Abstract
Microwave ablation is a recent development in the field of tumor ablation that uses electromagnetic waves to establish a microwave near-field with direct tissue heating. Some of the limitations of the earlier generation devices had been unpredictable size and shape of the ablation zones with changes in the surrounding tissue environment as well as differences across various different tissue types. The Emprint Ablation System with Thermosphere Technology (Covidien, Boulder, CO) is the most recent generation ablation system that attempts to produce predictable large spherical zones of ablation despite varying tissue environments across different tissue types such as liver, lung, and bone to name a few. This article will discuss these recent device developments as well as review some basic microwave characteristics.
Keywords: microwave ablation, radiofrequency ablation, thermal ablation, interventional radiology
Objectives: Upon completion of this article, the reader will be able to discuss the differences in current- and field-based ablation technologies, along with the basic science related to microwave ablation. The reader will also be able to identify one of the recent next-generation microwave ablation technologies.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
The arena of heat-based thermal ablation in the management of malignancies has expanded dramatically over the years. Heat-based thermal ablation is now used in many organ systems including liver, kidney, lung, bone, and soft tissue. The number of heat-based thermal ablative tools has expanded and evolved rapidly. The heat-based thermal ablation devices currently available include radiofrequency ablation, microwave ablation, laser ablation, and high-intensity focused ultrasound.1 All of these devices cause local temperature changes to the surrounding tissue that ultimately results in tumor cell death. The two most commonly used heat-based ablation devices are radiofrequency ablation and microwave ablation.
Radiofrequency Ablation versus Microwave Ablation
Radiofrequency ablation is a current-based technology, while microwave ablation is field-based technology.1 Radiofrequency ablation delivers thermal energy via an electric current between the electrode and a ground pad. The main criticism of radiofrequency ablation is the relatively high incidence of local recurrence of larger tumors, especially when located near large blood vessels.2 3 Such current-based technology creates a small ablation zone within a few millimeters of the electrode, and the amount of heat conducted to the tumor periphery is relatively low. Additionally, when a tumor is located near large blood vessels, the adjacent blood flow absorbs a fraction of the deposited energy resulting in convective heat loss and decreased intratumoral temperatures (“heat sink effect”).
Microwave ablation is a recent development in the field of tumor ablation that uses electromagnetic waves to establish a microwave near-field with direct tissue heating. It is not subject to many of the limitations of current-based ablation. Microwave ablation is less susceptible to the heat sink effect because of higher temperatures and shorter ablation times.4 Microwave ablation has rapidly gained favor due to its ability to consistently provide high intratumoral temperatures, fast ablation times, and large ablation volumes.5 However, the shape of the ablation zone can be unpredictable, as it depends in part on inherent characteristics of the target tissues.
The major limitation of all of the heat-based thermal ablation devices is the lack of predictability of the ablation zone size and shape. These limitations must be overcome if ablation is expected to achieve the outcomes that are desired. A specific newer generation microwave ablation system attempts to address these limitations and is designed to create predictable large spherical zones of ablation that are not impacted by varying tissue environments.
Next-Generation Microwave Ablation Systems
The Emprint Ablation System with Thermosphere Technology (Covidien, Boulder, CO) is an improved version of Covidien's previous generation, the Evident Ablation System (Covidien) ablation system. The Emprint Ablation System attempts to overcome the limitations of unpredictable size and shape of the ablation zone frequently seen with previous generation systems. This new device is a 2,450-MHz microwave ablation system, and consists of a 100-W generator with a high efficiency reusable cable and an ablation pump that provides cooling of the probe during ablation. The probes come in various sizes ranging from short (15 cm), standard (20 cm), to long (30 cm). The probes consist of a single body fiberglass shaft that minimizes probe fracture. It can be internally cooled with infusion of saline during ablation. The device was approved for use by the FDA on April 28, 2014.
Basic Science of Microwave Ablation
Prior to discussing the unique properties of The Emprint Ablation System, a brief overview of the basic science of microwave ablation will be helpful. Microwave ablation is a field-based thermal energy source. A rapidly oscillating electromagnetic field is generated that causes frictional heating of water molecules in the soft tissues around the field source. The electromagnetic field is directed to the target tissue by an antenna (also called a probe). The electromagnetic field is able to penetrate all tissues, even those with high electrical impedance such as bone, lung, or charred tissue.6 There are moving electrons in the probe that can be impacted by the surrounding target tissue, which can ultimately impact the probes ablation performance. Different tissues have different impacts, resulting in unpredictable ablation zones. The Emprint Ablation System uses the properties of field-based thermal energy to create predictable large spherical zones of ablation regardless of tissue environment.
Thermosphere Technology
The unique properties that allow The Emprint Ablation to produce reliable large spherical zones of ablation rely on three types of energy control: (1) thermal control, (2) field control, and (3) wavelength control.
Thermal control is based on internally cooling the probe and associated coaxial cables with an infusion of sterile saline, which minimizes nontarget thermal damage as the probe and coaxial cables can become quite hot. The infused sterile saline is circulated down the shaft to the distal tip of the probe, thus ensuring that the entire probe and cables do not become too hot and cause injury to the operator or patient. This ensures a reliable ablation zone that remains unaffected by tissue desiccation near the shaft.
Field control is based on the unique design of the probe and its ability to conform the movement of electrons in the probe to produce a desired field shape. This field shape remains constant despite the changing tissue environments.
Wavelength control is based on maintaining a constant wavelength despite the changing local tissue environment that occurs with heating. As the surrounding tissue heats, the hydration of the tissue is affected, which in turn alters the dielectric constant of the tissue. The changing dielectric constant can alter the electromagnetic wavelength, which will then alter the shape of the electromagnetic field. As the electromagnetic wavelength is altered, this can alter the movement of electrons in the probe, thereby affecting field control. For example, elongation of the electromagnetic wavelength can cause an elliptical-shaped thermal zone, as the wavelength moves away from the tip of the shaft. Thermosphere Technology is able to maintain wavelength control by creating a constant stable environment around the shaft of the probe, maintained by circulating sterile saline along the shaft. This minimizes changes in the dielectric constant immediately surrounding the probe, thus maintaining shorter wavelengths. It also ensures that the desired electron movement pattern is maintained in the probe to achieve reliable field control.
The combination of these three properties allows the Emprint Ablation System to produce reliable large spherical zones of ablation. Howk et al reported predictable and spherical ablation zones in 53 liver and 73 lung ablations in 16 domestic swine over a range of power settings (45, 75, and 100 W) and a range of ablation times (1–10 minutes).7 In fact, the most predictable sizes and zones of ablation were achieved at 100 W. Ierardi et al published one of the earliest in vivo series of patients treated with the Emprint Ablation System.8 These authors demonstrated that the Emprint Ablation System produced technically successful reliable spherical zones of ablation in a short period of time. Ten liver nodules (8 hepatocellular carcinomas and 2 metastases), with a mean diameter of 24.9 mm, were treated percutaneously. The technical success, safety, ablation time, and overall procedure time were recorded. The ablation zone was defined with the use of multiplanar reformatted imaging, and a roundness index transverse was measured. An index of 1 was consistent with a spherical zone of ablation, while an index distant from 1 was consistent with a more oval zone of ablation. In this study, technical success was 100% with a mean ablation time of 3.85 minutes; no major complications were noted. The roundness index transverse was 0.94, meaning that a spherical zone of ablation was consistently achieved.8
The authors have encountered similar results. Fig. 1 illustrates the case of a 55-year-old woman who presented with hepatocellular carcinoma (HCC) involving both lobes of the liver. The patient was not a candidate for transplant or surgical resection. MRI of the abdomen with contrast demonstrated a hyperenhancing, well-encapsulated 2.6 cm × 2.4 cm × 2.6 cm mass in the lateral segment of the left lobe of the liver, as well as a much larger mass in the right lobe of the liver (Fig. 1a). Percutaneous microwave thermal ablation was chosen to treat the left hepatic lobe mass, and transarterial radioembolization was chosen to address the right hepatic lobe mass. The left hepatic lobe mass was treated with the Emprint Ablation System using computed tomography (CT) and ultrasound guidance with the patient under general anesthesia. The mass was ablated with a 15-cm antenna for 8 minutes at 100 W (Fig. 1b). A postablation triple phase CT scan with intravenous contrast showed a nonenhancing, hypoattenuating 3.2 cm × 3.8 cm × 2.9 cm zone of ablation encompassing the mass (Fig. 1c, d). The patient tolerated the procedure well with no immediate or delayed complications.
Fig. 1.
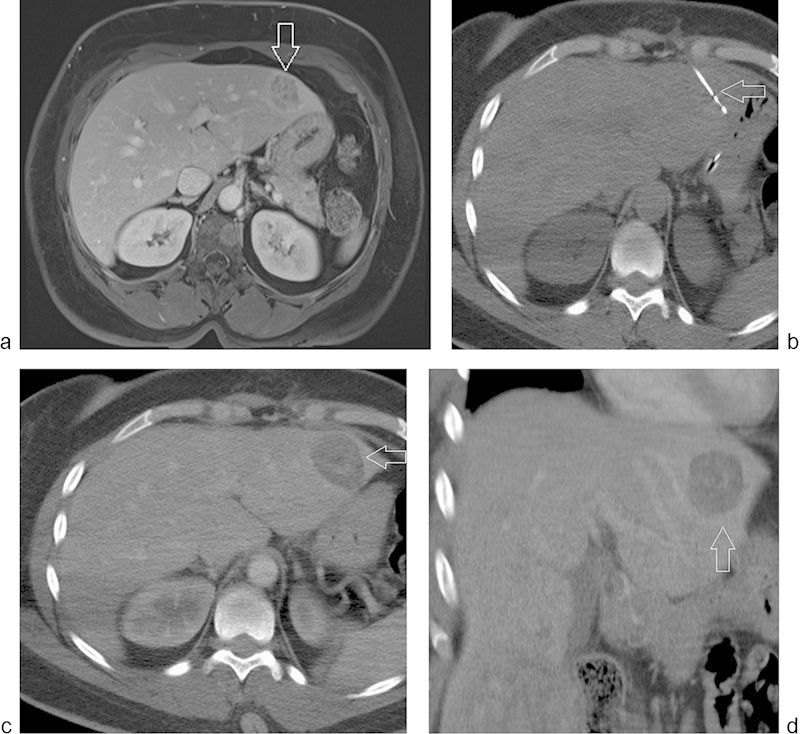
(a) Diagnostic MRI of the liver with intravenous contrast showing the mass in the lateral segment of the left hepatic lobe (arrow). (b) CT imaging showing a 15-cm Thermosphere ablation probe (arrow) in the lesion in the lateral segment of the left hepatic lobe. (c–d) Postablation CT scan with intravenous contrast showing the zone of ablation (arrow) in the axial and coronal planes.
Conclusion
In summary, the Emprint Ablation System is the most recent generation ablation system that attempts to eradicate the unpredictable zones of ablation due to varying tissue environments noted with prior systems. This system is able to create predictable spherical zones of ablation by incorporating thermal control, field control, and wavelength control technology into the system. At this point, experience with this device is preliminary. Long-term studies are required to validate the effectivity of this new device; however, the preliminary imaging and clinical results are definitely encouraging.
Acknowledgments
The authors would like to acknowledge Joseph D. Brannan, MS, Microwave Engineering University of Colorado at Boulder, Inventor/Developer of Thermosphere Technology, for his contribution to this article on the technical aspects of this new device, via verbal communication on June 11, 2015.
References
- 1.Saldanha D F, Khiatani V L, Carrillo T C. et al. Current tumor ablation technologies: basic science and device review. Semin Intervent Radiol. 2010;27(3):247–254. doi: 10.1055/s-0030-1261782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bleicher R J, Allegra D P, Nora D T, Wood T F, Foshag L J, Bilchik A J. Radiofrequency ablation in 447 complex unresectable liver tumors: lessons learned. Ann Surg Oncol. 2003;10(1):52–58. doi: 10.1245/aso.2003.03.018. [DOI] [PubMed] [Google Scholar]
- 3.Crocetti L, de Baere T, Lencioni R. Quality improvement guidelines for radiofrequency ablation of liver tumours. Cardiovasc Intervent Radiol. 2010;33(1):11–17. doi: 10.1007/s00270-009-9736-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feldman L, Fuchshuber P R, Jones D B. New York: Springer; 2012. The SAGES Manual on the Fundamental Use of Surgical Energy (FUSE) [Google Scholar]
- 5.Simon C J, Dupuy D E, Mayo-Smith W W. Microwave ablation: principles and applications. Radiographics. 2005;25 01:S69–S83. doi: 10.1148/rg.25si055501. [DOI] [PubMed] [Google Scholar]
- 6.Hinshaw J L, Lubner M G, Ziemlewicz T J, Lee F T Jr, Brace C L. Percutaneous tumor ablation tools: microwave, radiofrequency, or cryoablation—what should you use and why? Radiographics. 2014;34(5):1344–1362. doi: 10.1148/rg.345140054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howk K, Ladtkow C, Peterson D, Cafaro A. Consistent and predictable spherical ablation shape in both liver and lung: performance of the Emprint Ablation System with Thermosphere Technology in an in vivo porcine model. [Poster 129] J Vasc Interv Radiol. 2015;26(5):e89–e90. [Google Scholar]
- 8.Ierardi A M, Mangano A, Floridi C. et al. A new system of microwave ablation at 2450 MHz: preliminary experience. Updates Surg. 2015;67(1):39–45. doi: 10.1007/s13304-015-0288-1. [DOI] [PubMed] [Google Scholar]


