have not been reported previously for serotype A FMDVs.
Methods
Viruses, cells and plasmid.
The 56 East African type A viruses and their corresponding capsid sequences and serology data against seven vaccine strains described previously (Bari et al., 2014) were used in this study. IB-RS2 cells (a pig kidney cell line) were used for growing viruses, titration and VN test. BHK21 cells were used for electroporation and passaging of recombinant viruses.
The most broadly reactive vaccine strain, A-EA-2007 (Bari et al., 2014), was selected for the reverse genetics work in this study. The parental virus was plaque-purified four times on IB-RS2 cells. An existing serotype O infectious copy of FMDV (pT7S3-O1Kwt) containing unique restriction sites at the beginning and end of the capsid-encoding genes (AflII and SpeI restriction sites in the L and 2B regions of the FMDV genome, respectively; Asfor et al., 2014) was used for this study.
RNA extraction, RT-PCR and sequencing.
Total RNA was extracted from cell-culture-grown viruses using RNeasy Mini kits (Qiagen) according to the manufacturer’s recommendation. Reverse transcription (RT)-PCR to amplify the capsid-coding region, nucleotide sequencing and sequence analysis were carried out as described by Upadhyaya et al. (2014).
Construction of recombinant full-length genome plasmid.
Standard molecular biological techniques were used for the cloning of the serotype A capsid into vectors. The A-EA-2007 FMDV capsid-encoding region was amplified from the total RNA isolated from the plaque-purified virus using specific primer set A-EA-2007 AflII F/A-EA-2007SpeI R containing AflII and SpeI restriction sites, respectively (Table S1). The amplified product was cloned in to the intermediate vector pT7Blue (Promega) resulting in generation of pT7Blue-A-EA-2007. The capsid was excised from the intermediate vector using AflII and SpeI restriction enzymes. The excised capsid-encoding region was used to replace the capsid-encoding region of pT7S3-O1Kwt to generate pT7S3-O1K/A-EA-2007. The capsid-encoding region of the full-length genome plasmid was sequenced on both the strands to ensure they were from the desired virus. pT7S3-O1K/A-EA-2007 was used in all subsequent experiments.
Epitope prediction.
In silico methods.
Two different methods of epitope prediction, (a) Shannon entropy (Shannon, 1948) and (b) conservation surface mapping (ConSurf) (Landau et al., 2005; Ashkenazy et al. 2010), were used to predict candidate epitopes from the capsid sequence data of 56 serotype A FMDVs originating from Africa (Bari et al., 2014). The Shannon entropy analysis implemented in BioEdit v7.2.5 (Hall, 1999) was used to calculate the variability of each amino acid position across all VP1-3 sequences taking account of the type and frequency of amino acids. In Shannon entropy, a score more than half of the highest score was used as a cut-off to select the most variable residue. In ConSurf (http://consurf.tau.il), the prediction of epitopes was performed by calculating the evolutionary conservation rate (inverse of evolutionary substitution rate) using a Bayesian method (Ashkenazy et al. 2010) for each position in the multiple amino acid sequence alignments of individual VP regions (VP1-3). The three-dimensional crystal structure of serotype A1061 FMDV (Fry et al., 2005) was used as the reference structure. ConSurf also predicts the location of each amino acid (buried or surface exposed) and assigns an antigenicity score.
By correlating capsid sequence with serology data.
The locations of residues involved in antibody binding sites (epitopes) were inferred by correlating the antibody cross-reactivity of viruses to their capsid sequence similarities as described previously (Reeve et al., 2010). This technique identifies residues responsible for cross-reactivity while controlling for repeated measures arising from the phylogenetic relationship between the viruses. The capsid sequence data of 56 East African type A viruses and their corresponding serology data against seven vaccine strains (Bari et al., 2014) were used for this analysis.
Construction of mutant plasmids.
Standard site-directed mutagenesis (SDM) technique was used to introduce mutations at specific positions in the capsid of pT7S3-O1K/A-EA-2007. A total of eight sites (VP1-43/44/45/81; VP2-191, VP3-131/132/220), all in surface-exposed capsid regions and newly predicted (not previously reported), were selected for further investigation. These residues were substituted either to alanine or with a specific amino acid whose presence in other isolates had been correlated with higher or lower antibody reactivity. Specific overlapping primers were designed to introduce mutations either individually or in combinations to make recombinant viruses containing either single or double substitutions in the capsid (Table S1). The cDNA backbone containing the serotype A capsid was manipulated according to the method described by Asfor et al. (2014). The capsid-encoding regions of all the plasmids were sequenced to confirm the identity of the mutations introduced.
Electroporation and rescue of recombinant viruses.
The parent plasmid (pT7S3-O1K/A-EA-2007) or its derivatives were linearized by digestion with HpaI enzyme and full-length RNA transcripts were synthesized as described previously (Asfor et al., 2014). Electroporation of the transcribed RNA and recovery of the recombinant viruses were also carried out as described previously (Asfor et al., 2014). The rescued viruses were subsequently passaged at least three times before stocks of viruses were made.
Characterization of recombinant viruses.
In order to characterize the recombinant viruses, RT-PCR was carried out on the total RNA isolated from virus-infected BHK-21 cells. The whole capsid was amplified and then sequenced on both strands to ensure all the mutations were present in the respective viruses. Virus titres for each virus were determined on IB-RS2 cells as described by Reed & Muench (1938). The growth kinetics of the mutant and parental recombinant viruses were evaluated as described by Asfor et al. (2014). The plates were frozen at five different time points (0, 4, 8, 12 and 24 h) post-infection. The harvested virus was stored at −70 °C until used. The plaque sizes of the mutant and the parent recombinant viruses were also compared, as described by Asfor et al. (2014).
Generation of polyclonal sera against rO1K/A-EA-2007 vaccine in cattle.
For use in serological assays antisera were prepared in cattle against the recombinant parent virus recovered from the cDNA clone (rO1K/A-EA-2007), which is the parent to all other mutant viruses generated in this study. Briefly, the rO1K/A-EA-2007 virus was grown in BHK-21 cells. When the CPE was complete, the culture supernatant was harvested, clarified by centrifugation, and inactivated with 5 mM binary ethylenimine (BEI) at 25 °C for 24 h (Bahnemann, 1975, 1990). The inactivated antigen was purified by sucrose gradient purification (Ferris et al., 1984) and concentrated by polyethylene glycol precipitation. The vaccine was prepared from the antigen as a water-in-oil-in-water emulsion with Montanide ISA 206 (SEPPIC) adjuvant according to the manufacturer’s recommendation (1 : 1 ratio). Five cattle housed at the high-containment isolation facility of The Pirbright Institute, Pirbright, UK, were used for serum production. All the animals were sero-negative for FMDV antibodies at the beginning of the experiment. The animals were observed for 7 days before the beginning of the experiment to make sure that they were in good health. The animals were injected subcutaneously with 1 ml of an emulsion containing 15 µg each of the recombinant viral antigen. All the animals received a booster at 21 days post-vaccination and were bled 1 week later for serum preparation. The serum was stored at −20 °C until use. A pool of sera from five animals was used for serological tests.
Virus neutralization test.
The 2D-VNT was carried out using the pooled 28th day post-vaccination bovine sera from five animals to determine the sero-reactivity of the mutant viruses according to Rweyemamu et al. (1978). The recombinant virus, rO1K/A-EA-2007, was used as the homologous virus in the VN test. Antibody titres were calculated from regression data as the log10 reciprocal antibody dilution required for 50 % neutralization of 100 tissue culture infective units of virus (log10SN50/100 TCID50). The antigenic relationship of a mutant virus to its parent is given by the ratio: ‘r1’ = neutralizing antibody titre against the mutant virus/neutralizing antibody titre against the recombinant parental virus. The significance of differences between ‘r1-values’ obtained by the polyclonal serum was evaluated according to the method of Rweyemamu & Hingley (1984) using a cut-off r1-value ≥0.3 as representing an expectation of adequate cross protection. Each test was conducted in duplicate and repeated at least eight times. Test results showing evidence of a reduction in serum titre after mutagenesis were repeated eight more times for further confirmation.
Data analysis.
The data were analysed using minitab (version 16) software. A paired t-test was used to compare the differences in sero-reactivity between the homologous and the mutant viruses.
Acknowledgements
We would like to thank WRL-FMD at Pirbright for providing the parental seed viruses used for this study and Dr Abraham Sangula, Kenya Veterinary Vaccine Production Institute, Nairobi, Kenya, for sharing reagents. This work was supported financially by Biotechnology and Biological Sciences Research Council (BBSRC) Institute Strategic Programme on Livestock Viral Diseases at The Pirbright Institute, and BBSRC/Department for International Development/Scottish Government grants BB/F009186/1 and BB/H009175/1.
Footnotes
One supplementary figure and one supplementary table are available with the online Supplementary Material.
References
- Asfor A. S., Upadhyaya S., Knowles N. J., King D. P., Paton D. J., Mahapatra M. ( 2014). Novel antibody binding determinants on the capsid surface of serotype O foot-and-mouth disease virus. J Gen Virol 95, 1104–1116. 10.1099/vir.0.060939-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashkenazy H., Erez E., Martz E., Pupko T., Ben-Tal N. ( 2010). ConSurf 2010: calculating evolutionary conservation in sequence and structure of proteins and nucleic acids. Nucleic Acids Res 38 (Web Server issue), W529–W533. 10.1093/nar/gkq399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahnemann H. G. ( 1975). Binary ethylenimine as an inactivant for foot-and-mouth disease virus and its application for vaccine production. Arch Virol 47, 47–56. 10.1007/BF01315592 [DOI] [PubMed] [Google Scholar]
- Bahnemann H. G. ( 1990). Inactivation of viral antigens for vaccine preparation with particular reference to the application of binary ethylenimine. Vaccine 8, 299–303. 10.1016/0264-410X(90)90083-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bari F. D., Parida S., Tekleghiorghis T., Dekker A., Sangula A., Reeve R., Haydon D. T., Paton D. J., Mahapatra M. ( 2014). Genetic and antigenic characterisation of serotype A FMD viruses from East Africa to select new vaccine strains. Vaccine 32, 5794–5800. 10.1016/j.vaccine.2014.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow D. J., Edwards M. S., Thornton J. M. ( 1986). Continuous and discontinuous protein antigenic determinants. Nature 322, 747–748. 10.1038/322747a0 [DOI] [PubMed] [Google Scholar]
- Baxt B., Vakharia V., Moore D. M., Franke A. J., Morgan D. O. ( 1989). Analysis of neutralizing antigenic sites on the surface of type A12 foot-and-mouth disease virus. J Virol 63, 2143–2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blignaut B., Visser N., Theron J., Rieder E., Maree F. F. ( 2011). Custom-engineered chimeric foot-and-mouth disease vaccine elicits protective immune responses in pigs. J Gen Virol 92, 849–859. 10.1099/vir.0.027151-0 [DOI] [PubMed] [Google Scholar]
- Bolwell C. B., Clarke B. E., Parry N. R., Ouldridge E. J., Brown F., Rowlands D. J. ( 1989). Epitope mapping of foot-and-mouth disease virus with neutralizing monoclonal antibodies. J Gen Virol 70, 59–68. 10.1099/0022-1317-70-1-59 [DOI] [PubMed] [Google Scholar]
- Borley D. W., Mahapatra M., Paton D. J., Esnouf R. M., Stuart D. I., Fry E. E. ( 2013). Evaluation and use of in-silico structure-based epitope prediction with foot-and-mouth disease virus. PLoS ONE 8, e61122. 10.1371/journal.pone.0061122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bøtner A., Kakker N. K., Barbezange C., Berryman S., Jackson T., Belsham G. J. ( 2011). Capsid proteins from field strains of foot-and-mouth disease virus confer a pathogenic phenotype in cattle on an attenuated, cell-culture-adapted virus. J Gen Virol 92, 1141–1151. 10.1099/vir.0.029710-0 [DOI] [PubMed] [Google Scholar]
- Chitray M., de Beer T. A. P., Vosloo W., Maree F. F. ( 2014). Genetic heterogeneity in the leader and P1-coding regions of foot-and-mouth disease virus serotypes A and O in Africa. Arch Virol 159, 947–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowther J. R., Farias S., Carpenter W. C., Samuel A. R. ( 1993). Identification of a fifth neutralizable site on type O foot-and-mouth disease virus following characterization of single and quintuple monoclonal antibody escape mutants. J Gen Virol 74, 1547–1553. 10.1099/0022-1317-74-8-1547 [DOI] [PubMed] [Google Scholar]
- Doel T. R. ( 1996). Natural and vaccine-induced immunity to foot and mouth disease: the prospects for improved vaccines. Rev Sci Tech 15, 883–911. [DOI] [PubMed] [Google Scholar]
- Evans M. C., Phung P., Paquet A. C., Parikh A., Petropoulos C. J., Wrin T., Haddad M. ( 2014). Predicting HIV-1 broadly neutralizing antibody epitope networks using neutralization titers and a novel computational method. BMC Bioinformatics 15, 77. 10.1186/1471-2105-15-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris N. P., Donaldson A. I., Barnett I. T. R., Osborne R.W. ( 1984). Inactivation, purification and stability of 146S antigens of foot-and-mouth disease virus for use as reagents in the complement fixation test. Rev Sci Tech 3, 339–350. [DOI] [PubMed] [Google Scholar]
- Fry E. E., Newman J. W. I., Curry S., Najjam S., Jackson T., Blakemore W., Lea S. M., Miller L., Burman A., et al. ( 2005). Structure of foot-and-mouth disease virus serotype A1061 alone and complexed with oligosaccharide receptor: receptor conservation in the face of antigenic variation. J Gen Virol 86, 1909–1920. 10.1099/vir.0.80730-0 [DOI] [PubMed] [Google Scholar]
- Grazioli, S., Moretti, M., Barbieri, I., Crosatti, M. & Emiliana Brocchi, E. (2006). Use of monoclonal antibodies to identify and map new antigenic determinants involved in neutralisation on FMD viruses type SAT 1 and SAT 2. http://www.fao.org/ag/againfo/commissions/docs/research_group/paphos/App43.pdf
- Grazioli S., Fallacara F., Brocchi E. ( 2013). Mapping of antigenic sites of foot-and-mouth disease virus serotype Asia 1 and relationships with sites described in other serotypes. J Gen Virol 94, 559–569. 10.1099/vir.0.048249-0 [DOI] [PubMed] [Google Scholar]
- Grubman M. J., Baxt B. ( 2004). Foot-and-mouth disease. Clin Microbiol Rev 17, 465–493. 10.1128/CMR.17.2.465-493.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall T. A. ( 1999). BioEdit: a user-friendly biological alignment editor and analysis program for windows 95/98/NT. Nucleic Acids Symp Ser 41, 95–98. [Google Scholar]
- Jamal S. M., Ferrari G., Ahmed S., Normann P., Curry S., Belsham G. J. ( 2011). Evolutionary analysis of serotype A foot-and-mouth disease viruses circulating in Pakistan and Afghanistan during 2002–2009. J Gen Virol 92, 2849–2864. 10.1099/vir.0.035626-0 [DOI] [PubMed] [Google Scholar]
- Kitson J. D. A., McCahon D., Belsham G. J. ( 1990). Sequence analysis of monoclonal antibody resistant mutants of type O foot and mouth disease virus: evidence for the involvement of the three surface exposed capsid proteins in four antigenic sites. Virology 179, 26–34. 10.1016/0042-6822(90)90269-W [DOI] [PubMed] [Google Scholar]
- Kringelum J. V., Lundegaard C., Lund O., Nielsen M. ( 2012). Reliable B cell epitope predictions: impacts of method development and improved benchmarking. PLOS Comput Biol 8, e1002829. 10.1371/journal.pcbi.1002829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R. M., Sanyal A., Hemadri D., Tosh C., Mohapatra J. K., Bandyopadhyay S. K. ( 2004). Characterization of foot-and-mouth disease serotype asial viruses grown in the presence of polyclonal antisera in serology and nucleotide sequence analysis. Arch Virol 149, 1801–1814. [DOI] [PubMed] [Google Scholar]
- Landau M., Mayrose I., Rosenberg Y., Glaser F., Martz E., Pupko T., Ben-Tal N. ( 2005). ConSurf 2005: the projection of evolutionary conservation scores of residues on protein structures. Nucleic Acids Res 33 (Web Server issue), W299–W302. 10.1093/nar/gki370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence P., Pacheco J. M., Uddowla S., Hollister J., Kotecha A., Fry E., Rieder E. ( 2013). Foot-and-mouth disease virus (FMDV) with a stable FLAG epitope in the VP1 G-H loop as a new tool for studying FMDV pathogenesis. Virology 436, 150–161. 10.1016/j.virol.2012.11.001 [DOI] [PubMed] [Google Scholar]
- Liu M. K. P., Hawkins N., Ritchie A. J., Ganusov V. V., Whale V., Brackenridge S., Li H., Pavlicek J. W., Cai F., et al. ( 2013). Vertical T cell immunodominance and epitope entropy determine HIV-1 escape. J Clin Invest 123, 380–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahapatra M., Aggarwal N., Cox S., Statham R. J., Knowles N. J., Barnett P. V., Paton D. J. ( 2008). Evaluation of a monoclonal antibody-based approach for the selection of foot-and-mouth disease (FMD) vaccine strains. Vet Microbiol 126, 40–50. 10.1016/j.vetmic.2007.06.022 [DOI] [PubMed] [Google Scholar]
- Mahapatra M., Seki C., Upadhyaya S., Barnett P. V., La Torre J., Paton D. J. ( 2011). Characterisation and epitope mapping of neutralising monoclonal antibodies to A24 Cruzeiro strain of FMDV. Vet Microbiol 149, 242–247. 10.1016/j.vetmic.2010.11.003 [DOI] [PubMed] [Google Scholar]
- Maree F. F., Blignaut B., Esterhuysen J. J., de Beer T. A. P., Theron J., O’Neill H. G., Rieder E. ( 2011). Predicting antigenic sites on the foot-and-mouth disease virus capsid of the South African Territories types using virus neutralization data. J Gen Virol 92, 2297–2309. 10.1099/vir.0.032839-0 [DOI] [PubMed] [Google Scholar]
- Mateu M. G., Camarero J. A., Giralt E., Andreu D., Domingo E. ( 1995). Direct evaluation of the immunodominance of a major antigenic site of foot-and-mouth disease virus in a natural host. Virology 206, 298–306. 10.1016/S0042-6822(95)80045-X [DOI] [PubMed] [Google Scholar]
- McCahon D., Crowther J. R., Belsham G. J., Kitson J. D., Duchesne M., Have P., Meloen R. H., Morgan D. O., De Simone F. ( 1989). Evidence for at least four antigenic sites on type O foot-and-mouth disease virus involved in neutralization; identification by single and multiple site monoclonal antibody-resistant mutants. J Gen Virol 70, 639–645. 10.1099/0022-1317-70-3-639 [DOI] [PubMed] [Google Scholar]
- Opperman P. A., Rotherham L. S., Esterhuysen J., Charleston B., Juleff N., Capozzo A. V., Theron J., Maree F. F. ( 2014). Determining the epitope dominance on the capsid of a serotype SAT2 foot-and-mouth disease virus by mutational analyses. J Virol 88, 8307–8318. 10.1128/JVI.00470-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan K., Deem M. W. ( 2011). Quantifying selection and diversity in viruses by entropy methods, with application to the haemagglutinin of H3N2 influenza. J R Soc Interface 8, 1644–1653. 10.1098/rsif.2011.0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parida S. ( 2009). Vaccination against foot-and-mouth disease virus: strategies and effectiveness. Expert Rev Vaccines 8, 347–365. 10.1586/14760584.8.3.347 [DOI] [PubMed] [Google Scholar]
- Paton D. J., Valarcher J. F., Bergmann I., Matlho O. G., Zakharov V. M., Palma E. L., Thomson G. R. ( 2005). Selection of foot and mouth disease vaccine strains–a review. Rev Sci Tech 24, 981–993. [PubMed] [Google Scholar]
- Pay T. W., Hingley P. J. ( 1987). Correlation of 140S antigen dose with the serum neutralizing antibody response and the level of protection induced in cattle by foot-and-mouth disease vaccines. Vaccine 5, 60–64. 10.1016/0264-410X(87)90011-9 [DOI] [PubMed] [Google Scholar]
- Piatti P., Hassard S., Newman J. F. E., Brown F. ( 1995). Antigenic variants in a plaque-isolate of foot-and-mouth disease virus: implications for vaccine production. Vaccine 13, 781–784. 10.1016/0264-410X(94)00057-T [DOI] [PubMed] [Google Scholar]
- Qi T., Qiu T., Zhang Q., Tang K., Fan Y., Qiu J., Wu D., Zhang W., Chen Y., et al. ( 2014). SEPPA 2.0–more refined server to predict spatial epitope considering species of immune host and subcellular localization of protein antigen. Nucleic Acids Res 42 (Web Server issue), W59–W63. 10.1093/nar/gku395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed L. J., Muench H. ( 1938). A simple method of estimating fifty percent endpoints. Am J Hyg 27, 493–497. [Google Scholar]
- Reeve R., Blignaut B., Esterhuysen J. J., Opperman P., Matthews L., Fry E. E., de Beer T. A. P., Theron J., Rieder E., et al. ( 2010). Sequence-based prediction for vaccine strain selection and identification of antigenic variability in foot-and-mouth disease virus. PLOS Comput Biol 6, e1001027. 10.1371/journal.pcbi.1001027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas E. R., Carrillo E., Schiappacassi M., Campos R. ( 1992). Modification of foot-and-mouth disease virus O1 Caseros after serial passages in the presence of antiviral polyclonal sera. J Virol 66, 3368–3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinstein N. D., Mayrose I., Martz E., Pupko T. ( 2009). Epitopia: a web-server for predicting B-cell epitopes. BMC Bioinformatics 10, 287. 10.1186/1471-2105-10-287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rweyemamu M. M., Hingley P. J. ( 1984). Food and mouth disease virus strain differentiation: analysis of the serological data. J Biol Stand 12, 225–229. 10.1016/S0092-1157(84)80057-8 [DOI] [PubMed] [Google Scholar]
- Rweyemamu M. M., Booth J. C., Head M., Pay T. W. F. ( 1978). Microneutralization tests for serological typing and subtyping of foot-and-mouth disease virus strains. J Hyg (Lond) 81, 107–123. 10.1017/S002217240005381X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rweyemamu M., Roeder P., MacKay D., Sumption K., Brownlie J., Leforban Y. ( 2008). Planning for the progressive control of foot-and-mouth disease worldwide. Transbound Emerg Dis 55, 73–87. 10.1111/j.1865-1682.2007.01016.x [DOI] [PubMed] [Google Scholar]
- Saiz J. C., Gonzalez M. J., Borca M. V., Sobrino F., Moore D. M. ( 1991). Identification of neutralizing antigenic sites on VP1 and VP2 of type A5 foot-and-mouth disease virus, defined by neutralization-resistant variants. J Virol 65, 2518–2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarangi L. N., Mohapatra J. K., Subramaniam S., Sanyal A., Pattnaik B. ( 2013). Antigenic site variation in foot-and-mouth disease virus serotype O grown under vaccinal serum antibodies in vitro . Virus Res 176, 273–279. 10.1016/j.virusres.2013.07.003 [DOI] [PubMed] [Google Scholar]
- Schiappacassi M., Rieder Rojas E., Carrillo E., Campos R. ( 1995). Response of foot-and-mouth disease virus C3 Resende to immunological pressure exerted in vitro by antiviral polyclonal sera. Virus Res 36, 77–85. 10.1016/0168-1702(94)00099-X [DOI] [PubMed] [Google Scholar]
- Seago J., Jackson T., Doel C., Fry E., Stuart D., Harmsen M. M., Charleston B., Juleff N. ( 2012). Characterization of epitope-tagged foot-and-mouth disease virus. J Gen Virol 93, 2371–2381. 10.1099/vir.0.043521-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon C. E. ( 1948). A mathematical theory of communication. Bell Syst Tech J 27, 379–423. 10.1002/j.1538-7305.1948.tb01338.x [DOI] [Google Scholar]
- Thomas A. A., Woortmeijer R. J., Puijk W., Barteling S. J. ( 1988). Antigenic sites on foot-and-mouth disease virus type A10. J Virol 62, 2782–2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosh C., Venkataramanan R., Pattnaik B., Hemadri D., Sanyal A. ( 1999). Monoclonal antibodies to an Indian strain of type A foot-and-mouth disease virus. Acta Virol 43, 219–225. [PubMed] [Google Scholar]
- Upadhyaya S., Ayelet G., Paul G., King D. P., Paton D. J., Mahapatra M. ( 2014). Genetic basis of antigenic variation in foot-and-mouth disease serotype A viruses from the Middle East. Vaccine 32, 631–638. 10.1016/j.vaccine.2013.08.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rensburg H. G., Henry T. M., Mason P. W. ( 2004). Studies of genetically defined chimeras of a European type A virus and a South African Territories type 2 virus reveal growth determinants for foot-and-mouth disease virus. J Gen Virol 85, 61–68. 10.1099/vir.0.19509-0 [DOI] [PubMed] [Google Scholar]
- Wekesa S. N., Sangula A. K., Belsham G. J., Muwanika V. B., Heller R., Balinda S. N., Masembe C., Siegismund H. R. ( 2014). Genetic diversity of serotype A foot-and-mouth disease viruses in Kenya from 1964 to 2013; implications for control strategies in eastern Africa. Infect Genet Evol 21, 408–417. 10.1016/j.meegid.2013.12.006 [DOI] [PubMed] [Google Scholar]
- Yang G., Li S., Blackmon S., Ye J., Bradley K. C., Cooley J., Smith D., Hanson L., Cardona C., et al. ( 2013). Mutation tryptophan to leucine at position 222 of haemagglutinin could facilitate H3N2 influenza A virus infection in dogs. J Gen Virol 94, 2599–2608. 10.1099/vir.0.054692-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H., Guo J., Jin Y., Yang F., He J., Lv L., Zhang K., Wu Q., Liu X., Cai X. ( 2013). Engineering foot-and-mouth disease viruses with improved growth properties for vaccine development. PLoS ONE 8, e55228. 10.1371/journal.pone.0055228 [DOI] [PMC free article] [PubMed] [Google Scholar]