Abstract
Background
Before 2007, U.S.-bound immigrants and refugees were screened for tuberculosis (TB) by a smear-based algorithm that could not diagnose smear-negative and culture-positive TB. In 2007, the Centers for Disease Control and Prevention began to implement a culture-based algorithm.
Objective
To evaluate the effect of the culture-based algorithm on preventing the importation of TB to the United States by immigrants and refugees from foreign countries.
Design
Population-based, cross-sectional study.
Setting
Panel physician sites for overseas medical examination.
Patients
Immigrants and refugees with TB.
Measurements
Comparison of the increase of smear-negative and culture-positive TB cases diagnosed overseas among immigrants and refugees by the culture-based algorithm with the decline of reported TB cases among foreign-born persons within 1 year after arrival in the United States from 2007 to 2012.
Results
Of the 3 212 421 arrivals of immigrants and refugees from 2007 to 2012, 1 650 961 (51.4%) were screened by the smear-based algorithm and 1 561 460 (48.6%) were screened by the culture-based algorithm. Among the 4032 TB cases diagnosed by the culture-based algorithm, 2195 (54.4%) were smear-negative and culture-positive. Before implementation (2002 to 2006), the annual number of reported TB cases among foreign-born persons within 1 year after arrival was relatively constant (range, 1424 to 1626 cases; mean, 1504 cases) but decreased from 1511 to 940 cases during implementation (2007 to 2012). During the same period, the annual number of smear-negative and culture-positive TB cases diagnosed overseas among U.S.-bound immigrants and refugees by the culture-based algorithm increased from 4 in 2007 to 629 in 2012.
Limitation
This analysis did not control for the decline in new arrivals of nonimmigrant visitors to the United States and the decrease of incidence of TB in their countries of origin.
Conclusion
Implementation of the culture-based algorithm in U.S.-bound immigrants and refugees may have substantially reduced the incidence of TB among newly arrived, foreign-born persons in the United States.
Primary Funding Source
None.
Immigration has a substantial effect on the incidence of tuberculosis (TB) in the United States (1, 2). In 2013, 6172 (64.4%) of the 9588 new TB cases reported in the United States were among foreign-born persons (3). To reduce the incidence of TB in the United States, U.S.-bound immigrants and refugees are required to have overseas TB screening (1). Before 2007, overseas TB screening was limited to chest radiography and the use of a smear-based algorithm (acid-fast bacilli smears of 3 consecutive sputum samples from persons with abnormal chest radiographs) (4). Although smear-based screening for TB overseas with follow-up evaluation was a relatively high-yield intervention for preventing TB in U.S.-bound immigrants and refugees (5, 6), studies showed a likely advantage of including the Mycobacterium tuberculosis culture in overseas screening (7, 8). Of 183 U.S.-bound immigrants in Vietnam whose M. tuberculosis culture was positive, 120 (65.6%) had a smear that was negative for acid-fast bacilli (7). Overseas screening with M. tuberculosis culture substantially reduced the TB incidence rate among newly arrived Hmong refugees in the United States (8).
In 2007, the Centers for Disease Control and Prevention (CDC) revised the smear-based screening algorithm to include the M. tuberculosis culture, drug-susceptibility testing, and directly observed therapy for TB treatment (9, 10). Because of the importance in identifying and treating latent TB infection (2), the new culture-based screening algorithm also required latent TB infection screening for persons aged 2 to 14 years in countries with a World Health Organization (WHO)–estimated incidence of TB of 20 cases or greater per 100 000 persons per year. The culture-based algorithm was first implemented in Thailand (April 2007) and then in Mexico, the Philippines, Belize, and Qatar (October 2007). It had been implemented in 81 countries as of December 2012 and in all countries in October 2013 (11).
A recent study of newly arrived immigrants and refugees in California showed that fewer TB cases were imported from countries where the culture-based algorithm had been implemented (12). A preliminary analysis at the CDC showed that smear-negative and culture-positive TB accounted for approximately 60.0% of the 1100 TB cases diagnosed overseas among U.S.-bound immigrants and refugees by the culture-based algorithm in 2012 (13). We analyzed a national data set from the CDC to evaluate the effect of implementing the culture-based algorithm in U.S.-bound immigrants and refugees from 2007 to 2012.
Methods
Study Population
The study population included immigrants and refugees who were initially screened for TB overseas between 2007 and 2012 and arrived in the United States before 1 May 2014, the date that we obtained the final data set for the analysis. Data about TB diagnoses from overseas screening and follow-up evaluation after arrival in the United States and about refugee arrivals were obtained from the CDC’s Electronic Disease Notification (EDN) database. Summary data of immigrant arrivals (by arrival year, birth country, sex, and age) came from the U.S. Department of Homeland Security. For comparison, we also obtained the annual number of reported TB cases among foreign-born persons within 1 year after arrival from the National Tuberculosis Surveillance System between 2002 and 2012 (14–16).
Overseas TB Screening
Overseas medical examination is required for all U.S.-bound immigrants and refugees, and TB screening is a major component of the examination. Overseas medical examination is performed by 400 to 800 panel physicians, licensed local physicians who are appointed by the U.S. embassies and consulates (5, 17). The CDC provides technical guidance and oversight to the panel physicians. Before 2007, overseas TB screening was based on a smear-based algorithm that consisted of standard posteroanterior radiography of the chest for persons aged 15 years or older; in the case of persons with chest radiographs suggestive of active TB or with symptoms of TB, sputum specimens were collected on 3 consecutive days and stained for acid-fast bacilli (4). The smear-based algorithm classified persons as class A TB if chest radiographs were suggestive of active TB and 1 or more sputum smears were positive for acid-fast bacilli, class B1 TB if chest radiographs were suggestive of active TB and sputum smears were negative for acid-fast bacilli on 3 consecutive days, class B2 TB if chest radiographs were suggestive of TB that was not clinically active (such as showing fibrosis, scarring, pleural thickening, diaphragmatic tenting, or blunting of costophrenic angles), or no TB if chest radiographs were normal (Table 1). Appendix Figure 1 (available at www.annals.org) demonstrates the smear-based algorithm.
Table.
TB Classifications Used by the Smear- and Culture-Based Algorithms
| TB Classification | Smear-Based Algorithm | Culture-Based Algorithm |
|---|---|---|
| Class A | ≥1 sputum smear results were positive. Persons diagnosed with class A TB had to complete TB treatment overseas and would be reclassified as having class B2 TB. | ≥1 sputum smear or culture results were positive or TB was clinically diagnosed. Persons diagnosed with class A TB had to complete directly observed therapy for TB overseas and would be reclassified as having class B1 TB. |
| Class A TB waiver: Persons with class A TB received TB treatment overseas until their sputum smear results became negative and applied for an immigration waiver. A class A TB waiver is rare. Follow-up evaluation after arrival in the United States is mandated for persons with a class A TB waiver. | Class A TB waiver: Persons with class A TB received directly observed therapy until their sputum smear and culture results became negative and applied for an immigration waiver. A class A TB waiver is rare. Follow-up evaluation after arrival in the United States is mandated for persons with a class A TB waiver. | |
|
| ||
| Class B1 | Chest radiograph suggestive of active TB | Chest radiograph, medical history, or examination suggestive of TB |
|
| ||
| Class B2 | Chest radiograph suggestive of inactive TB | NA |
|
| ||
| Class B2 latent TB infection | NA | Induration of ≥ 10 mm on TST or positive results on an IGRA |
|
| ||
| No TB | Normal chest radiograph | Normal chest radiograph |
IGRA = interferon-γ release assay; NA = not applicable; TB = tuberculosis; TST = tuberculin skin test.
As a result of methodological research (7, 8), the CDC formally revised the smear-based algorithm in 2007 to include the M. tuberculosis culture for those identified with class B1 or B2 TB by the smear-based algorithm (9, 10). The new culture-based algorithm also required persons aged 2 to 14 years in countries with a WHO-estimated incidence of TB of 20 cases or greater per 100 000 persons per year to have screening for latent M. tuberculosis infection. The culture-based algorithm classified persons as class A TB if chest radiographs were suggestive of TB disease and 1 or more sputum smears or mycobacterial cultures were positive, class B1 TB if chest radiographs were suggestive of TB disease and both sputum smears and mycobacterial cultures were negative, class B2 latent TB infection if chest radiographs were normal but the tuberculin skin test was 10 mm or greater or the interferon-γ release assay was positive, or no TB if the person had no signs or symptoms of TB and chest radiographs were normal. For persons screened for latent TB infection, their tuberculin skin test or interferon-γ release assay results were negative (Table 1). Appendix Figure 2 (available at www.annals.org) demonstrates the culture-based algorithm. Persons with class A TB had to complete overseas TB treatment, and directly observed therapy was required for those screened by the culture-based algorithm.
Persons could apply for an immigration waiver after their smears became negative (for those screened by smear-based algorithm) or both their smears and cultures became negative (for those screened by the culture-based algorithm) (4, 5, 10). Class A TB waivers were rare. The smear-based algorithm reclassified persons who completed overseas TB treatment as class B2 TB, and the culture-based algorithm reclassified persons who completed directly observed therapy for TB as class B1 TB (4, 10).
For persons diagnosed with TB disease overseas by the smear-based algorithm, their medical examination forms did not require panel physicians to provide information about their TB diagnosis and treatment. However, for those diagnosed with TB disease by the culture-based algorithm, the newly revised medical examination forms recorded their TB diagnosis and treatment. We classified persons who were diagnosed with TB disease by the culture-based algorithm and completed overseas TB treatment as smear-positive and culture-positive TB, smear-positive and culture-negative TB, smear-negative and culture-positive TB, or clinically diagnosed TB. Because overseas drug-susceptibility testing was not systematically reported on the overseas medical examination forms between 2007 and 2012, we could not calculate prevalence of multidrug-resistant TB and study the pattern of drug resistance among U.S.-bound immigrants and refugees.
Follow-up Evaluation After Arrival in the United States
Persons with a class A TB waiver were mandated to report to health departments for follow-up evaluation after arrival. Through its EDN database, the CDC notified state and local health departments about arriving immigrants and refugees identified with class B1 or B2 TB by the smear-based algorithm and those identified with class B1 TB or class B2 latent TB infection by the culture-based algorithm. Health department physicians were asked to conduct a follow-up evaluation, assign a TB diagnosis after arrival, and complete the follow-up evaluation worksheet (5). Follow-up evaluation data were entered into the CDC’s EDN database by state or local health departments.
Ethical Review
The study protocol was reviewed for human subject concerns by the CDC and found to be consistent with the CDC’s public health surveillance activities and not human subject research; therefore, review by an institutional review board was not required.
Statistical Analysis
Estimation of the Number of Immigrants Screened by the Culture-Based Algorithm [level 3] The CDC’s EDN database collected information about overseas medical examination for all refugees and immigrants with medical conditions. To estimate the number of immigrants screened by the culture-based algorithm from 2007 to 2012, we assumed that the number of immigrants screened overseas was equal to the number of immigrant arrivals during a specific year, and the number of immigrant arrivals was uniformly distributed by month within a specific year. For example, the implementation date was 1 October 2007 for Mexico and the number of Mexican immigrants screened by the culture-based algorithm was estimated as 25.0% of arrivals in 2007 (average arrivals in 3 months, October to December) and 100% of arrivals to 2008 to 2012.
Evaluation of the Effect of Implementing the Culture-Based Algorithm
We described the progress of implementing the culture-based algorithm and calculated the prevalence of TB for persons screened by the culture-based algorithm. We also calculated the proportions of active TB diagnosed among newly arrived immigrants and refugees with class B1 or B2 TB by follow-up evaluation in the United States.
Had the culture-based algorithm not been implemented, cases of smear-negative and culture-positive TB among U.S.-bound immigrants and refugees would have been imported to the United States and would likely have been reported as TB cases among newly arrived, foreign-born persons in the U.S. National Tuberculosis Surveillance System. By applying the mean of the annual number of reported TB cases among foreign-born persons within 1 year after arrival before implementation (2002 to 2006) as the baseline, we calculated the difference between the baseline and the annual number of reported TB cases among foreign-born persons within 1 year after arrival during implementation (2007 to 2012). We compared the cumulative sum of the differences with the total number of smear-negative and culture-positive TB cases diagnosed overseas among U.S.-bound immigrants and refugees by the culture-based algorithm during implementation.
Role of the Funding Source
The study did not receive external funding.
Results
Progress of Implementing the Culture-Based Algorithm
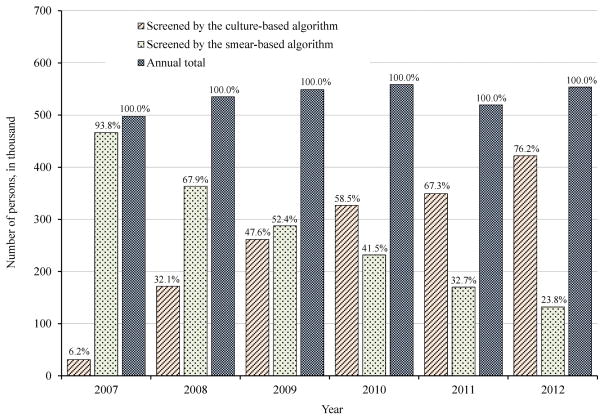
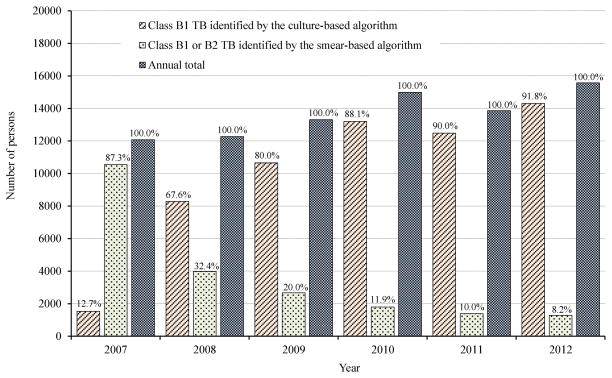
Of the 3 212 421 arrivals of immigrants and refugees between 2007 and 2012, 1 650 961 (51.4%) were screened by the smear-based algorithm and 1 561 460 (48.6%) were screened by the culture-based algorithm. The percentage of persons screened by the culture-based algorithm increased from 6.2% in 2007 to 76.2% in 2012 (Figure 1). As a result, the annual number of persons identified with class B1 TB by the culture-based algorithm increased from 1532 in 2007 to 14 292 in 2012 (Figure 2).
Figure 1.
U.S.-bound Immigrants and refugees who were screened for TB overseas by the smear-based algorithm or the culture-based algorithm, 2007–2012
Definitions: TB = Tuberculosis.
Figure 2.
U.S.-bound Immigrants and refugees identified with Class B1 or B2 TB by the smear-based algorithm, and those identified with Class B1 TB by the culture-based algortihm, 2007–2012
Definitions: TB = Tuberculosis.
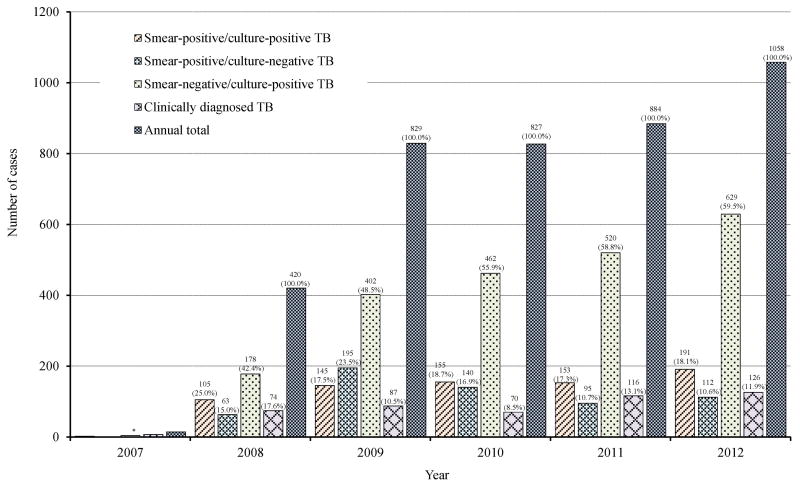
TB Cases Diagnosed Overseas by the Culture-Based Algorithm
Appendix Tables 1 and 2 (available at www.annals.org) show the results of overseas TB screening from 2007 to 2012. Data about TB cases diagnosed overseas by the smear-based algorithm were not reported to the CDC. The annual number of TB cases diagnosed overseas by the culture-based algorithm increased from 14 in 2007 to 1058 in 2012 (Figure 3). Among the 1 561 460 persons screened by the culture-based algorithm from 2007 to 2012, 4032 (258 cases per 100 000 persons) were diagnosed with TB: 751 (48 cases per 100 000 persons) with smear-positive and culture-positive TB, 606 (39 cases per 100 000 persons) with smear-positive and culture-negative TB, 2195 (141 cases per 100 000 persons) with smear-negative and culture-positive TB, and 480 (31 cases per 100 000 persons) with clinically diagnosed TB. Smear-negative and culture-positive TB accounted for 2195 (54.4%) of the 4032 TB cases diagnosed by the culture-based algorithm.
Figure 3.
TB cases diagnosed overseas among 1,561,460 U.S.-bound immigrants and refugees who were screened by the culture-based algorithm, 2007–2012
Definitions: TB = Tuberculosis.
* 14 cases of TB diagnosed in 2007: 2 (14.3%) cases of smear-positive/culture-positive TB, 1 (7.1%) cases of smear-positive/culture-negative TB, 4 (28.6%) cases of smear-negative/culture-positive TB, and 7 (50.0%) cases of clinically diagnosed TB.
Between 2007 and 2012, refugees made up only 14.9% of persons screened by the culture-based algorithm but accounted for 27.4% of TB cases diagnosed overseas among U.S.-bound immigrants and refugees. Of the 4032 TB cases diagnosed among U.S.-bound immigrants and refugees by the culture-based algorithm, 3757 (93.2%) were among persons in countries with a WHO-estimated incidence of TB of 100 cases or greater per 100 000 persons per year. The highest TB prevalence was among persons from Vietnam (890 cases per 100 000 persons) and the Philippines (854 cases per 100 000 persons).
Follow-up Evaluation After Arrival in the United States
Appendix Table 3 (available at www.annals.org) shows the results of follow-up evaluation. Of the 21 638 persons with class B1 or B2 TB identified by the smear-based algorithm, 11 686 (54.0%) completed follow-up evaluation in the United States. Among the 60 423 persons with class B1 TB identified by the culture-based algorithm, 40 896 (67.7%) completed follow-up evaluation. For persons who completed follow-up evaluation, active TB cases were diagnosed in 410 (3.5%) of the 11 686 persons screened by the smear-based algorithm and in 731 (1.8%) of the 40 896 persons screened by the culture-based algorithm (P < 0.001). In 2012, 1280 persons were identified with class B1 or B2 TB by the smear-based algorithm and 14 292 were identified with class B1 TB by the culture-based algorithm. If all persons with class B1 or B2 TB completed follow-up evaluation in 2012, 302 active TB cases were likely diagnosed in the United States (that is, 3.5% of 1280 plus 1.8% of 14 292).
Class B2 latent TB infection was identified in 41 167 (13.4%) of the 306 084 persons aged 2 to 14 years in countries with a WHO-estimated incidence of TB 20 cases or greater per 100 000 persons per year. Of the 41 167 persons with class B2 latent TB infection, 24 090 (58.5%) completed follow-up evaluation; of these, 79 (0.3%) were diagnosed with active TB.
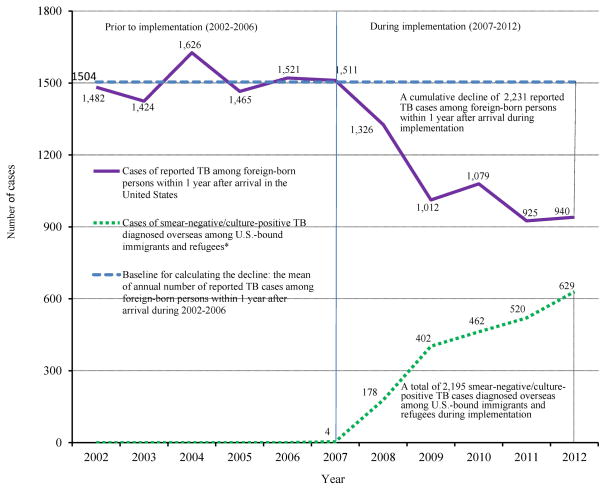
Effect of Implementing the Culture-Based Algorithm
Figure 4 shows the effect of implementing the culture-based algorithm. Before implementation (2002 to 2006), the annual number of reported cases among foreign-born persons within 1 year after arrival in the United States was relatively constant (range, 1424 to 1626 cases; mean, 1504 cases). During the implementation (2007 to 2012), the annual number of reported TB cases among foreign-born persons within 1 year after arrival decreased from 1511 in 2007 to 940 in 2012. During the same period, the annual number of smear-negative and culture-positive TB cases diagnosed overseas among U.S.-bound immigrants and refugees by the culture-based algorithm increased from 4 in 2007 to 629 in 2012. The cumulative decline of reported TB (2231 cases) among foreign-born persons within 1 year after arrival during implementation was similar to the total number of cases of smear-negative and culture-positive TB in U.S.-bound immigrants and refugees diagnosed overseas by the culture-based algorithm (2195 cases) during the same period.
Figure 4.
Comparison of reported TB cases among foreign-born persons within 1 year after arrival in the United States and smear-negative/culture-positive TB cases diagnosed overseas among U.S.-bound immigrants and refugees by the culture-based algorithm, 2002–2012
Definitions: TB = Tuberculosis.
* Had the culture-based algorithm not been implemented, cases of smear-negative/culture-positive TB would very likely have been imported to the United States and counted as reported cases among foreign-born persons within 1 year after arrival by the U.S. National TB Surveillance System.
Discussion
In the United States, screening immigrants and refugees for TB has been done for more than a century and continues to identify high TB incidence rates (18). Before 2007, the mandated overseas TB screening was based on a smear-based algorithm that could not diagnose smear-negative and culture-positive TB. In 2007, the CDC revised the smear-based algorithm to include the M. tuberculosis culture. From 2007 to 2012, the culture-based algorithm was preferentially implemented in countries with a high TB incidence. By increasing the number of TB cases diagnosed and treated overseas among U.S.-bound immigrants and refugees, the implementation of the culture-based algorithm contributed to the decline of foreign-born TB incidence in the United States. In 2012, the culture-based algorithm was used to screen 421 734 (76.2%) of the 553 563 U.S.-bound immigrants and refugees and diagnosed 1058 TB cases, including 629 cases of smear-negative and culture-positive TB. If the culture-based algorithm had not been implemented in any countries in 2012, these 629 smear-negative and culture-positive TB cases would have been imported to the United States.
Most TB cases diagnosed among U.S.-bound immigrants and refugees by the culture-based algorithm were among persons in countries with a high TB incidence. U.S.-bound refugees had a high incidence of TB. Despite only 50 000 to 70 000 annual arrivals, refugees contributed substantially to the TB burden among U.S.-bound immigrants and refugees.
In 2012, the U.S. National Tuberculosis Surveillance System reported 940 cases of TB among foreign-born persons within 1 year after arrival (16). In 2012, 15 572 immigrants and refugees had class B1 or B2 TB. If all of them completed follow-up evaluation after arrival in the United States, we estimated that 302 cases of TB would have been diagnosed in 2012. These 302 cases of TB estimated among newly arrived immigrants and refugees with class B1 or B2 TB accounted for 32.1% of the 940 reported TB cases among foreign-persons within 1 year after arrival in the United States. Our findings were consistent with a previous study that reported that 38.1% of the 2547 foreign-born TB cases within 1 year after arrival between 1992 and 1995 were among immigrants and refugees with class B1 or B2 TB (19). Although some of the remaining 638 cases may be among newly arrived immigrants and refugees with normal chest radiographs, most could be among new arrivals of nonimmigrant visitors and undocumented persons because they were not screened for TB before they departed for the United States (20). The CDC provided comprehensive training to panel physicians on the culture-based algorithm. This training likely helped panel physicians improve their diagnosis of TB among U.S-bound immigrants and refugees (13). Because of the requirement for the M. tuberculosis culture, drug-susceptibility testing, and directly observed therapy for TB treatment, the fee for the overseas medical examination increased. The U.S. Department of State sponsors refugees, but immigrants pay for their examination (5). The fee for immigrant examination is set by the U.S. Consular Sections in each country; in many cases, the fee includes the costs of TB treatment. The implementation of the culture-based algorithm also increased the CDC’s costs for training, education, and quality assurance. A separate study is under way at the CDC to evaluate the cost-effectiveness of the culture-based algorithm.
Certain limitations apply to interpreting the results of our analysis. Misclassifications of TB cases may occur during overseas screening and follow-up evaluation after arrival. Assumptions used for estimating the number of immigrants screened by the culture-based algorithm may be invalid. Follow-up data may not be reported randomly to the CDC. In 2007, the CDC started requiring state and local health departments to enter follow-up evaluation data via its newly developed EDN database. The new requirement may have affected the follow-up data reported from 2007 to 2008, resulting in a low percentage of completion of follow-up evaluation for persons who were screened by the smear-based algorithm. We compared the decline of reported TB cases among foreign-born persons within 1 year after arrival and the increase of smear-negative and culture-positive TB cases diagnosed overseas in U.S.-bound immigrants and refugees by the culture-based algorithm. However, this comparison was done without controlling for the decline of new arrivals of nonimmigrant visitors to the United States and the decrease of TB incidence in their countries of origin. From 2007 to 2012, WHO-estimated incidence of TB decreased globally by 10.9%, from 137 cases per 100 000 persons per year in 2007 to 122 cases per 100 000 persons per year in 2012 (21, 22). The mean of annual admissions of nonimmigrant visitors decreased by 8.5%, from 180.9 million between 2002 and 2006 to 165.5 million from 2007 to 2012 (23–29). However, the mean of the annual number of reported TB cases among foreign-born persons within 1 year after arrival decreased 24.7%, from 1504 cases from 2002 to 2006 to 1132 cases between 2007 and 2012 (14–16).
In 2012, 5334 (85.0%) of the 6274 reported TB cases were among foreign-born persons who had been in the United States more than 1 year after their arrival (16). Because 83.7% of the foreign-born TB cases in the United States were attributed to reactivation of TB (30), identifying and treating latent TB infection is important for eliminating TB in the United States (1, 31). In our analysis, prevalence of latent TB infection was 13.5% for U.S.-bound immigrants and refugees aged 2 to 14 years in countries with a WHO-estimated TB incidence of 20 cases or greater per 100 000 persons per year. In the United States, 11.9% of foreign-born persons aged 1 to 14 years had latent TB infection (32). Because shortened treatment regimens for latent TB infection have proved to be effective (33–35), cost-effective and operational research studies are needed to determine ways to address latent TB infection screening and treatment in foreign-born persons.
In conclusion, culture-based overseas TB screening is a high-yield intervention for preventing TB in U.S.-bound immigrants and refugees. To further reduce the TB incidence in foreign-born populations, consideration should be given to expanding TB screening to students, exchange visitors, and temporary workers from countries with a high incidence of TB, as well as finding novel strategies to address the large numbers of foreign-born persons with latent TB infection.
Supplementary Material
Appendix Figure 1. The smear-based overseas TB screening algorithm. TB = tuberculosis.
Appendix Figure 2. The culture-based overseas TB screening algorithm. IGRA = interferon-γ release assay; TB = tuberculosis; TST = tuberculin skin test; WHO = World Health Organization.
Appendix Table 1. Immigrants and Refugees Identified With Class B1 or B2 TB by the Smear-Based Algorithm and Class B1 TB or B2 Latent TB Infection by the Culture-Based Algorithm, 2007–2012*
Appendix Table 2. Immigrants and Refugees Who Were Diagnosed With TB and Completed Overseas TB Treatment by the Culture-Based Algorithm, 2007–2012
Appendix Table 3. Follow-up Evaluation of Newly Arrived Immigrants and Refugees With Class B1 or B2 TB Identified by the Smear-Based Algorithm and Class B1 TB or B2 Latent TB Infection Identified by the Culture-Based Algorithm, 2007–2012*
Acknowledgments
The authors thank Mr. Wei-Lun Juang for his computer programming support, Mr. Curtis Blanton for providing statistical consultation, and Ms. Zanju Wang for obtaining immigrant arrival data from the U.S. Department of Homeland Security. They also thank the staff of the CDC’s EDN team for managing the notification system for TB in immigrants and refugees, the staff of the CDC’s quarantine stations for collecting overseas medical examination forms at the ports of entry, panel physicians for performing overseas TB screening, the staff of the state and local health department for conducting follow-up evaluation, and Dr. Nancy Rytina of the U.S. Department of Homeland Security for providing summary data of immigrant arrivals.
Footnotes
Disclaimer: The findings and conclusions of this article are those of the authors and do not necessarily represent the official position of the CDC.
Disclosures: None. Forms can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M14-2082.
Reproducible Research Statement: Study protocol and data set: Not available.
Statistical code: Available from Mr. Liu (yliu@cdc.gov).
Author Contributions:
Conception and design: Y. Liu, D.L. Posey, M.S. Cetron, J.A. Painter.
Analysis and interpretation of the data: Y. Liu, D.L. Posey, M.S. Cetron, J.A. Painter.
Drafting of the article: Y. Liu, M.S. Cetron, J.A. Painter.
Critical revision of the article for important intellectual content: Y. Liu, D.L. Posey, M.S. Cetron, J.A. Painter.
Final approval of the article: Y. Liu, D.L. Posey, M.S. Cetron, J.A. Painter.
Provision of study materials or patients: M.S. Cetron.
Statistical expertise: Y. Liu, M.S. Cetron, J.A. Painter.
Obtaining of funding: M.S. Cetron, J.A. Painter.
Administrative, technical, or logistic support: M.S. Cetron, J.A. Painter.
Collection and assembly of data: Y. Liu, M.S. Cetron, J.A. Painter.
References
- 1.American Thoracic Society. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: controlling tuberculosis in the United States. Am J Respir Crit Care Med. 2005;172:1169–227. doi: 10.1164/rccm.2508001. [DOI] [PubMed] [Google Scholar]
- 2.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008;300:405–12. doi: 10.1001/jama.300.4.405. [DOI] [PubMed] [Google Scholar]
- 3.Alami NN, Yuen CM, Miramontes R, Pratt R, Price SF, Navin TR Centers for Disease Control and Prevention. Trends in tuberculosis—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:229–33. [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Technical Instructions for Panel Physicians. Atlanta, GA: Centers for Disease Control and Prevention; 1991. [Google Scholar]
- 5.Liu Y, Weinberg MS, Ortega LS, Painter JA, Maloney SA. Overseas screening for tuberculosis in U.S.-bound immigrants and refugees. N Engl J Med. 2009;360:2406–15. doi: 10.1056/NEJMoa0809497. [DOI] [PubMed] [Google Scholar]
- 6.Binkin NJ, Zuber PL, Wells CD, Tipple MA, Castro KG. Overseas screening for tuberculosis in immigrants and refugees to the United States: current status. Clin Infect Dis. 1996;23:1226–32. doi: 10.1093/clinids/23.6.1226. [DOI] [PubMed] [Google Scholar]
- 7.Maloney SA, Fielding KL, Laserson KF, Jones W, Nguyen TN, Dang QA, et al. Assessing the performance of overseas tuberculosis screening programs: a study among U.S.-bound immigrants in Vietnam. Arch Intern Med. 2006;166:234–40. doi: 10.1001/archinte.166.2.234. [DOI] [PubMed] [Google Scholar]
- 8.Oeltmann JE, Varma JK, Ortega L, Liu Y, O’Rourke T, Cano M, et al. Multidrug-resistant tuberculosis outbreak among U.S.-bound Hmong refugees, Thailand, 2005. Emerg Infect Dis. 2008;14:1715–21. doi: 10.3201/eid1411.071629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Notice to readers: revised technical instructions for tuberculosis screening and treatment for panel physicians. MMWR Morb Mortal Wkly Rep. 2008;57:292–3. [Google Scholar]
- 10.U.S. Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Emerging and Zoonotic Infectious Diseases. CDC Immigration Requirements: Technical Instructions for Tuberculosis Screening and Treatment. Atlanta, GA: Centers for Disease Control and Prevention; 2007. [on 23 May 2013]. Accessed at www.cdc.gov/immigrantrefugeehealth/pdf/tuberculosis-ti-2009.pdf. [Google Scholar]
- 11.Tuberculosis screening and treatment technical instructions (TB TIs) using cultures and directly observed therapy (DOT) implementation. Centers for Disease Control and Prevention; 2010. [on 4 January 2014]. Accessed at www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/tuberculosis-implementation.html. [Google Scholar]
- 12.Lowenthal P, Westenhouse J, Moore M, Posey DL, Watt JP, Flood J. Reduced importation of tuberculosis after the implementation of an enhanced pre-immigration screening protocol. Int J Tuberc Lung Dis. 2011;15:761–6. doi: 10.5588/ijtld.10.0370. [DOI] [PubMed] [Google Scholar]
- 13.Posey DL, Naughton MP, Willacy EA, Russell M, Olson CK, Godwin CM, et al. Centers for Disease Control and Prevention. Implementation of new TB screening requirements for U.S.-bound immigrants and refugees—2007–2014. MMWR Morb Mortal Wkly Rep. 2014;63:234–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Online tuberculosis information system. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [on 4 January 2014]. Accessed at http://wonder.cdc.gov/TB-v2010.html. [Google Scholar]
- 15.Centers for Disease Control and Prevention. Reported Tuberculosis in the United States 2011. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [on 4 January 2014]. pp. 1–154. Accessed at www.cdc.gov/tb/statistics/reports/2011/pdf/report2011.pdf. [Google Scholar]
- 16.Centers for Disease Control and Prevention. Reported Tuberculosis in the United States 2012. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [on 4 April 2014]. pp. 1–184. Accessed at www.cdc.gov/tb/statistics/reports/2012/pdf/report2012.pdf. [Google Scholar]
- 17.Liu Y. Panel physician. In: Loue S, Sajatovic M, editors. Encyclopedia of Immigrant Health. New York: Springer; 2012. pp. 1171–2. [Google Scholar]
- 18.Dara M, Gushulak BD, Posey DL, Zellweger JP, Migliori GB. The history and evolution of immigration medical screening for tuberculosis. Expert Rev Anti Infect Ther. 2013;11:137–46. doi: 10.1586/eri.12.168. [DOI] [PubMed] [Google Scholar]
- 19.Sciortino S, Mohle-Boetani J, Royce SE, Will D, Chin DP. B notifications and the detection of tuberculosis among foreign-born recent arrivals in California. Int J Tuberc Lung Dis. 1999;3:778–85. [PubMed] [Google Scholar]
- 20.Liu Y, Painter JA, Posey DL, Cain KP, Weinberg MS, Maloney SA, et al. Estimating the impact of newly arrived foreign-born persons on tuberculosis in the United States. PLoS One. 2012;7:e32158. doi: 10.1371/journal.pone.0032158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. WHO Report 2007: Global Tuberculosis Control: Surveillance, Planning, Financing. Geneva: World Health Organization; 2007. Report no. WHO/HTM/TB/2007.376. [Google Scholar]
- 22.World Health Organization. Geneva: World Health Organization; 2012. [on 12 November 2014]. Global Tuberculosis Report 2012. Report no. WHO/HTM/TB/2012.6. Accessed at http://apps.who.int/iris/bitstream/10665/75938/1/9789241564502_eng.pdf. [Google Scholar]
- 23.U.S. Department of Homeland Security. Annual Flow Report: Temporary Admissions of Nonimmigrants to the United States: 2006. Washington, DC: U.S. Department of Homeland Security; 2007. [on 12 November 2014]. Accessed at www.dhs.gov/xlibrary/assets/statistics/publications/NI_FR_2006_508_final.pdf. [Google Scholar]
- 24.Barr M, Jefferys K, Monger R. Annual Flow Report: Nonimmigrant Admissions to the United States: 2007. Washington, DC: U.S. Department of Homeland Security; 2008. [on 12 November 2014]. Accessed at www.dhs.gov/xlibrary/assets/statistics/publications/ois_ni_fr_2007.pdf. [Google Scholar]
- 25.Monger R, Barr M. Annual Flow Report: Nonimmigrant Admissions to the United States: 2008. Washington, DC: U.S. Department of Homeland Security; 2009. [on 12 November 2014]. Accessed at www.dhs.gov/xlibrary/assets/statistics/publications/ois_ni_fr_2008.pdf. [Google Scholar]
- 26.Monger R, Barr M. Annual Flow Report: Nonimmigrant Admissions to the United States: 2009. Washington, DC: U.S. Department of Homeland Security; 2010. [on 12 November 2014]. Accessed at www.dhs.gov/xlibrary/assets/statistics/publications/ni_fr_2009.pdf. [Google Scholar]
- 27.Monger R, Mathews M. Annual Flow Report: Nonimmigrant Admissions to the United States: 2010. Washington, DC: U.S. Department of Homeland Security; 2011. [on 12 November 2014]. Accessed at www.dhs.gov/xlibrary/assets/statistics/publications/ni_fr_2010.pdf. [Google Scholar]
- 28.Monger R. Annual Flow Report: Nonimmigrant Admissions to the United States: 2011. Washington, DC: U.S. Department of Homeland Security; 2012. [on 12 November 2014]. Accessed at www.dhs.gov/xlibrary/assets/statistics/publications/ni_fr_2011.pdf. [Google Scholar]
- 29.Monger R. Annual Flow Report: Nonimmigrant Admissions to the United States: 2012. Washington, DC: U.S. Department of Homeland Security; 2013. [on 12 November 2014]. Accessed at www.dhs.gov/sites/default/files/publications/ois_ni_fr_2012.pdf. [Google Scholar]
- 30.Ricks PM, Cain KP, Oeltmann JE, Kammerer JS, Moonan PK. Estimating the burden of tuberculosis among foreign-born persons acquired prior to entering the U.S., 2005–2009. PLoS One. 2011;6:e27405. doi: 10.1371/journal.pone.0027405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Thoracic Society; Centers for Disease Control and Prevention. Targeted tuberculin testing and treatment of latent tuberculosis infection. Am J Respir Crit Care Med. 2000;161:S221–47. doi: 10.1164/ajrccm.161.supplement_3.ats600. [DOI] [PubMed] [Google Scholar]
- 32.Bennett DE, Courval JM, Onorato I, Agerton T, Gibson JD, Lambert L, et al. Prevalence of tuberculosis infection in the United States population: the National Health and Nutrition Examination Survey, 1999–2000. Am J Respir Crit Care Med. 2008;177:348–55. doi: 10.1164/rccm.200701-057OC. [DOI] [PubMed] [Google Scholar]
- 33.Lobue P, Menzies D. Treatment of latent tuberculosis infection: an update. Respirology. 2010;15:603–22. doi: 10.1111/j.1440-1843.2010.01751.x. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Recommendations for use of an isoniazid-rifapentine regimen with direct observation to treat latent Mycobacterium tuberculosis infection. MMWR Morb Mortal Wkly Rep. 2011;60:1650–3. [PubMed] [Google Scholar]
- 35.Sterling TR, Villarino ME, Borisov AS, Shang N, Gordin F, Bliven-Sizemore E, et al. TB Trials Consortium PREVENT TB Study Team. Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 2011;365:2155–66. doi: 10.1056/NEJMoa1104875. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Figure 1. The smear-based overseas TB screening algorithm. TB = tuberculosis.
Appendix Figure 2. The culture-based overseas TB screening algorithm. IGRA = interferon-γ release assay; TB = tuberculosis; TST = tuberculin skin test; WHO = World Health Organization.
Appendix Table 1. Immigrants and Refugees Identified With Class B1 or B2 TB by the Smear-Based Algorithm and Class B1 TB or B2 Latent TB Infection by the Culture-Based Algorithm, 2007–2012*
Appendix Table 2. Immigrants and Refugees Who Were Diagnosed With TB and Completed Overseas TB Treatment by the Culture-Based Algorithm, 2007–2012
Appendix Table 3. Follow-up Evaluation of Newly Arrived Immigrants and Refugees With Class B1 or B2 TB Identified by the Smear-Based Algorithm and Class B1 TB or B2 Latent TB Infection Identified by the Culture-Based Algorithm, 2007–2012*