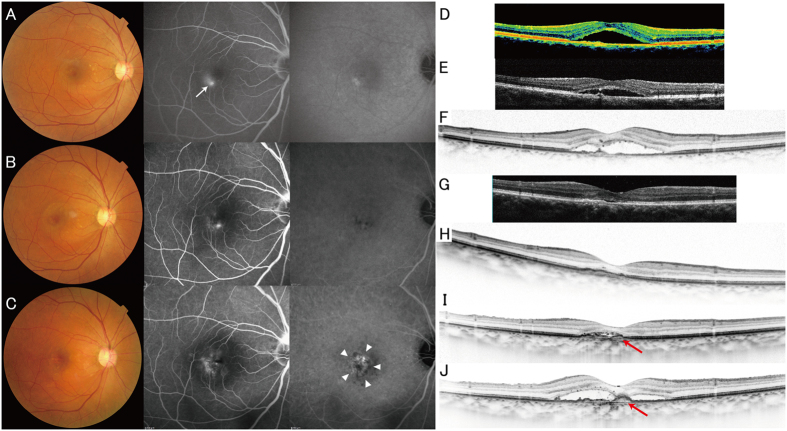
Figure 4. A case of pachychoroid neovasculopathy.
A 50-year-old man visited the macular service at Kyoto University Hospital with a chief complaint of central scotoma in his right eye. (A,D) The color fundus photograph from the patient’s first visit shows serous retinal detachment without drusen. Fluorescein angiography (FA) shows late leakage (ink blot pattern; white arrow). Indocyanine green angiography (IA) image shows no choroidal neovascularization (CNV). Optical coherence tomography (OCT; vertical scan thorough the center of the fovea) shows serous retinal detachment and an almost flat retinal pigment epithelium (RPE) band. All these findings were compatible with a diagnosis of central serous chorioretinopathy (CSC). (E) Four months after the patient’s first visit: OCT shows persistent serous retinal detachment. (B,F) Ten months after the patient’s first visit: CNV is not apparent in either FA or IA. However, there are several protrusions in the OCT image. (G–I) 2.5 yr (G), 4.5 yr (H), and 6.5 yr (I) after the patient’s first visit. After spontaneous resolution of subretinal fluid, it again increased. The RPE band gradually elevated, suggesting the development of CNV (red arrows). (C,J) Seven years after the patient’s first visit, CNV is apparent in both FA/IA (white arrowheads) and OCT (red arrow) images. Choroid is thick all over the macula. Color fundus photography contains no drusen.