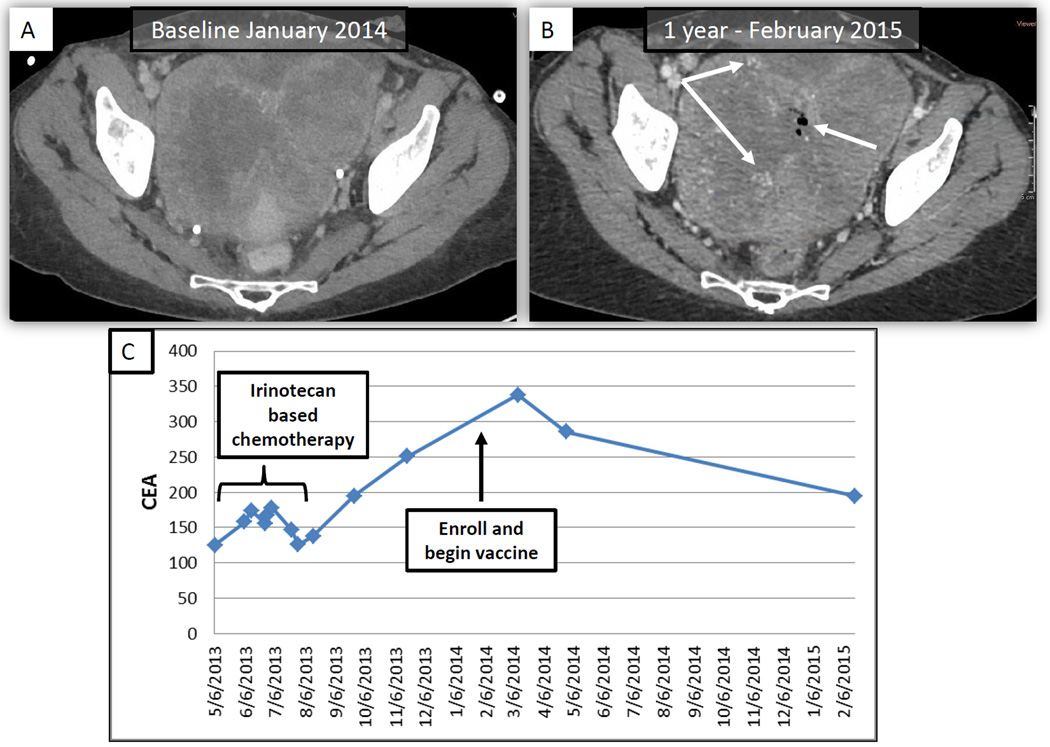
Figure 1.
A 48-year-old female with metastatic colorectal cancer after disease progression through three prior lines of standard therapy enrolled on study with a rising CEA in January 2014. Her main site of disease was a very large pelvic mass, which caused compression of the ureters and the rectum, resulting in the need for colostomy and bilateral nephrostomy tubes. A, Baseline CT scan of the chest, abdomen and pelvis demonstrating large (approximately 14 cm) pelvic mass with compression of ureters and rectum. Note the lack of contrast enhancing vasculature within the tumor and lack of central necrosis (gas). B, Restaging CT scan at 1-year follow-up demonstrating similar size pelvic mass with increased perfusion demonstrated by contrast enhanced vasculature (white arrows) and central gaseous necrosis (white arrow). C, CEA was rising prior to enrollment and declined after enrollment (arrow indicates time of enrollment and first vaccine).