Abstract
Anorectal malignant melanoma (AMM) is an uncommon malignancy that is thought to arise from melanocytes in the mucosa around the anorectal junction. AMM is commonly misdiagnosed, and definitive preoperative diagnosis is often difficult. The prognosis of AMM is relatively poor. Although radical resection is required for AMM, there is still no consensus at this moment on which surgical approach is preferred. We herein report a rare case of AMM which was treated by transanal endoscopic microsurgery (TEM) in combination with radiotherapy, which resulted in complete excision of the lesion without complications. The successful treatment for this AMM using TEM emphasizes the need to broaden its application in the treatment of various rectal lesions while preserving organ function and decreasing recurrence.
Keywords: Anorectal malignant melanoma, differential diagnosis, transanal endoscopic microsurgery
Introduction
AMM is an uncommon and aggressive disease, accounting for less than 1% of all melanomas and about 1% of all anorectal carcinomas, typically presenting in the fifth or sixth decade of life and predominantly in woman [1]. The first case of the disease was reported by Moore in 1857 and so far approximately 500 cases have been reported in the literature [2]. Patients present themselves with local symptoms like rectal bleeding and a changed defecation pattern [3]. These tumors are often misdiagnosed due to their wide macroscopic and histological variability [4]. Prognosis is very poor with a median survival of 24 months and a 5-year survival of 10% [1]. Almost all patients die because of metastases. In addition, due to the low incidence of these tumors and the difficulty in collecting a consistent number of cases in a homogeneous and rational way, clear guidelines for the therapy of anal melanomas are not completely established [3]. Only a few literatures have analyzed and compared some surgical procedures of choice, ranging from an abdomino-perineal resection to local excision with or without adjuvant radiotherapy [3,5-7].
Herein, we present a case of an 85-year-old man previously with hypertension and diabetes suffering from AMM presenting as a fleshy, movable, smooth mass on the anterior wall with 5 cm distance from the anal verge, invading the submucosa. The diagnosis was unclear at first and biopsy was highly indicative of an AMM at stage I. According to the previous knowledge, because AMMs are characterized by high malignancy, abdomino-perineal resection (APR) may provide substantial benefits by avoiding severe symptoms caused by local recurrences, such as incontinence and continuous bleeding of the tumor. But giving the patient’s underlying diseases and poor surgery tolerance, together with his low risk of distant metastases and rapid deterioration (stage I), we performed a local resection by transanal endoscopic microsurgery (TEM) in combination with radiotherapy. The patient survived for 28 months by without the common complications such as urinary retention, temporary incontinences, bleeding and bowel malfunction. We believe TEM was the most appropriate choice for him. The purpose of this article is twofold: to present this rare entity and the first attempt in local excision of it using TEM and to enlighten future clinical researches to further evaluate the clinical consequences and safety of TEM for AMM patients.
Case report
An 85 year old male was admitted to Peking Union Medical College Hospital (PUMCH, China) with a chief complaint of a history of frequent fresh blood stool for 10 days. He also made reference to intermittent pain in the lower abdomen, which began 2 to 3 months ago. He denied nausea and vomiting, rectal tenesmus, change in stool form, urinary continence or anus bulge and pain. The patient did not exhibit fatigue, fever, chills or pruritus. He noticed a slight weight loss despite a normal appetite. The previous history was hypertension for 15 years and impaired glucose tolerance (IGT) for 10 years that can be generally controlled by medication. He once suffered tuberculosis in the 1960s but cured afterwards. His wife and two sons are healthy. We did not identify any special circumstances regarding her family history or personal history related to her presentation. Upon physical examination, he was afebrile with blood pressure of 143/91 mmHg and a regular pulse of 69 bpm. Her abdomen was soft and without tenderness. Bowel sounds were normal at 3-5/min. The digital rectal examination revealed a fleshy, pedunculated, movable and smooth mass about 5 centimeters from anal verge at the 6 o’clock position of the knee-chest position. Whole blood cell test showed RBC count was 3.80×1012/L, HGB was 125 g/L. Stool test showed positive in occult test. Urine routines and a test for liver and kidney function did not show any abnormal changes. Serum cancer-associated biomarkers (CA242, AFP, CEA, CA19-9, CA125, CA72-4 and CA15-3) were all normal. EURS revealed a hypoechoic focal lesion on the anterior wall measuring 1.4×1.2 cm, around 5 cm from anal verge. The lesion invaded the submucosa but not the muscular layer. The surface was smooth. Internal echo was homogeneously low. The lesion had plenty of color signals within and around. Diagnoses of rectal adenocarcinoma, adenoma, adenomatous polyp and carcinoid were all possible (Figure 1). Rectosigmoidoscopy also demonstrated a polypoid tumor on the anterior wall, which was examined by biopsy. Histopathological examination highly suggested a diagnosis of malignant melanoma. Melan-A, S-100, HMB45 were positive and the Ki-67 index was approximately 20% (Figure 2). Abdominal ultrasonography and MRI, thorax CT and brain MRI all showed no evidence for distant or lymph node metastases. According to the 3-level staging system to be used for AMM, which was first described by Ballantyne in 1970 [8], the clinical diagnosis was AMM at stage I.
Figure 1.

Ultrasound image of the AMM. EURS image showed a hypoechoic focal lesion on the anterior wall measuring 1.4×1.2 cm, around 5 cm from anal verge. The lesion invaded the submucosa but not the muscular layer. The surface was smooth. Internal echo was homogeneously low. The lesion had plenty of color signals within and around.
Figure 2.
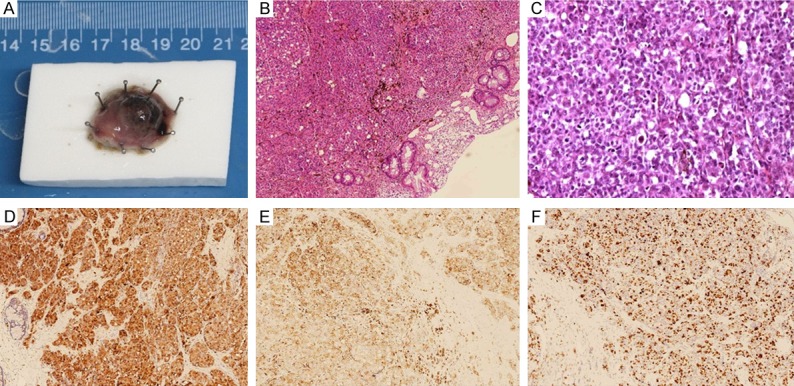
Surgical specimen and bioptic microscopic images. Surgical specimen of the AMM lesion measuring approximately 14 mm×12 mm×6 mm. The cut surface was uniformly smooth, soft and exhibited bright appearance with melanin deposition (A). A pattern of pleomorphic cells with melanin pigmentation of the cytoplasm are seen (B, H-E stain, ×200; C, H-E stain, ×1000). Immunohistochemistry indicated strong staining for S-100 (D, ×200). HMB45 was positive (E, ×200). The proliferation index Ki67% of the AMM was approximately 60% (F, ×200).
It was shown that AMM demonstrating infiltration of the submucosa already had lymph node metastasis in 44% of cases. And primary lymph node metastases are associated with an increased risk of distant metastases and correlate with worse disease-free and overall survival [9]. Fortunately, this patient was not the case. In addition, the patient was 85 years old and had relatively severe underlying diseases. We believed that traditional APR or WLE was very like to cause too many surgical attacks for him. So after obtaining written informed consent, we decided to perform a transanal endoscopic microsurgery (TEM) for him, which allowed for the performance of a full-thickness excision of the lesion (Figure 3). The patient was positioned in the prone position. A 40 mm diameter resectoscope, which was attached to the operating table by a double ball jointed Martin arm, was inserted into the anus after gentle dilatation. The margin of the lesion was made more clearly defined after methylene blue dye topical spray as in chromoendoscopy. A 1 cm resection margin was marked around the lesion before excision by needle diathermy. A full-thickness excision was carried out using the ultrasonic dissector. Defects in the rectal wall were irrigated with a copious amount of chlorhexidine solution and closed using the running sutures of 3/0 absorbable monofilaments. The operation was completed within 40 min with a proximate blood loss of 10 ml (Figure 4). Immediately after surgery, the resected specimen was pinned out on a cork board. Macroscopic examination of the resected specimen confirmed a solid tumor with a size of 14 mm×12 mm×6 mm. The cut surface was uniformly smooth, soft and exhibited bright appearance with melanin deposition (Figure 2). The resection margin was free of the tumor. The histopathological examination confirmed again the diagnosis of malignant melanoma. No analgesic was required postoperatively. The flatus appeared on postoperative day 1. A solid feeding was given on day 4, and the patient was dismissed from PUMCH 6 days after the surgery in good clinical condition. Considering the potential risk of metastasis, he also underwent radiotherapy. The postoperative period was uneventful and the disease seemed to be in remission. At follow-up, no complications of TEM such as urinary retention, temporary incontinences and bleeding which may be associated with lesion location and surgeon experience were found and his bowel function was not affected. However, two years and four months after surgery, the patient died because of inguinal lymph nodes and intra-abdominal metastases.
Figure 3.
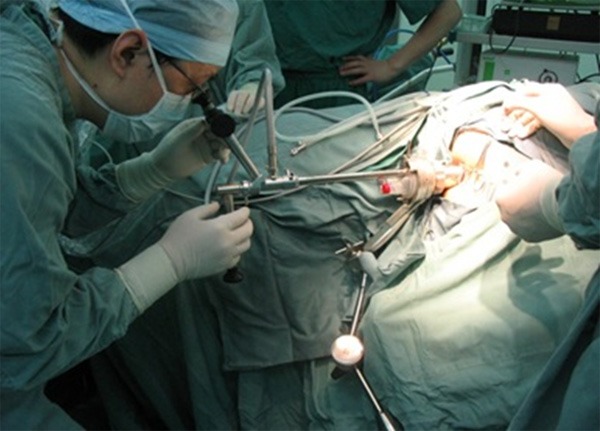
An intraoperative photograph of transanal endoscopic microsurgery (TEM).
Figure 4.
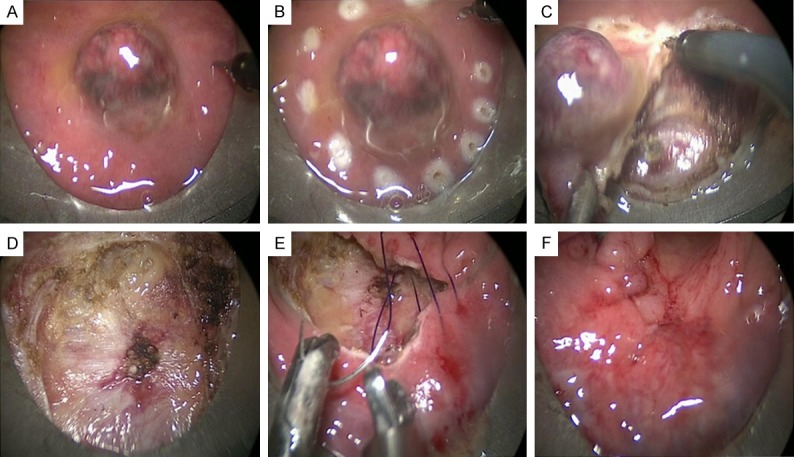
Details of the resection of multiple carcinoids by TEM. A. The rectoscopic view of the AMM. B. A 1 cm resection margin was marked around the lesion before excision by needle diathermy. C, D. Full-thickness excision was carried out using the ultrasonic dissector. E, F. Defects in the rectal wall were closed using the running sutures of 3/0 absorbable monofilaments.
Discussion
First reported by Moore DW in 1857(2), AMM is an extremely rare malignancy and accounts for less than 0.05%-4.6% of all anorectal malignancies. AMM is the third most common primary origin of melanoma following skin and retina [1]. Malignant melanoma arising in anorectal lesions accounts for 0.4%-1.6% of all malignant melanomas [10]. Grossly AMM may display a polypoid mass covered by a smooth surface which may eventually be ulcerated and usually extends into the lower rectum. The rare nature of this entity is represented by the limited number of cases described in the medical literature. AMM patients are more frequently female, and the median age at diagnosis is 60 years or higher [3]. Some epidemiologic data suggest that immunodeficiency virus infection increases the risk of AMM.
Clinical manifestations are non-specific and contribute to a delayed recognition. Presentation symptoms often include rectal bleeding, perineal or anal pain, anal discomfort, tenesmus, fecal incontinence or bowel habit change [3]. AMM is also sometimes diagnosed by a routine health check-up without any symptoms. A mass is usually palpated on digital rectal examination. Proctoscopy usually reveals a hemorrhoid-like pigmented lesion near the anorectal junction, on which a biopsy must be performed, though the histopathologic findings are not always reliable. Almost 60% of patients have already metastases at initial diagnosis [11]. The brain is the most common metastasis site, followed by liver and lung. Therefore, after the histologic diagnosis of AMM, a complete staging and search for possible distant metastases (colonoscopy, computed tomography of the abdomen and thorax, MRI of the pelvis and brain), as well as ruling out primary sites (skin and retina), are mandatory.
Correctly diagnosing AMM is difficult for several reasons: the lack of clinical suspicion due to its very low incidence, the late-onset of non-specific symptoms, the frequent absence of the typical melanin pigmentation, and their histological features overlapping those of other tumors including sarcoma, lymphoma and carcinoma [4]. Thereby, though a few immunohistochemical stains including HMB-45, Melan-A, S-100 and Vimentin tests may help the correct evaluation of preoperative biopsy, AMM is featured by its high misdiagnosis rate up to 80% in some reports. In our case, The diagnosis was unclear at first and biopsy was highly indicative of an AMM. There can be considerable histologic variability for AMM. The use of a panel of immunohistochemical stains, including S-100 protein, MelanA (also known as MART-1), HMB-45, tyrosinase, and a pankeratin, is helpful to the correct diagnosis. Expression of KIT can be present in AMM but can lead to confusion with gastrointestinal stromal tumors when present in spindle cell tumors [12].
The prognosis of AMM is very poor due to its aggressive characteristics. The five year survival rate of AMM is 6%-22%, and the median survival in the literature is 19-26.4 months. The five year survival rate varies according to the presence of metastasis. If AMM is confined to the local area, the five year survival rate is 37%-50%. However, if there is regional and distant metastasis, the five year survival rate decreases in 7%-17% and 0%-6%, respectively [1,3]. The prognosis of AMM differs depending on the stage of AMM. The thickness of the lesion also proves to be an influential factor in AMM, and thickness less than 2 mm is the major factor for determining long-term. It has been proven by various institutions that the tumor depth, size, nodal status at the time of diagnosis all have a significant effect on the survival rate [3].
Surgical resection is the mainstay of treatment [3,5]. APR with or without bilateral inguinal lymphadenectomy and wide local excision (WLE) have been used to manage patients with AMM [5]. APR is thought to reduce the probability of recurrence by controlling the spread to mesenteric lymph nodes and creating a larger negative resection margin. However, despite the absence of prospective studies, increasing evidence suggests that local excision provides comparable survival outcomes with less perioperative morbidity [5-7]. Moreover, this sphincter-sparing approach may benefit the patient’s quality of life [13,14].
Since its introduction by Buess et al in 1983 [15], TEM has emerged as an effective minimal invasive surgery for local resection of rectal lesions. Using a minimally aggressive technique, it allowed the excision of tumors for which local surgery was indicated up to 20 cm from the anal verge and avoided the need for abdominal surgery associated with greater operative morbidity and mortality. Most small rectal tumors without metastasis are ideal candidates of TEM. TEM enables full-thickness excision and ensures accurate resection with sufficient margins by applying the delicate instruments under the superior visualization. In addition, it allows suturing of the rectal wall defects after tumor resection, thus securing sufficient excision without worrying about the bowel perforation [16-18]. In comparison with endoscopic resection methods, including advanced techniques of endoscopic mucosal resection with cap and endoscopic submucosal resection with band ligation, TEM enables much larger extent of resection, ensuring more satisfactory oncological results for lesions with malignant potential [16]. Serra-Aracil et al reviewed other atypical indications in rectal and pelvic disease including pelvic abscess, benign rectal stenoses, rectourethral fistula after prostatectomy, gastrointestinal stromal tumor, endorectal condylomata acuminata, rectal prolapse, extraction of impacted fecaloma in the rectosigmoid junction, repair of traumatic and iatrogenic perforation of the rectum, presacral tumor, rectovaginal fistulas, rectal duplication, pyogenic granuloma, and conservative treatment for the leaks in low colorectal anastomoses [19]. Richa Sharma recently reported a successful treatment for rectal amyloidoma using TEM [18]. As for our case, this is first one about treating AMM which is located in rectal submucosa with TEM. The 85 year old patient got 28 months postoperative long-term survival time (longer than median survival of 24 months) without complications, which may imply the TEM is an appropriate solution for therapy of AMM. However, the potential clinical consequences and safety of a TEM procedure in AMM patients (such as intra-abdominal contamination or infection, and risk of complications and recurrence etc.) are poorly evaluated at present. It needs more clinical data to support the conclusion.
Conclusion
Although uncommon, AMM needs to be included in the differential diagnosis of rectal submucosal tumor. This is first case about treating AMM which is located in rectal submucosa with TEM. The 85 year old patient got 28 months postoperative long-term survival time, which may imply the TEM is an appropriate solution for therapy of AMM. More clinical researches should be done to further evaluate the clinical consequences and safety of TEM for AMM patients.
Disclosure of conflict of interest
None.
References
- 1.Buissin D, Sterle A, Schmiegelow P, Wassenberg D, Ambe PC. Primary anorectal malignant melanoma: a rare but aggressive tumor: report of a case. World J Surg Oncol. 2015;13:12. doi: 10.1186/s12957-014-0419-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miguel I, Freire J, Passos MJ, Moreira A. Anorectal malignant melanoma: retrospective analysis of management and outcome in a single Portuguese Institution. Med Oncol. 2015;32:445. doi: 10.1007/s12032-014-0445-2. [DOI] [PubMed] [Google Scholar]
- 3.Nam S, Kim CW, Baek SJ, Hur H, Min BS, Baik SH, Kim NK. The clinical features and optimal treatment of anorectal malignant melanoma. Ann Surg Treat Res. 2014;87:113–7. doi: 10.4174/astr.2014.87.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erdas E, Calo PG, Licheri S, Pomata M. Unexpected post-operative diagnosis of primary rectal melanoma. A case report. G Chir. 2014;35:137–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Keskin S, Tas F, Karabulut S, Yildiz I, Kiliç L, Ciftci R, Vatansever S. The role of surgical methods in the treatment of anorectal malignant melanoma (AMM) Acta Chir Belg. 2013;113:429–33. [PubMed] [Google Scholar]
- 6.Matsuda A, Miyashita M, Matsumoto S, Takahashi G, Matsutani T, Yamada T, Kishi T, Uchida E. Abdominoperineal Resection Provides Better Local Control But Equivalent Overall Survival to Local Excision of Anorectal Malignant Melanoma: A Systematic Review. Ann Surg. 2015;261:670–7. doi: 10.1097/SLA.0000000000000862. [DOI] [PubMed] [Google Scholar]
- 7.Zhang S, Gao F, Wan D. Abdominoperineal resection or local excision? a survival analysis of anorectal malignant melanoma with surgical management. Melanoma Res. 2010;20:338–41. doi: 10.1097/CMR.0b013e328339b159. [DOI] [PubMed] [Google Scholar]
- 8.Ballantyne AJ. Malignant melanoma of the skin of the head and neck. An analysis of 405 cases. Am J Surg. 1970;120:425–31. doi: 10.1016/s0002-9610(70)80001-0. [DOI] [PubMed] [Google Scholar]
- 9.Falch C, Stojadinovic A, Hann-von-Weyhern C, Protic M, Nissan A, Faries MB, Daumer M, Bilchik AJ, Itzhak A, Brücher BL. Anorectal malignant melanoma: extensive 45-year review and proposal for a novel staging classification. J Am Coll Surg. 2013;217:324–35. doi: 10.1016/j.jamcollsurg.2013.02.031. [DOI] [PubMed] [Google Scholar]
- 10.Parra RS, Almeida AL, Badiale GB, Moraes MM, Rocha JJ, Feres O. Melanoma of the anal canal. Clinics (Sao Paulo) 2010;65:1063–5. doi: 10.1590/S1807-59322010001000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Schaik PM, Ernst MF, Meijer HA, Bosscha K. Melanoma of the rectum: a rare entity. World J Gastroenterol. 2008;14:1633–5. doi: 10.3748/wjg.14.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laforga CJ, Gasent BJ. Amelanotic Anorectal Malignant Melanoma: Case Report with Immunohistochemical Study and Literature Review. Case Rep Oncol. 2009;2:30–7. doi: 10.1159/000204788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Su M, Zhu L, Luo W, Wei H, Zou C. Primary anorectal malignant melanoma treated with neoadjuvant chemoradiotherapy and sphincter-sparing surgery: A case report. Oncol Lett. 2014;7:1605–7. doi: 10.3892/ol.2014.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song Y, Yang G, Qiu J, Zhang X, Deng Q, Wang D. [Evaluation of anal function and quality of life after transanal endoscopic microsurgery] . Zhonghua Wei Chang Wai Ke Za Zhi. 2014;17:809–12. [PubMed] [Google Scholar]
- 15.Buess G, Theiss R, Hutterer F, Pichlmaier H, Pelz C, Holfeld T, Said S, Isselhard W. [Transanal endoscopic surgery of the rectum-testing a new method in animal experiments] . Leber Magen Darm. 1983;13:73–7. [PubMed] [Google Scholar]
- 16.Lin GL, Meng WC, Lau PY, Qiu HZ, Yip AW. Local resection for early rectal tumours: Comparative study of transanal endoscopic microsurgery (TEM) versus posterior trans-sphincteric approach (Mason’s operation) Asian J Surg. 2006;29:227–32. doi: 10.1016/S1015-9584(09)60093-2. [DOI] [PubMed] [Google Scholar]
- 17.Cunningham C. Transanal endoscopic microsurgery. Recent Results Cancer Res. 2014;203:31–8. doi: 10.1007/978-3-319-08060-4_4. [DOI] [PubMed] [Google Scholar]
- 18.Sharma R, George VV. Transanal endoscopic microsurgery: The first attempt in treatment of rectal amyloidoma. World J Gastroenterol. 2015;21:1324–8. doi: 10.3748/wjg.v21.i4.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Serra-Aracil X, Mora-Lopez L, Alcantara-Moral M, Corredera-Cantarin C, Gomez-Diaz C, Navarro-Soto S. Atypical indications for transanal endoscopic microsurgery to avoid major surgery. Tech Coloproctol. 2014;18:157–64. doi: 10.1007/s10151-013-1040-9. [DOI] [PubMed] [Google Scholar]


