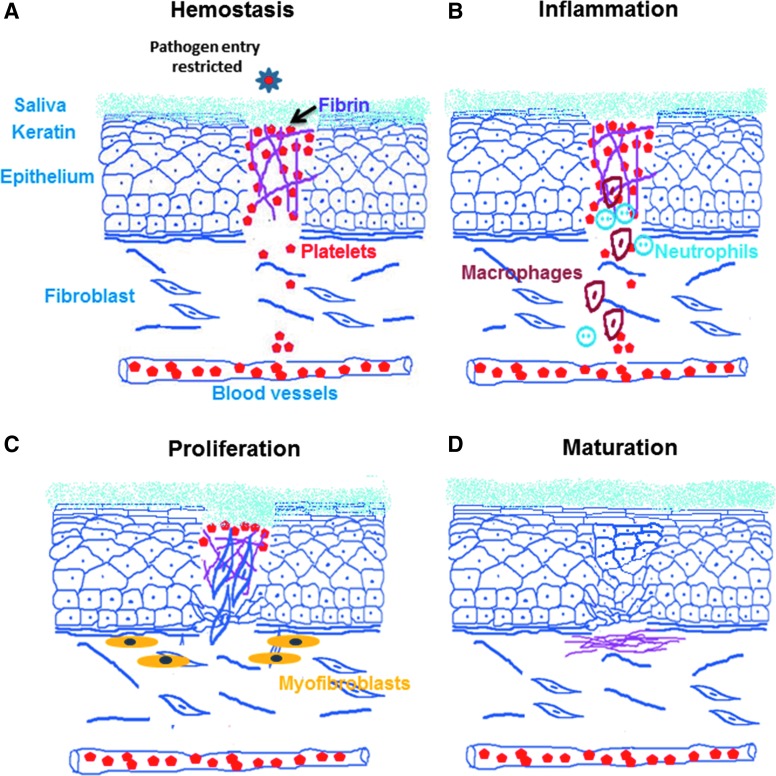
Figure 1.
Different stages of wound healing. (A) Hemostasis: wound closure starts with the first phase of clotting involving formation of immediate platelet plug, followed by initiation of the coagulation cascade. Oral wounds have a rich vascular supply and the salivary proteins which aid in forming a temporary hemostatic plug. (B) Inflammation: the second phase involves migration of acute (neutrophils) and eventually chronic inflammatory (monocytes–macrophages and lymphocytes) cells into the wound area. Moist oral mucosa possesses both innate (neutrophils and macrophages) and adaptive (immunoglobulins) immunities, which quickly resolve inflammation. This is well supported by chemical and enzymatic actions of salivary constituents. (C) Proliferation: the third phase consists of migration and proliferation of keratinocytes, endothelial cells, and fibroblasts that complete closure of wound. Proliferation and activation of fibroblasts to myofibroblasts hastens wound closure. (D) Maturation: the final fourth phase involves remodeling and reorganization that can be partial (scarring) or complete (regeneration).