Abstract
The relationship between posttraumatic stress disorder (PTSD) and asthma in the wake of natural disasters is poorly understood. Using pre- and postdisaster data (N = 405) from the Resilience in Survivors of Katrina (RISK) project, we examined associations between PTSD symptoms, measured by the Impact of Event Scale-Revised (IES-R), and self-reported postdisaster asthma attacks. A 1-point increase in the IES-R avoidance score, which corresponded to one standard deviation change in this sample, was associated with double the odds of reporting an asthma attack or episode since the hurricane, 95% CI Revise spacing among characters: [1.22, 4.16]. Association with hyperarousal and intrusion symptoms was null. Further research using objective measures of asthma morbidity is needed; nevertheless, these findings may help inform postdisaster health services delivery and predisaster mitigation planning.
The prevalence of asthma and other respiratory symptoms increases in the aftermath of natural disasters (e.g., Ohkouchi et al., 2013; Rath et al., 2011). Disrupted access to medication (Hendrickson, Vogt, Goebert, & Pon, 1997) and physical triggers such as contaminated air (Rando, Lefante, Freyder, & Jones, 2012) have been identified as postdisaster asthma risk factors. Given previous research linking posttraumatic stress disorder (PTSD) to a range of general medical conditions (e.g., Boscarino, 2004), PTSD and its symptoms may also help explain increased asthma risk postdisaster. Associations between PTSD and asthma symptoms have been documented among combat veterans (e.g., Caspi, Saroff, Suleimani, & Klein, 2008) and survivors of manmade disasters (Shiratori & Samuelson, 2012). This relationship, however, has not been examined in the context of a natural disaster.
With rare exceptions (e.g., Tomita et al., 2005), the extant literature on the link between PTSD and asthma lack pre-event data on asthma morbidity, making causal relationships difficult to discern. Also, current research has inadequately explored whether the different symptom clusters of PTSD—intrusion, avoidance, and hyperarousal—are uniquely related to asthma risk, though previous studies highlight avoidance symptoms as most strongly associated with behavioral risk factors for asthma, including nicotine dependence and heavy smoking (e.g., Baschnagel, Coffey, Schumacher, Drobes, & Saladin, 2008).
This study drew on pre- and postdisaster data to explore associations between overall PTSD symptoms, as well as individual PTSD symptom clusters, and asthma attacks. Participants were survivors of Hurricane Katrina, which struck the New Orleans area on August 29, 2005 and led to nearly 2,000 deaths and over 650,000 persons displaced, and Hurricane Rita, another intense storm that made landfall in the Gulf Coast less than a month thereafter.
Method
Participants and Procedure
Prehurricane data were collected from 1,019 predominantly low-income, non-Hispanic Black parents recruited from two community colleges in New Orleans in 2003–2005 as part of a study on academic persistence (Brock & Richburg-Hayes, 2006). Participants had to (a) be between the ages of 18 and 34 years and (b) be parents of at least one dependent child under 19 years; (c) have a household income under 200% of the federal poverty level; and (d) have a high school diploma or equivalent. In 2006–2007 (7–19 months postdisaster), the study was redesigned as the Resilience in Survivors of Katrina (RISK) project, and 711 of the 1,019 participants were located and surveyed by telephone. The study was approved by the Harvard and Princeton institutional review boards.
Of the 711 postdisaster participants, 402 had been surveyed twice prior to Hurricane Katrina, and 309 had been surveyed once. We excluded 223 members of the latter group for whom we could not establish the temporal order of hurricane exposure and asthma symptoms at follow-up. We also excluded men (n = 24), who accounted for only 6.2% of the follow-up sample, and participants missing health, PTSD symptom, demographic, or flood depth information (n = 59). The resulting 405 participants served as our primary study sample. Sensitivity analyses drew on a subsample with more detailed data on hurricane-related experiences (n = 323). No differences were detected between participants in the primary sample versus the subsample on flooding exposure (p = .963), PTSD symptoms (p = .260), asthma diagnosis (p = .431), or other key variables except for age (p = .034), which was included in the analysis.
Measures
Participants surveyed twice prior to the disaster reported whether they had “had episode of asthma or an asthma attack” (yes/no) since Hurricane Katrina. Participants with one predisaster assessment reported on asthma episodes or attacks (yes/no) in the past 12 months, and we excluded all respondents (n = 223) who were surveyed within a year of Hurricane Katrina (Figure 1).
Figure 1.
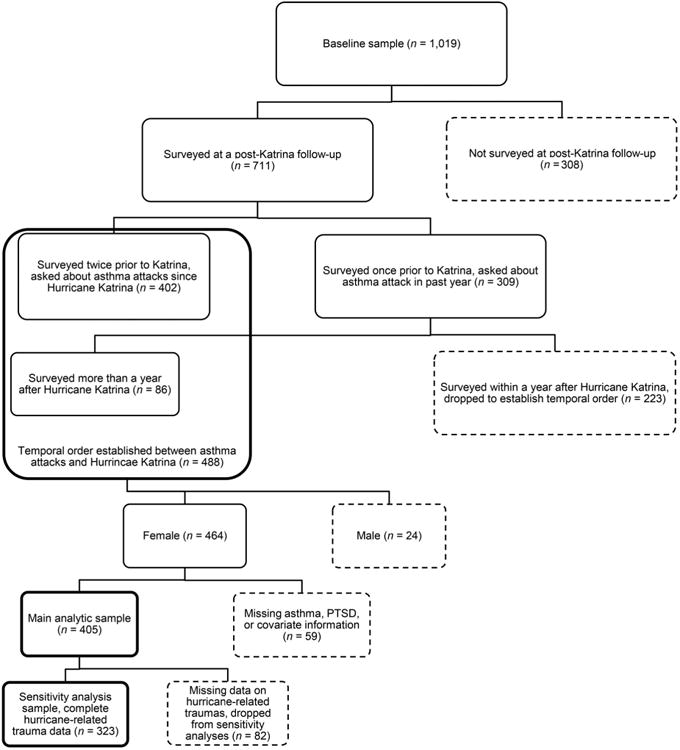
Flowchart showing process of composition of final sample and subsample.
The Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997), a 22-item self-report inventory with good psychometric properties (Creamer, Bell, & Failla, 2003), was administered at follow-up to measure hurricane-related PTSD symptoms. Participants were asked how much they were distressed or bothered by experiences related to Hurricane Katrina over the prior week, from 0 = not at all to 4 = extremely. Overall and subscale mean scores (range: 1–4) were used in the analyses. Cronbach's α reliability ranged from .84 to .95.
Health, social, and demographic variables were self-reported at baseline, and included lifetime asthma diagnosis, household food stamp assistance, age, and race/ethnicity. We also had a measure of severity of hurricane exposure as measured by flood depth in subjects' homes calculated from geocoded address and flood records.
Sensitivity analyses adjusted for three additional measures of hurricane exposure: home damage, bereavement (whether a close friend or relative was killed due to the hurricanes and their aftermath), and an index of the following events: (a) no fresh water to drink, (b) no food to eat, (c) felt their life was in danger, (d) lacked necessary medicine, (e) lacked necessary medical care, (f) had a family member who lacked necessary medical care, (g) lacked information regarding safety of children, and (h) lacked information regarding safety of other family members. Trauma index items were asked for both Hurricanes Katrina and Rita, yielding 16 items, and the sum of affirmative responses was included as a variable.
Data Analysis
Analyses were conducted in Stata 12.1 SE. (StataCorp., 2011) First, we estimated a series of logistic regression equations with measures of overall PTSD symptoms (Model 1) and symptom clusters (Model 2) predicting odds of a postdisaster asthma attack. Models were adjusted for baseline health, social, and demographic variables, and hurricane exposure. Second, models were replicated with the subsample of participants for both overall symptoms (Model 3) and clusters (Model 4) with more detailed information on hurricane exposure. Lastly, we considered reverse causation by using the same subsample to test whether predisaster asthma predicted subsequent PTSD symptoms after considering individual characteristics and hurricane exposure.
Results
Descriptive data for study variables are listed in Table 1. Adjusted logistic regression models showed that overall PTSD symptoms were not associated with higher odds of reporting an asthma attack (p = .070). Each point on the IES-R, however, was equivalent to a SD change in this sample, and corresponded to roughly 54% higher odds of having experienced a postdisaster asthma attack or episode; nevertheless, the 95% confidence interval (CI) around this estimate contained 1.0, 95% CI [0.97, 2.45] (Table 2). One point on the IES-R avoidance subscale, again equivalent to a SD change in this sample, was associated with twice the odds of an asthma attack (p = .010; 95% CI [1.22, 4.16]). Reexperiencing and hyperarousal were not significantly related to asthma attacks. As expected, prior asthma diagnosis was the strongest risk factor for postdisaster asthma morbidity, corresponding to a 38-fold increase in the odds of subsequent asthma attacks, p < .001; 95% CI [15.17, 96.75].
Table 1. Sample Characteristics.
| Variable | n | M or n | SD or % |
|---|---|---|---|
| Diagnosed with asthma prior to baseline (%) | 405 | 49 | 12.1 |
| Experienced asthma episode/attack since Hurricane Katrina (%) | 405 | 34 | 8.4 |
| Non-Hispanic White (%) | 405 | 43 | 10.6 |
| Non-Hispanic Black (%) | 405 | 344 | 84.9 |
| Hispanic (%) | 405 | 10 | 2.5 |
| Other race/ethnicity (%) | 405 | 8 | 2.0 |
| Food stamp assistance (%) | 405 | 253 | 62.5 |
| Age at baseline | 405 | 25.20 | 4.45 |
| Home flooding depth (feet) | 405 | 1.45 | 2.22 |
| IES-R Intrusion | 405 | 1.61 | 1.12 |
| IES-R Avoidance | 405 | 1.54 | 1.02 |
| IES-R Hyperarousal | 405 | 1.21 | 1.14 |
| IES-R Total | 405 | 1.48 | 0.99 |
| Hurricane-related trauma | |||
| Minimal, or not serious home damage | 344 | 55 | 16.0 |
| Moderate or substantial home damage | 344 | 145 | 42.2 |
| Enormous home damage/home was destroyed | 344 | 144 | 41.9 |
| Bereavement | 403 | 111 | 27.5 |
| Hurricane-related traumas | 335 | 3.61 | 3.30 |
Note. IES-R = Impact of Event Scale–Revised
Table 2. Odds Ratios of Asthma Attack Since Hurricane Katrina for PTSD Symptom Scores and Covariates.
| Model 1 (n = 405) | Model 2 (n = 405) | Model 3 (n = 323) | Model 4 (n = 323) | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Variable | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| IES-R Avoidance | 2.25** | [1.22, 4.16] | 3.03** | [1.37, 6.68] | ||||
| IES-R Hyperarousal | 0.97 | [0.44, 2.17] | 1.06 | [0.39, 2.88] | ||||
| IES-R Intrusion | 0.82 | [0.35, 1.93] | 0.62 | [0.20, 1.90] | ||||
| IES-R Total | 1.54 | [0.97, 2.45] | 1.55 | [0.88, 2.72] | ||||
| Asthma at baseline | 32.69*** | [13.64, 78.35] | 38.31*** | [15.17, 96.75] | 45.21*** | [14.81, 138.00] | 48.88*** | [14.97, 159.58] |
| Food stamps | 1.53 | [0.59, 3.96] | 1.58 | [0.60, 4.18] | 1.14 | [0.38, 3.38] | 1.17 | [0.38, 3.63] |
| Race/ethnicity (Non-Hispanic White = reference) | ||||||||
| Non-Hispanic Black | 0.47 | [0.13, 1.74] | 0.44 | [0.12, 1.63] | 0.73 | [0.15, 3.56] | 0.64 | [0.13, 3.20] |
| Hispanic | 0.76 | [0.04, 13.00] | 0.72 | [0.04, 13.27] | 1.44 | [0.06, 33.18] | 1.47 | [0.06, 35.99] |
| Other | 0.79 | [0.07, 8.63] | 0.74 | [0.07, 8.10] | 4.21 | [0.18, 99.47] | 6.26 | [0.18, 218.17] |
| Age | 1 | [0.91, 1.11] | 1.01 | [0.92, 1.12] | 1.02 | [0.91, 1.15] | 1.05 | [0.92, 1.19] |
| Home depth flood | 0.9 | [0.72, 1.12] | 0.9 | [0.73, 1.13] | 1.05 | [0.80, 1.37] | 1.03 | [0.78, 1.34] |
| Bereavement | 2.23 | [0.69, 7.13] | 2.36 | [0.72, 7.75] | ||||
| Hurricane-related traumas | 0.95 | [0.81, 1.13] | 0.95 | [0.80, 1.13] | ||||
| Hurricane-related home damage (none, minimal, not serious= reference) | ||||||||
| Moderate or substantial home damage | 3.1 | [0.58, 16.47] | 3.46 | [0.62, 19.31] | ||||
| Enormous home damage/home was destroyed | 2.4 | [0.40, 14.52] | 2.54 | [0.40, 16.28] | ||||
Note. Detailed hurricane exposure variables are included only in Model 3 and Model 4 because these models replicate Model 1 and Model 2 using a subsample of participants with complete hurricane exposure data. Hurricane-related trauma and home damage data were not available for our primary sample and so are not included in Model 1 or Model 2. IES-R = Impact of Event Scale–Revised.
p < .05.
p < .01.
p < .001.
The relationship between avoidance symptoms and asthma persisted in sensitivity analyses despite the smaller sample size, with a 1 SD or 1 point increase on the IES-R avoidance subscale associated with 3 times higher odds of an asthma attack, p = .006; 95% CI [1.37, 6.68], (Table 2). Participants with a baseline asthma diagnosis were not at higher risk of overall PTSD symptoms (p = .336), nor of avoidance symptoms (p = .116), than were those without asthma.
Discussion
Including baseline asthma diagnosis and hurricane exposure in the model, we found an association between PTSD avoidance symptoms and higher odds of reporting a postdisaster asthma attack or episode. In contrast, our results showed no association between asthma and intrusion or hyperarousal symptoms. We found no evidence that baseline asthma diagnoses put subjects at elevated risk of experiencing PTSD symptoms, meaning that reverse causation was an unlikely driver of the observed associations.
PTSD avoidance symptoms may increase risk of asthma attack through direct physiological changes or by spurring behavioral changes. Psychological triggers have been shown to produce asthma symptoms in both observational and experimental settings (Lehrer, Feldman, Giardino, Song, & Schmaling, 2002). PTSD avoidance symptoms have also been linked to health behaviors known to exacerbate asthma including cigarette smoking (Baschnagel et al., 2008) and avoidant coping behaviors (Boden, Bonn-Miller, Vujanovic, & Drescher, 2012). Testing the meditational pathways from PTSD avoidance to asthma would be a fruitful area for further research.
Although avoidance symptoms were much less powerful in predicting postdisaster asthma morbidity than was a prior asthma diagnosis, this study sought to improve our understanding of the relationship between asthma and PTSD rather than to identify the main drivers of postdisaster asthma. The effect we identified, though a relatively small contribution to overall odds of postdisaster asthma attacks, highlights a potential area of intervention to reduce asthma morbidity and better plan for the care of disaster survivors.
There are several limitations to this study. First, we lacked information on the severity, frequency, or timing of asthma attacks. Random measurement error, introduced by coding participants with severe and mild asthma symptoms identically, widens confidence intervals around coefficients of interest, making associations harder to detect (Hutcheon, Chiolero, & Hanley, 2010). Second, participants with avoidance symptoms could be more likely to recall asthma episodes or to interpret the physical symptoms of panic or anxiety as asthma, regardless of whether airways are actually constricted (Lehrer et al., 2002), potentially inflating associations between PTSD avoidance and asthma attacks. Nonetheless, associations with perceived asthma morbidity may still be useful in predicting utilization of health care services to treat asthma, or in understanding perceptions of morbidity and quality of life. Lastly, participants were predominantly low-income, non-Hispanic Black mothers from New Orleans, and the results may not be generalizable to other populations. Our study population, however, may be of interest to researchers and practitioners working to eliminate health disparities.
Despite limitations, our results may help inform postdisaster health services delivery and predisaster mitigation planning; clinicians and disaster planners should be aware that demand for asthma-related health care may rise among survivors, as suggested by previous research (Ohkouchi et al., 2013; Rath et al., 2011), and that those experiencing PTSD avoidance symptoms may be at particular risk.
Acknowledgments
This paper was funded by National Institutes of Health Grants R01HD046162, RO1HD057599, the National Science Foundation, and the MacArthur Foundation. SVS, JER, and MCW are supported by the Robert Wood Johnson Investigator Award in Health Policy.
References
- Baschnagel JS, Coffey SF, Schumacher JA, Drobes DJ, Saladin ME. Relationship between PTSD symptomatology and nicotine dependence severity in crime victims. Addictive Behaviors. 2008;33:1441–1447. doi: 10.1016/j.addbeh.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Vujanovic AA, Drescher KD. A prospective investigation of changes in avoidant and active coping and posttraumatic stress disorder symptoms among military veteran. Journal of Psychopathology and Behavioral Assessment. 2012;34:433–439. doi: 10.1007/s10862-012-9293-6. [DOI] [Google Scholar]
- Boscarino JA. Posttraumatic stress disorder and physical illness: Results from clinical and epidemiologic studies. Annals of the New York Academy of Sciences. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- Brock T, Richburg-Hayes L. Paying for persistence: Early results of a Louisiana scholarship program for low-income parents attending community college. New York, NY: MRDC; 2006. [Google Scholar]
- Caspi Y, Saroff O, Suleimani N, Klein E. Trauma exposure and posttraumatic reactions in a community sample of Bedouin members of the Israel Defense Forces. Depression and Anxiety. 2008;25:700–707. doi: 10.1002/da.20449. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale—Revised. Behaviour Research and Therapy. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Hendrickson LA, Vogt RL, Goebert D, Pon E. Morbidity on Kauai before and after Hurricane Iniki. Preventive Medicine. 1997;26:711–716. doi: 10.1006/pmed.1997.0196. [DOI] [PubMed] [Google Scholar]
- Hutcheon JA, Chiolero A, Hanley JA. Random measurement error and regression dilution bias. BMJ. 2010;340:c2289–c2289. doi: 10.1136/bmj.c2289. [DOI] [PubMed] [Google Scholar]
- Lehrer P, Feldman J, Giardino N, Song HS, Schmaling K. Psychological aspects of asthma. Journal of Consulting and Clinical Psychology. 2002;70:691–711. doi: 10.1037/0022-006X.70.3.691. [DOI] [PubMed] [Google Scholar]
- Ohkouchi S, Shibuya R, Yanai M, Kikuchi Y, Ichinose M, Nukiwa T. Deterioration in regional health status after the acute phase of a great disaster: Respiratory physicians' experiences of the Great East Japan Earthquake. Respiratory Investigation. 2013;51:50–55. doi: 10.1016/j.resinv.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Rando RJ, Lefante JJ, Freyder LM, Jones RN. Respiratory health effects associated with restoration work in post-Hurricane Katrina New Orleans. Journal of Environmental and Public Health. 2012;2012:462–478. doi: 10.1155/2012/462478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rath B, Young EA, Harris A, Perrin K, Bronfin DR, Ratard R, et al. Magnus M. Adverse respiratory symptoms and environmental exposures among children and adolescents following Hurricane Katrina. Public Health Reports. 2011;126:853–860. doi: 10.1177/003335491112600611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiratori Y, Samuelson KW. Relationship between posttraumatic stress disorder and asthma among New York area residents exposed to the World Trade Center disaster. Journal of Psychosomatic Research. 2012;73:122–125. doi: 10.1016/j.jpsychores.2012.05.003. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Tomita K, Hasegawa Y, Watanabe M, Sano H, Hitsuda Y, Shimizu E. The Totton-Ken Seibu earthquake and exacerbation of asthma in adults. The Journal of Medical Investigation: JMI. 2005;52:80–84. doi: 10.2152/jmi.52.80. [DOI] [PubMed] [Google Scholar]
- Weiss D, Marmar C. The Impact of Event Scale Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD–a practitioners handbook. New York, NY: Guilford Press; 1997. [Google Scholar]


