Figure 1.
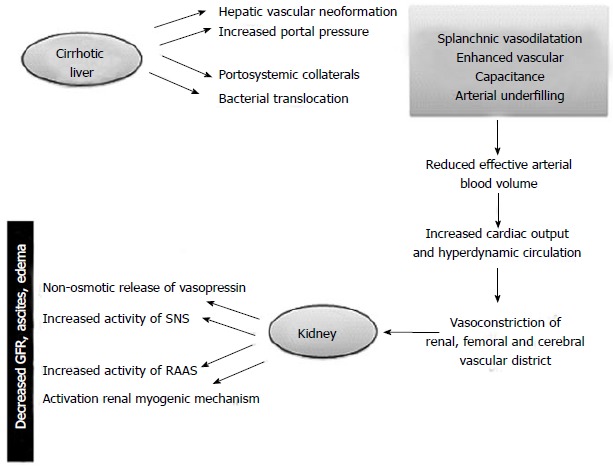
Hepatorenal syndrome: Pathogenesis. In cirrhotic patients portal hypertension can lead to markedly dilated splanchnic arterial vessels. The bacterial translocation of intestinal germs, the gradual decrease in systemic vascular resistances, the hepatic vascular neoformation are potential risk factors. The fall in mean arterial pressure is compensated by increase in cardiac output and by activation of renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system (SNS) to improve systemic vascular resistence. The response mechanisms to the decreased effective circulating volume caused by Enhanced vascular capacitance (so-called “arterial underfilling”) include the non-osmotic release of vasopressin accounting for renal tubular sodium resorption and water retention leading to the onset of ascites, edema and hypervolemic hyponatremia. These compensatory mechanisms ultimately have repercussions on kidney function causing reduced glomerular filtration rate (GFR) and further water retention thereby worsening the water overload.
