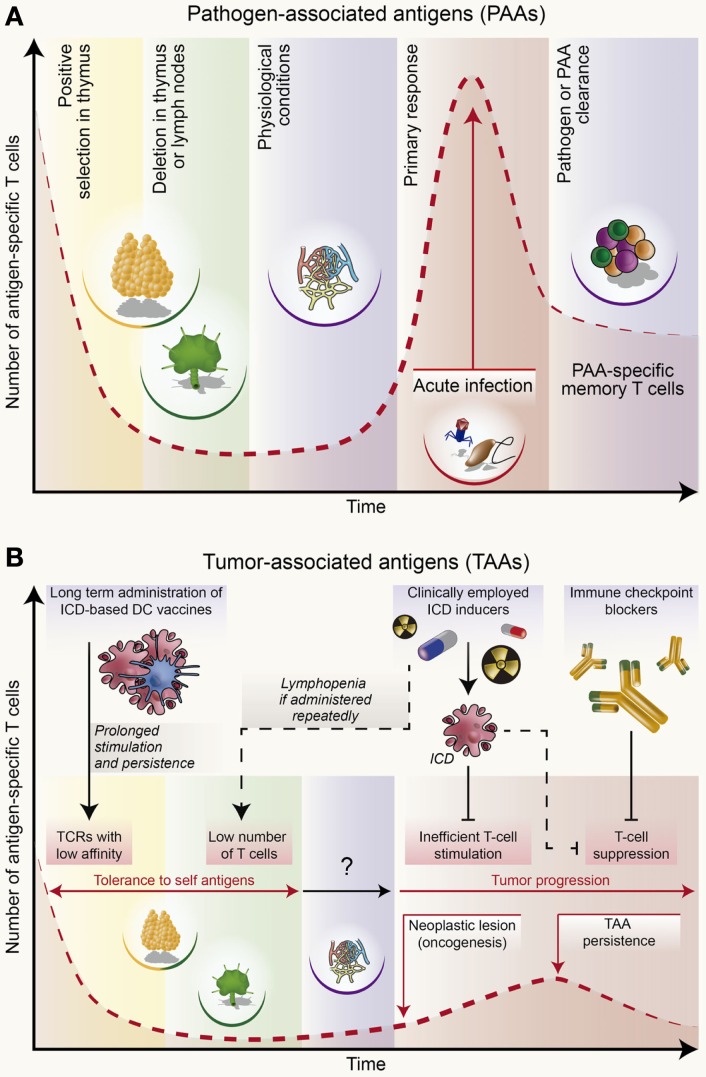
Figure 2.
Population dynamics of antigen-specific T cells during an immune response to infection or cancer. (A) T cells capable of putatively recognizing non-self, pathogen-associated antigens (PAAs) are not exposed to negative selection in the thymus or peripheral organs like lymph nodes. This allows for the constitutive presence of T lymphocytes bearing high-affinity T-cell receptor (TCR) in naïve conditions. Upon infection, these cells undergo robust expansion and acquire potent effector functions, hence driving an immune response that clears the pathogen and PAAs. Finally, PAA-specific T cells undergo contraction along with the establishment of immunological memory. To a limited extent, T cells reacting against PAAs expressed by virus-induced tumors may exhibit similar (although not identical) responses. (B) T cells that may recognize self or close-to-self antigens expressed by virus-unrelated malignancies undergo robust negative selection in the thymus and lymph nodes. Thus, all putative T lymphocytes bearing a high-affinity TCR against tumor-associated antigens (TAAs) are eliminated. However, some leakiness in this process allows for the persistence of TAA-specific T lymphocytes with low-affinity TCR, although at very low precursor frequencies. This is one of the reasons why in some individuals immunosurveillance at some stage fails to impede tumor progression. As malignant lesions progress, the amount of TAAs increases, causing a weak rise in TAA-specific T cells. However, tumor progression is generally coupled with the establishment of robust immunosuppressive networks that potently inhibit such TAA-targeting T cells. In this context, the administration of immunogenic cell death (ICD) according to a schedule that does not lead to lymphodepletion can favor the stimulation of TAA-targeting T cells and (re)instate immunosurveillance. Combining ICD inducers with checkpoint-blocking agents may further boost TAA-targeting immune responses. However, these treatments may not ensure the lifelong persistence of TAA-recognizing T cells, some of which are susceptible to elimination through tolerance mechanisms. Anticancer vaccines may counteract, at least to some extent, such loss. The figure was partly inspired from Baitsch et al. (234).