Abstract
Background:
Discharge against Medical Advice (DAMA) is a problem for hospitals which may result in increasing readmissions, morbidities, inabilities, deaths and health care costs. This study, aimed to investigate the rate and causes of DAMA in Iranian hospitals.
Methods:
A systematic review and meta-analysis study was conducted in 2014. Required data were collected through searching for key words included: “Discharge Against Medical Advice”, “Leaving against medical advice”, “causes*”, “hospital” and their Persian equivalents, over databases including PubMed, OVID, Google Scholar, Embase, Scopus, Magiran, scientific information database (SID). The reference lists of the articles, certain relevant journals and web sites in this field were also searched.
Results:
Out of 913 articles initially retrieved, finally 17 articles were incorporated into the study. There were 244858 individuals studied in the articles. Using a random effects model, the rate of DAMA in Iranian hospitals was estimated at 7.9% (6.3%–9.8%). While the highest rate of DAMA was associated with patients in departments of psychiatry (12%), the lowest rate was related to patients in departments of pediatrics (3.7). DAMA was in men more than women (P<0.05) Patient’s perception of feeling of wellbeing, financial problems, family problems, the lack of attention from physicians and nurses, inappropriate behavior with patients by hospital team and the lack of timely care were mentioned as main causes for DAMA.
Conclusion:
The rate of DAMA in Iranian hospitals is relatively high. Thus effective initiatives in this area are required.
Keywords: Rate, Causes, Discharge, Systematic review, Meta-analysis, Iran
Introduction
Discharge with Discharge against Medical Advice (DAMA) is a major problem for inpatient care delivery considered as one of the indicators of patient dissatisfaction (1, 2). DAMA means a rejection of the permission previously given by the patient to allow health services providers to take care of him (3).
However the prevalence of DAMA has been reported as 1%– 25% (4–6). DAMA is accounted for one percent of total discharges in Canada and varies from 0.8% to 2.2% in the US (5, 7). Besides, in studies conducted in Iran, various rates of DAMA have been reported (8–10).
DAMA is regarded as a risk factor for the recurrence of disease, readmission and higher costs for patient (11–13). Incurred costs due to DAMA in five years were estimated to be nearly 3 billion dollars (14). Patient dissatisfaction with the medical team, personal or family problems, patient’s perception of feeling of wellbeing, dissatisfaction with treatment provided, low economic status, improper equipment, the lack of medical and nursing care can be mentioned as the most significant causes for DAMA (14–16).
Through investigating the rate and causes contributing to DAMA in hospitals, their weaknesses can be identified, and accordingly planning should be done to resolve problems and decrease the rate of DAMA. Such attempts may play an important role not only in promoting the health of population, but also in reducing additional costs and increasing hospital revenue.
This study, therefore, aimed to estimate the rate of and causes contributing to DAMA in Iranian hospitals through conducting a systematic review and meta-analysis of the results of published studies.
Methods
Search strategy
A systematic review and meta-analysis study was conducted in 2014 and a search strategy was developed by an experienced librarian. Required data were collected through searching for key words included: “DAMA”, “Leaving against medical advice”, “Causes*”, “hospital” and their Persian equivalents using databases including PubMed, OVID, Google Scholar, Embase, Scopus, Magiran, scientific information database (SID), Google Search engine, and also gray literature. To increase the confidence in the selection of articles, the reference lists of the articles, certain relevant journals and web sites in this field also were searched.
Including and excluding criteria
Published articles from January 2000 to December 2014 indicating the rate of DAMA were included. The inclusion criteria included: articles in English and Persian language; studies conducted in Iranian hospitals, articles reporting the rate of DAMA.
The following articles were excluded; Letters to editor, Presentations in conferences and Case Reports.
Quality Assessment
To assess the quality of the retrieved articles, two authors evaluated the articles according to the checklist of strengthening the Reporting of Observational studies in Epidemiology (STROBE).
Data Extraction
In the First phase, articles non-relevant to the subject of this study were excluded. In the second phase, the abstract and the full text of articles were reviewed. Computer software for reference management (Endnote X5) was used for organizing and recognizing the duplication articles.
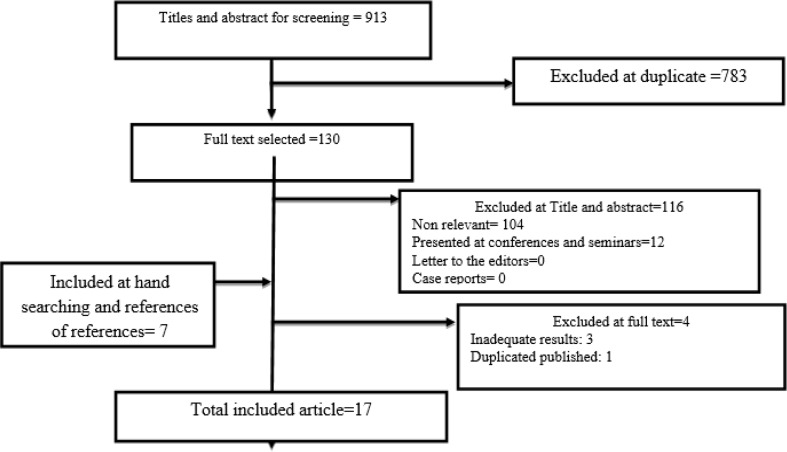
Result of primary search included 913 articles. After excluding non-relevant articles and duplicates among different databases as well as matching the exclusion criteria, 17 articles were incorporated into the study (Fig. 1). The extracted data were summarized in previously designed extraction tables included: Author and year, City, Sample and sample size, DAMA prevalence (%), DAMA-Male Gender (%), DAMA cause (%).
Fig. 1:
Literature review and retrieval flow diagram
Data analysis
Causes
To estimate the rate of DAMA, a quantitative meta-analysis method was adopted using Computer software (CMA: 2—Comprehensive Meta-Analysis). In order to report the results, forest plots with 95% confidence interval and Funnel plot were used to report the rate of DAMA and examine the publication bias, respectively. According to the Q statistics indicating heterogeneity of results in different studies, the random effect model was used to perform meta-analyses.
To compare the rate of DAMA between female and male we conducted t-test by using SPSS Version 16 Software (Chicago, IL, USA). P-value of less than 0·05 was regarded as statistically significant.
The contributing causes of DAMA were extracted through the method of manual Content-Analysis. This method is used to detect, categorize and report themes from text and is very popular in analyzing qualitative data (17). Two researchers coded data by through the following process: Data immersion (getting accustomed to data context), identifying and extracting primary codes, themes detection (assigning the extracted primary codes to the related themes), reviewing and completing the detected themes, naming and defining themes, the reliability assurance of extracted codes and themes (two encoders agreed on removing disputed cases through discussion).
Results
Out of 913 retrieved articles by the initial search, 17 articles were incorporated into the study (8, 18–32).The information from the studied articles has been provided in Table 1. In general, there were 244858 individuals studied in the articles. The articles were published from 2010 to 2014. As it is observed in Table 1, the studies related to the rate measurement of discharge against medical advice have been conducted only in seven cities of Iran especially in Tehran with the most frequency. The lowest rate of discharge against medical advice was reported by a study with the participation of 4835 inpatient children in Sari (2.2%). The highest rate of discharge against medical advice was belonged to a study conducted on 1171 patient form the department of physiotherapy (34.4%). The mean score of discharge against medical advice was higher in men compared with women (42.3±6.5 versus 57.6±6.5). The statistical test showed that the difference in the rate of discharge against medical advice between two gender is statistically significant (P<0.05). Out of the 17 reviewed articles, 3 articles have investigated DAMA among patients in departments of pediatrics, 2 articles in departments of psychiatry, 4 articles in emergency departments, 7 articles in inpatients wards (whole hospital) and 1 article in department of cardiology.
Table 1:
Characteristics of reviewed articles
| DAMA cause (%)* | DAMA-Male Gender (%) | DAMA Prevalence (%) | Sample and sample size | City | Reference Number |
|---|---|---|---|---|---|
|
Patient- related reasons: financial constraint (7.9), family problems (3.4), feeling of wellbeing (59.7), Be traveler (6.2). Hospital condition: Nurse and Physician negligence (15.5), Inappropriate behavior (5/4), physician’s suggestion (18), absence of timely physician (6.2), lack of skilled medical staff (18/3), Improper cleaning (3.7), inadequate equipment (5.6), poor nutrition (1.1), unsuitable environment (8.2). |
56.6 | 1100 (4.2) | Children-26089 | Mashhad | 18 |
| Hospital staff- related reason (16.5), treatment related reason (39.2), Hospital condition (23.2), Patient- related reasons (54.0) | - | 237 (4.6) | General patients - 5137 | Urmia | 21 |
|
Patient- related reasons: financial constraint (3.1), family problems (20.1), fear of treatment (5.1), patient job (4.5), no have family member in hospital (12.2), feeling of wellbeing (28.4), Be traveler (26.2) Hospital condition: Nurse and Physician negligence (34.3), Inappropriate behavior (13), absence of timely physician (18.8), lack of skilled medical staff (30.4), improper cleaning (9.4), inadequate equipment (19.8), poor nutrition1 (8.6), unsuitable environment (6.2), other (3.3) |
55.5 | 2026 (10.3) | General patients- 19660 | 8 | |
|
Patient- related reasons: feeling of wellbeing (20), unhopeful from treatment (3), Transferring to another hospital (4), Transportation problem (7), Lack of consent to surgery or invasive procedures (5), holiday (3), not have family support (3), refer to previous doctor (10) Hospital condition: fear of hospital infection (20), Inappropriate behavior (7), inadequate equipment (2), absence of timely physician (2), treatment by medical students (6), couldn’t choice a doctor (8) |
59/6 | 483 (5.1) | General patients- 9295 | Kerman | 22 |
|
Patient- related reasons: Disappearance of symptoms (35.6), Lack of insight (25.6), Missing family (18.9), Economic problem (12.2), Fear of other patients (10) Hospital condition: Boredom from ward environment (16.7), Anger over given treatment (8.9), Lack of trust to the doctor (3.3), Lack of satisfaction with staff behavior (4.4), other (8.9) |
41.7 | 403 (34.4) | psychiatric wards patients- 1171 | Sari | 23 |
|
Patient- related reasons: Feeling complete recovery (45.4), Transferring to another hospital (15.1), The patient’s personal reasons (5.8), Going to home (4.5), Financial problems (1.3) Hospital condition: Lack of required facilities (7.3), Not paying full and close attention to the patients (5.1), Hospital intolerance (3.1), Prolonged treatment process (2.8), Dissatisfaction with the hospital (2.8), Lack of required special medical services (1.7), Overcrowding in the unit and department (1.5) |
65.3 | 2601 (14) | General patients- 18518 | Tehran | 24 |
|
Patient- related reasons: Perceived improvement of child illness (32.9), Financial problems (15.5), Hospital condition: Unsatisfactory treatment and care (29.9), Inconvenience for child hospitalization (18.6), not declared (3.1) |
56.7 | 97 (5.3) | Children- 1842 | Tehran | 20 |
| - | - | 31 (3.4) | psychiatric wards patients-908 | Tehran | 25 |
| - | 61 | 121 (5.6) | Emergency Department- 2161 | Kerman | 27 |
| Hospital condition: Dissatisfaction from physician (33), Advice of the doctor (27.5), Lack of required facilities (12.7), Dissatisfaction from nurses (9.3), unsuitable environment (6.6), hospital cost (3.6), others (3.9) | 65.3 | 330 (8.2) | General patients- 4017 | Ghazvin | 31 |
| Patient- related reasons: Feeling of recovery (12), Personal reason (13.9), Transportation (7.5), Follow up (0.9), Unknown (65.7) | 52.7 | 108 (2.2) | Children- 4835 | Sari | 26 |
|
Patient- related reasons: Feeling better (47.1), Financial problems (4), Referring to a private center (10.5), Referring to certain centers due to personal ties (7.5) Hospital condition: Oral statements of physicians regarding improved conditions (9.2), No ICU bed (2), No CCU bed (1.1), No inpatient bed (2.1), Lack of appropriate specialty (2.7), Advice of the doctor and staff to refer to other centers (4.6), Unaccountability of the physician and the staff (3.1), Poor attendance (0.8), Over-crowding and insufficient care (1.4), Dissatisfaction with the course of treatment (3.3) |
58.4 | 1502 (13.3) | Emergency Department-13309 | Tehran | 32 |
|
Patient- related reasons: Lack of consent to surgery or invasive procedures (30.8), Personal or family issues (16.8), Feeling well (12.9), Financial problems (11.1), Desire to be transferred to another hospital (10.1), Requesting temporary leave from hospital stay during public or extended holidays (2.9), No noticeable improvements (5.9), No reason mentioned (2.8) Hospital condition: Dissatisfaction with hospital services/facilities (2.3), Seeking consultation elsewhere (1.4), Delay in delivery of health care services (0.8), Dissatisfaction with the staff’s behavior (0.7), Other reasons (1.5) |
59.5 | 992 (4.9) | In patients with Heart Disease- 20289 | Tehran | 9 |
| - | 56.3 | 860 (9) | General patients- 9463 | Shiraz | 10 |
| - | 51.1 | 7967 (8.4) | General patients-94441 | Mazandaran | 30 |
|
Patient- related reasons: Feeling better (78), Tendency to refer to a better center (7.7), Not having tendency to hospitalization (8.9) Hospital condition: Lack of expert physicians (0.3), Lack of suitable services (2), Ward being over crowded (2.3), Need to hospitalization in special units such as ITU or CCU (2.1), other (1.3) |
67.3 | 1516 (11.8) | Emergency Department- 12843 | Tehran | 29 |
| - | - | 178 (20.2) | emergency department-880 | Tehran | 19 |
”Patient- related reasons” and ”Hospital condition” are two main them of DAMA cause
The rates of DAMA in terms of these groups are provided in Table 2. While the highest rate of DAMA is associated with patients in departments of psychiatry, the lowest rate is related to patients in departments of pediatrics.
Table 2:
Discharge against medical advice rate in Iranian hospital according to study groups
| Q-value | I2 | df | Upper and Lower limit (%) | DAMA rate (%) | Groups |
|---|---|---|---|---|---|
| 1320 | 99.4 | 7 | [6 9.6] | 7.6 | General patients and cardiac patients |
| 148 | 97.9 | 3 | [9.1 15.1] | 11.8 | Emergency Department patients |
| 51 | 96 | 2 | [2.4 5.5] | 3.7 | Children |
| 1195 | 99.4 | 1 | [10 65] | 12 | psychiatric wards patients |
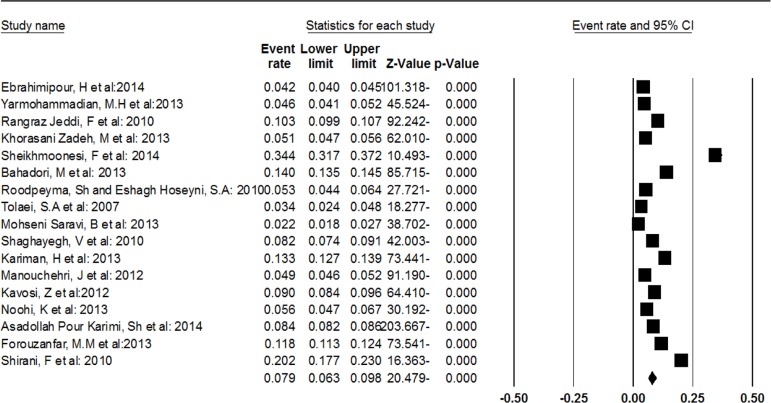
In general, using a random effects model, the rate of DAMA in Iranian hospitals was estimated at 7.9% (Fig. 2). (DAMA=7.9% [6.3% 9.8%], df =16 I2= 99.5, Q= 3613.9).
Fig. 2:
The rate of discharge against medical advice in Iranian hospitals using a random effects model
In the current study, a funnel plot was used to examine the publication bias in reviewed studies (Fig. 3). The results of this figure show that there is the possibility of risk of publication bias.
Fig. 3:
The funnel plot to examine the possibility of the publication bias
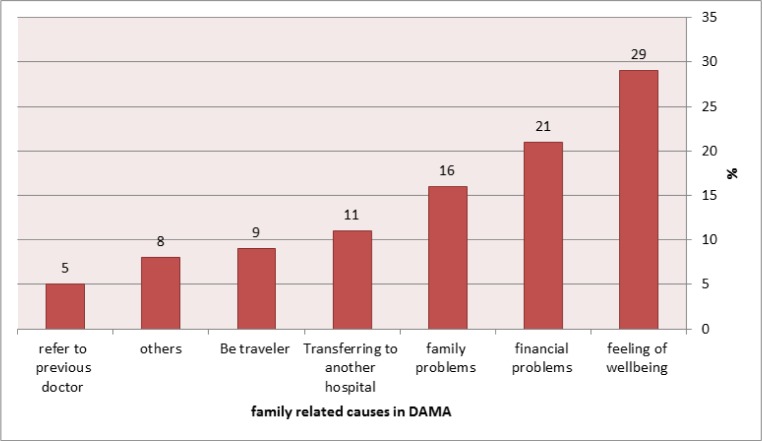
Using content analysis, causes contributing of DAMA were categorized into two main categories: causes related to patient and his/her family and hospital-related causes. The most important causes in each category, in terms of their priority, are presented in Fig. 4 and 5. As Fig. 4 shows, among causes related to patient and his/her family, “patient’s perception of feeling of wellbeing” (29%), “financial problems” (21%) and “family problems” (16%) were considered as the most important causes, whereas among hospital related causes.
Fig. 4:
The most important patient and family related causes contributing to discharge against medical advice
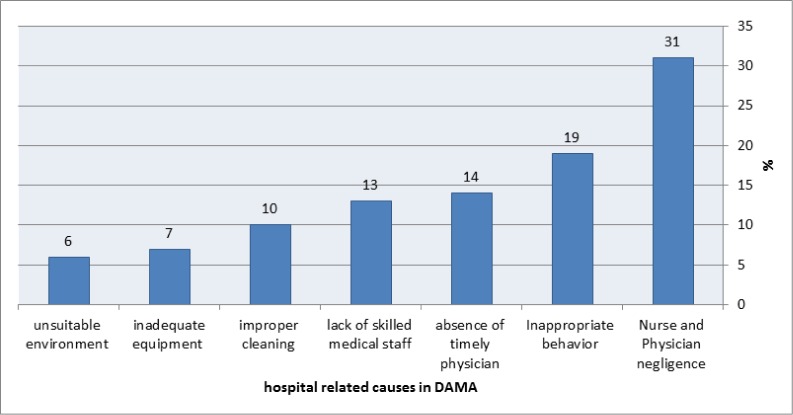
Fig. 5:
The most important hospital related causes contributing to discharge against medical advice
As Fig. 5 shows, among hospital related causes “lack of attention from physicians and nurses” (31%), “inappropriate behavior by hospital team” (19%) and “absences timely physician” (14%) were regarded as the most important causes in DAMA.
Discussion
The results of the current study showed that the rate of DAMA in Iranian hospitals is 7.9%. The most important causes contributing to DAMA included patient’s perception of feeling of wellbeing, financial problems, the lack of attention from physicians and nurses as well as inappropriate behavior by hospital team.
The rate of DAMA in Iranian hospitals is too high in comparison with many studies conducted in developed countries (11, 33–37). One of the possible reasons for this issue can be high quality services in hospitals of developed countries. As the results of the review of studies conducted in Iran showed, hospital related causes (such as the lack of attention from physicians and nurses, inappropriate behavior by hospital team, improper equipment and environment) are the most important reasons for DAMA. So, paying more attention to the improvement of the quality of services provided to patients in Iranian hospitals and in particular, special focusing on the hospital related causes mentioned in this study, are necessary.
According to the results, the rate of DAMA among patients in departments of psychiatry has been higher than those of other patients and such a higher rate has been also reported in previous studies (38–42). Given the nature of the disease of this group of patients which extends average length of stay in hospital, these patients tend more to DAMA due to the perception of feeling of wellbeing, boring hospital environment and financial problems. Another possible reason may stem from cultural issues, because mental illness is considered as a social stigma and an unpleasant phenomenon from social and family perspectives in Iran. Most patients and their families, therefore, tend to early discharge from hospital, so that their relatives and others close to them do not become aware of the hospitalization. It is, therefore, important to pay more attention to and focus on this group of patients.
Besides, the rate of DAMA among children was less than other patients. The results of some studies also indicated the low rate of DAMA in departments of pediatrics (2, 4, 43). Main reasons for this issue may be the lack of decision-making authority of children and parents’ worries for their children’s health. Therefore, they try to solve financial problems anyway and the treatment of their children will be continued until full recovery is made and patient can be discharged based on physicians’ orders. Moreover, the rate of DAMA among children is less because they do not work and are less affected by family problems.
The rate of DAMA in emergency departments in Iranian hospitals was estimated at 11.8%. In comparison with results of most studies conducted in emergency departments, this rate is higher (44, 45). One of the main reasons for this issue may be overcrowding in emergency departments in Iran, because all 4 studies conducted in emergency departments in Iran were done in reference hospitals which are usually overcrowded. Thus increasing the space, facilities and human resources working in these departments can be effective in reducing the rate of DAMA.
The results showed that DAMA was in men more than women, and this result had been shown in previous studies (46–48). The reason of low rate of discharge in women than men could be because of their more cautious and fear. Male discharge against medical advice was higher than female. It may be due to men job and their responsibility to make a living which forces them to go back home sooner, also; their early recovery feeling in compared with women due to their physiology and masculine nature.
In this study, the main reasons for DAMA were categorized into two main categories: causes related to patient and his/her family and hospital-related causes. In general, patient’s perception of feeling of wellbeing, financial problems, the lack of attention from physicians and nurses as well as inappropriate behavior by hospital team were considered as four main causes contributing to DAMA. In this regard, results of a study conducted by Alibis and Rami also pointed to dissatisfaction with treatment trends, financial and family problems, patient’s perception of feeling of wellbeing, preferring other hospitals, dissatisfaction with hospital environment, inadequate treatment and being a teaching hospital (49). In many studies conducted in other countries, the relationships between causes such as insurance status, socioeconomic status, patient history as well as other similar causes and DAMA were also investigated (50–53). However, unfortunately many of these causes have not been paid enough attention by researchers in Iran. Further research, therefore, should investigate the relationship between various variables regarding DAMA.
Different studies throughout the world have addressed impacts of DAMA such as costs, readmissions, deaths and morbidities (6, 12, 54–62). Such issues regarding patients discharged from Iranian hospitals have not been addressed in studies which may be primarily due to the poor information system in Iranian hospitals. Given the importance of the issue, the investigation of results and impacts of DAMA in Iranian hospitals is considered as an inevitable necessity.
Time is another issue related to studies on DAMA conducted in Iran, so that all studies have conducted from 2010 and in our search results, no study was found which had been published before that time. The introduction of Clinical Governance in Iran can be considered as a possible reason for this issue, because during the indicated time interval which most studies have been conducted, clinical governance model has been implemented in Iranian hospitals (63). Through implementing this model with special emphasis on DAMA, a great attention has been paid to DAMA forms. If this assumption is true, then we can argue that implementing models similar to the clinical governance can be effective in this area. Fortunately, in recent year, Iranian hospitals’ accreditation standards include great attention to the issue of DAMA which requires careful attention in order to successfully implement it and achieve excellent results in this field.
Despite the efforts of authors, the lack of access to some theses and hospital reports on DAMA can be mentioned as a limitation of this study.
Conclusion
The rate of DAMA in Iranian hospitals in comparison with those of other countries is relatively high; thus effective initiatives in this area are required. In addition, patient’s perception of feeling of wellbeing, financial problems, the lack of attention from physicians and nurses as well as inappropriate behavior by hospital team were mentioned as main reasons for DAMA. These causes can be given high priority in plans for quality improvement and reducing DAMA. Furthermore, given the limited studies conducted in Iran and the lack of investigation into some variables contributing to DAMA and also impacts of DAMA in Iranian hospitals, more research is needed in this area.
Ethical Considerations
All ethical issues including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the author.
Acknowledgment
We would like to specially thank Masjid Nakhaei and Ahmad Negahban for sincerely critical comments in the present study. The authors declare that there is no conflict of interests.
References
- 1. Fiscella K, Meldrum S, Barnett S. (2007). Hospital discharge against advice after myocardial infarction: deaths and readmissions. Am J Med, 120: 1047–1053. [DOI] [PubMed] [Google Scholar]
- 2. Muna Al-Sadoon M, Al-Shamousi K. (2013). Discharge against Medical Advice among Children in Oman. A university hospital experience. Sultan Qaboos University Med J, 13: 534–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Taqueti V. (2007). Leaving against medical advice. N Engl J Med, 357: 213–215. [DOI] [PubMed] [Google Scholar]
- 4. Okoromah CN, Egri-Qkwaji MT. (2004). Profile of and control measures for paediatric discharges against medical advice. Niger Postgrad Med J, 11: 64–7. [PubMed] [Google Scholar]
- 5. Duno R, Pousa E, Sans J, Tolosa C, Ruiz A. (2003). Discharge against medical advice at a general hospital in Catalonia. Gen Hosp Psychiatry, 25: 46–50. [DOI] [PubMed] [Google Scholar]
- 6. Baptist A, Warrier I, Arora R, Ager J, Massanari M. (2007). Hospitalized patients with asthma who leave against medical advice: Characteristics, reasons and outcomes. J Allergy Clinl Immunol 119: 924–929. [DOI] [PubMed] [Google Scholar]
- 7. Saitz R, Ghali W, Moskowitz M. (2000). The impact of leaving against medical advice on hospital resource utilization. J Gen Intern Med, 15: 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rangraz Jeddi F, Rangraz Jeddi M, Rezaeiimofrad M. (2010). Patients’ Reasons for Discharge against Medical Advice in University Hospitals of Kashan University of Medical Sciences in 2008. Hakim Res J, 13: 33–39. [Google Scholar]
- 9. Manouchehri J, Goodarzynejad H, Khoshgoftar Z, Sheikh Fathollahi M, Aghamohammadi Abyaneh M. (2012). Discharge against Medical Advice among Inpatients with Heart Disease in Iran. J Teh Univ Heart Ctr 7: 72–77. [PMC free article] [PubMed] [Google Scholar]
- 10. Kavosi Z, Hatam N, Hayati Abbarik H, Nemati J, Bayati M. (2012). Factors Affecting Discharge against Medical Advice in a Teaching Hospital in Shiraz, Iran. Health Information Management, 9: 448–456. [Google Scholar]
- 11. Ibrahim S, Kwoh K, Krishnan E. (2007). Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health, 97:2204–2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hwang S, Li J, Gupta R, Chien V, Martin R. (2003). What happens to patients who leave hospital against medical advice? CMAJ, 168: 417–420. [PMC free article] [PubMed] [Google Scholar]
- 13. Choi M, Kim H, Qian H, Palepu A. (2011). Readmission rates of patients discharged against medical advice: a matched cohort study. PLoS ONE, 6: e24459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alfandre D. (2009). “I’m going home”: discharges against medical advice. Mayo Clin Proc, 84: 255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Seaborn Moyse H, Osmun W. (2004). Discharges against medical advice: A community hospital’s experience. Can J Rural Med, 9: 148–153. [PubMed] [Google Scholar]
- 16. Macrohon B. (2012). Pediatrician’s perspectives on discharge against medical advice (DAMA) among pediatric patients: A qualitative study. BMC Pediatr, 18: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sadeghi-Bazargani H, Tabrizi JS, Azami-Aghdash S. (2014). Barriers to evidence-based medicine: a systematic review. Journal of Evaluation in Clinical Practice. 20: 793–802. [DOI] [PubMed] [Google Scholar]
- 18. Ebrahimipour H, Meraji M, Hooshmand E, Nezamdoust F, Molavi-Taleghani Y, Hoseinzadeh N, Vafaee-Najar A. (2014). Factors Associated with Discharge of Children from Hospital Against Medical Advice (AMA) at Doctor Sheikh Pediatric Hospital (DSPH) in Mashhad: 2011–2013. World J Med Scie, 11: 196–201. [Google Scholar]
- 19. Shirani F, Jalili M, Asl-E-Soleimani H. (2010). Discharge against medical advice from emergency department: results from a tertiary care hospital in Tehran, Iran. Eur J Emerg Med, 17: 318–321. [DOI] [PubMed] [Google Scholar]
- 20. Roodpeyma S, Hoseyni S. (2010). Discharge of children from hospital against medical advice. World J Pediatr, 6: 353–356. [DOI] [PubMed] [Google Scholar]
- 21. Yarmohammadian M, Mojahed F, Vahidi R, Gholipour K, Shokri A, Rasi V. (2013). Clinical Audit of Self-Discharge against Medical Advice in Dr. Soulati Hospital in Urmia, Iran. Health Inf Manage, 9: 1006–1014. [Google Scholar]
- 22. Khorasani Zadeh M, Ebrahimi H. (2013). Evaluation of Patients’ Reasons for Discharge against Medical Advice in Shafa Hospital, Kerman, Iran. Health Inf Manage, 10:403–410. [Google Scholar]
- 23. Sheikhmoonesi F, Khademloo M, Pazhuheshgar S. (2014). Patients discharged against medical advice from a psychiatric hospital in Iran: a prospective study. Glob J Health Sci, 6: 213–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bahadori M, Raadabadi M, Salimi M, Ravangard R. (2013). Discharge against medical advice: a case study in a public teaching hospital in Tehran, Iran in 2012. Glob J Health Sci, 5: 179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tavallaei S, Asari S, Habibi M, Khodami H, Siavoshi Y, Nouhi S, et al. (2006). Discharge Against Medical Active from Psychiatric Ward. J Mil Med, 8: 24–30. [Google Scholar]
- 26. Mohseni Saravi B, Reza Zadeh E, Siamian H, Yahghoobian M. (2013). Discharge Against Medical Advice in the Pediatric Wards in Booali Sina Hospital, Sari, Iran 2010. Acta Inform Med, 21: 253–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Noohi K, Komsari S, Nakhaee N, Yazdi Feyzabadi V. (2013). Reasons for Discharge against Medical Advice: A Case Study of Emergency Departments in Iran. Int J Health Policy Manag, 1: 137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Karimi SA, Saravi BM, Farahabbadi EB, Zamanfar D, Fallah M, Abokheily MA. (2014). Studying the rate and causes of discharge against medical advice in hospitals affiliated to mazandaran university of medical sciences. Mater Sociomed, 26: 203–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Forouzanfar MM, Hashemi B, Baratloo A, Arhamodolatabadi A, Hatamabadi H, Shahrami A, Safari S. (2013). Discharge against medical advice in emergency department of a general hospital in Tehran. Intl Res J Appl Basic Sci, 5: 1487–1490. [Google Scholar]
- 30. Asadollah Pour Karimi S, Mohseni Saravi B, Bagherian Farahabbadi E, Zamanfar D, Fallah M, Asadi Abokheily MA. (2014). Studying the Rate and Causes of Discharge Against Medical Advice in Hospitals Affiliated to Mazandaran University of Medical Sciences. Mater Sociomed, 26: 203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vahdat S, Hesam S, Mehrabian F. (2010). Effective factors on patient discharge with own agreement in selected Therapeutic Training Centers of Ghazvin Shahid Rajaei. The J Nurs Midw Facul Guilan Med Uni, 20: 47–52. [Google Scholar]
- 32. Kariman H, Khazaei A, Shahrami A, Hatamabadi HR. (2013). Dealing with Discharge against Medical Advice in Emergency Department. J Basic Appl Sci Res, 3: 785–791. [Google Scholar]
- 33. Alfandre DJ. (2008). “I’m going home”: discharges against medical advice. J La State Med Soc, 160: 343–7. 19283983 [Google Scholar]
- 34. Saitz R. (2002). Discharges against medical advice: time to address the causes. Prehosp Emerg Care, 6: 391–5. [PMC free article] [PubMed] [Google Scholar]
- 35. Al-Turkistani HK. (2013). Discharge against medical advice from Neonatal Intensive Care Unit: 10 years experience at a University Hospital. J Family Community Med, 20: 113–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fiscella K, Meldrum S, Barnett S. (2007). Hospital discharge against advice after myocardial infarction: deaths and readmissions. Niger J Clin Pract, 10: 200–4. [DOI] [PubMed] [Google Scholar]
- 37. Ohanaka E. (2002). Discharge against medical advice. Trop Doct, 32: 149–151. [DOI] [PubMed] [Google Scholar]
- 38. Brook M, Hilty DM, Liu W, Hu R, Frye MA. (2006). Discharge against medical advice from inpatient psychiatric treatment: a literature review. Emerg Med Clin North Am, 24: 733–47. [DOI] [PubMed] [Google Scholar]
- 39. Hayat AA, Ahmed MM, Minhas FA. (2013). Patients leaving against medical advice: an inpatient psychiatric hospital-based study. J Coll Physicians Surg Pak, 23: 342–6. [PubMed] [Google Scholar]
- 40. Levine LJ, Schwarz DF, Argon J, Mandell DS, Feudtner C. (2005). Discharge disposition of adolescents admitted to medical hospitals after attempting suicide. Scott Med J, 50: 114–7. [DOI] [PubMed] [Google Scholar]
- 41. Tuckman J, Lavell M. (1963). Psychiatric patients discharged with or against medical advice. Arch Gen Psychiatr, 8: 131–8. [DOI] [PubMed] [Google Scholar]
- 42. Akhtar S, Wood G, Rubin JS, O’Flynn PE, Ratcliffe P. (1999). Effect of caffeine on the vocal folds: a pilot study. Schweiz Med Wochenschr, 129: 1535–44. [DOI] [PubMed] [Google Scholar]
- 43. Ibekwe RC, Muoneke VU, Nnebe-Agumadu UH, Amadife MA. (2008). Factors influencincing discharge against medical advice among paediatric patients in Abakaliki, Southeastern Nigeria. Crisis, 29: 213–5. [DOI] [PubMed] [Google Scholar]
- 44. Choi QJ, Hwang SI, Kim SY. (2009). Patients leaving against medical advice (AMA) from the emergency department-disease prevalence and willingness to return. Uisahak, 18: 157–72. [DOI] [PubMed] [Google Scholar]
- 45. Ding R, Jung JJ, Kirsch TD, Levy F, McCarthy ML. (2008). Uncompleted emergency department care: patients who leave against medical advice. Disabil Rehabil, 30: 863–70. [DOI] [PubMed] [Google Scholar]
- 46. Akiode O, Musa A, Shonubi A, Salami B, Oyelekan A. (2005). Trends of discharges against medical advice in a suburban surgical practice in Nigeria. Trop Doct, 35: 51–2. [PubMed] [Google Scholar]
- 47. Ohanaka E. (2002). Discharge against medical advice. Trop Doct, 32: 149–51. [DOI] [PubMed] [Google Scholar]
- 48. Nasir A, BO (2008). Clinical spectrum of discharges against medical advice in a developing country. Indian J Surg, 70: 68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Alebiosu CO, Raimi TH. (2003). Discharge against medical advice. J Obstet Gynaecol, 23: 397–401. [DOI] [PubMed] [Google Scholar]
- 50. Cheng KD, Huang CJ, Tsang HY, Lin CH. (2014). Factors related to missed first appointments after discharge among patients with schizophrenia in Taiwan. J Formos Med Assoc, 113: 436–41. [DOI] [PubMed] [Google Scholar]
- 51. Weingart SN, Davis RB, Phillips RS. (1998). Patients discharged against medical advice from a general medicine service. Psychiatr Serv, 49: 1187–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Taqueti VR. (2007). Leaving against medical advice. Gesundheitswesen, 69: 371–6. [DOI] [PubMed] [Google Scholar]
- 53. Sulstarova B, Poglia Mileti F, Mellini L, Villani M, Singy P. (2014). HIV disclosure and nondisclosure among migrant women from sub-Saharan Africa living in Switzerland. AIDS Care, 8: 1–7. [DOI] [PubMed] [Google Scholar]
- 54. Miller CD, Hwang W, Hoekstra JW, Case D, Lefebvre C, Blumstein H, Hiestand B, Diercks DB, Hamilton CA, Harper EN, Hundley WG. (2010). Discharge of children from hospital against medical advice. Ann Emerg Med, 56: 209–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Anis A, Sun H, Guh D, Palepu A, Schechter M, O’Shaughnessy M. (2002). Leaving hospital against medical advice among HIV-positive patients. CMAJ, 167: 633–637. [PMC free article] [PubMed] [Google Scholar]
- 56. Abramowitz MZ, Bentov-Gofrit D, Khawaled R, Bauer A, Cohen T. (2011). Readmission rates of patients discharged against medical advice: a matched cohort study. Int J Law Psychiatry, 34: 368–73. [DOI] [PubMed] [Google Scholar]
- 57. Aliyu ZY. (2002). Discharge against medical advice: sociodemographic, clinical and financial perspectives. Cochrane Database Syst Rev, 3. [PubMed] [Google Scholar]
- 58. Aujesky D, Mor MK, Geng M, Stone RA, Fine MJ, Ibrahim SA. (2009). Predictors of early hospital readmission after acute pulmonary embolism. Neuro Rehabilitation, 24: 67–74. [DOI] [PubMed] [Google Scholar]
- 59. Edwards J, Markert R, Bricker D. (2013). Discharge against medical advice: how often do we intervene? J Hosp Med, 8: 574–7. [DOI] [PubMed] [Google Scholar]
- 60. Garland A, Ramsey CD, Fransoo R, Olafson K, Chateau D, Yogendran M, Kraut A. (2013). Rates of readmission and death associated with leaving hospital against medical advice: a population-based study. CMAJ, 185: 1207–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Glasgow J, Vaughn-Sarrazin M, Kaboli P. (2010). Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med 25: 926–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hogele AM, Neu J. (2011). Readmissions after unauthorized discharges in the cardiovascular setting. Unfallchirurg, 114: 70–2. [DOI] [PubMed] [Google Scholar]
- 63. Sadeghi-Bazargani H, Saadati M, Tabrizi JS, Jannati A, Pourasghar F, Ghasemi B, Ebadi A, Mirzaie A, Abedi L, Azami-Aghdash S. (2014). Tabriz Clinical Governance Research Project (TCGRP): Study Protocol. J Clin Res Govern, 3: 76–80. [Google Scholar]