ABSTRACT
Objective:
The indications for permanent pacemaker implantations in Trinidad have expanded from initially symptomatic bradycardia to now include complex devices. A retrospective review of the available data was conducted to better understand the evolving trends in device implantation in Trinidad and Tobago.
Methods:
Data were collated from the two major implanting teams in Trinidad for the years 2005 and 2009. The two implanting centres were the Advanced Cardiovascular Institute (ACI) at Westshore Medical Centre and the Catheterization Laboratory of the Eric Williams Medical Sciences Complex (EWMSC). Data were based on retrospective collation using the implantation records.
Results:
The implantation rate for new devices increased from 39 per million to 103 per million population. The most common indications for new device implants in 2009 were high degree atrioventricular (AV) block (53%) and sick sinus syndrome (22%), with the notable appearance of congestive cardiomyopathy (13%) which was not present in the earlier cohort. Of particular note, 23 high-end devices were implanted in 2009. These were five cardiac-resynchronization therapy (CRT-P) devices, 14 automatic implantable cardio-defibrillator (AICD) devices and four combined cardiac-resynchronization therapy with defibrillator (CRT-D) devices versus none in 2005.
Conclusions:
In summary, over the period 2005 to 2009, a substantial increase in device implantation rates has occurred which now include high-end complex devices. Absolute rates, however, remain far below that of developed countries, indicating that the true need remains underserved. Furthermore, adjustment for gross domestic product suggests that the relatively buoyant economy of Trinidad and Tobago is capable of servicing a greater proportion of this need than is currently met.
Keywords: Pacemaker implantation, Trinidad and Tobago
RESUMEN
Objetivo:
Las indicaciones para las implantaciones permanentes de marcapasos en Trinidad se han extendido desde la bradicardia sintomática inicialmente, hasta la inclusión de dispositivos complejos en el presente. Se realizó una revisión retrospectiva de los datos disponibles para comprender mejor las tendencias cambiantes en la implantación de dispositivos en Trinidad y Tobago.
Métodos:
Se compilaron datos de los dos mayores equipos de especialistas en implantación de Trinidad, correspondientes a los años 2005 y 2009. Los dos centros de implantación fueron el Instituto Cardio-vascular Avanzado (ACI) en el Centro Médico de Westshore, y el Laboratorio de Cateterización del Complejo Eric Williams de Ciencias Médicas (EWMSC). Los datos se basaron en una recopilación retrospectiva a partir de los registros de implantación.
Resultados:
La tasa de implantación de nuevos dispositivos aumentó de 39 por millón a 103 por millón de habitantes. Las indicaciones más comunes para los implantes de nuevo dispositivos en 2009 fueron el bloqueo auriculoventricular (AV) de alto grado (53%), y el síndrome del seno enfermo (22%), con la notable aparición de la miocardiopatía congestiva (13%) que no estaba presente en la cohorte anterior. Cabe destacar que 23 dispositivos de alta gama fueron implantados en 2009. Se trató de cinco dispositivos para terapia de resincronización cardíaca (TRC-P), 14 dispositivos cardio-desfibriladores automáticos implantables (AICD), y cuatro dispositivos de terapia de resincronización cardíaca combinada con desfibrilador (TRC-D), en contraste con ninguno en 2005.
Conclusiones:
En resumen, durante el período 2005 a 2009, se produjo un incremento sustancial en las tasas de implantación de dispositivos, que ahora incluyen dispositivos complejos de alta gama. Las tasas absolutas, sin embargo, siguen siendo muy inferior a la de los países desarrollados, lo que indica que los servicios están por debajo de la necesidad. Además, los ajustes al producto interno bruto (PIB) sugieren que la relativamente boyante economía de Trinidad y Tobago es capaz de responder en mayor medida a esta necesidad en comparación con el servicio actual en tal sentido.
INTRODUCTION
Permanent pacemaker implantations have been performed in Trinidad for several years. The indications have expanded from initially symptomatic bradycardia to now include complex devices which aid in heart failure management, and devices for both the primary and secondary prevention of sudden cardiac death through the prompt and automated termination of episodes of ventricular tachycardia and ventricular fibrillation. Notwithstanding such expanded uses, the local demographics and patterns of implantation have not been recently assessed domestically. We therefore undertook a retrospective review of the available data in an attempt to better understand the evolving trends in device implantation in Trinidad and Tobago including changes in the demographics, indications for pacing and modes of pacing in the Trinidad and Tobago population over the study period.
SUBJECTS AND METHODS
As part of an international registry and data collection process for the World Survey of Cardiac Pacing and Cardioverter-Defibrillators (1, 2), two years of data were collated from the two major implanting teams in Trinidad for the years 2005 and 2009, respectively, the years for the most recent census. The two implanting centres were the Advanced Cardiovascular Institute (ACI), which is now based at Westshore Medical Centre (formerly at St Clair Medical Centre) and the Catheterization Laboratory of the Eric Williams Medical Sciences Complex (EWMSC). Data were based on retrospective collation using the implantation records. These implantation records are used for both clinical and industry purposes and are mandatory per implant. Each implanting centre is responsible for maintaining its own records. Both centres also use procedure logbooks so that the entered information could be verified with the implantation records. Approval and consent was granted by the relevant departments of both institutions for access to medical records of patients for collection of retrospective data for this study.
Trinidad and Tobago has been a participant of the Heartbeat International Programme since 1985. This is a non-governmental charitable organization responsible for the donation of heart rhythm devices to the indigent populations of the world. Thus, device availability may have been privately purchased by the individual or his insurer, purchased by the state through a public institution or special application subvention, or else may have been donated by Heartbeat International Programme after validation of indigence.
Implantation rates for various countries were taken from The World Survey of Cardiac Pacing and Cardioverter-defibrillators: calendar year 2005 (2). Economic data were referenced from the online database supplied by the World Bank with comparisons made by creating a novel ratio of implantation rate per million/per capita gross domestic product (GDP) for each territory studied. Attempts were made to select representative countries with both higher and lower GDP ratings than Trinidad and Tobago so as to cater for attributable differences in priority in healthcare spending. The results were presented in descending order of GDP from the United States of America [USA] (highest per capita GDP) to Peru (lowest per capita GDP).
RESULTS
The number of new devices implanted increased during the interval period from 51 devices in 2005 to 127 devices in 2009, representing a 150% increase. The mean age for implantation remained unchanged, 69 years in 2005 versus 68 years in 2009. However, there was a change in age distribution with 97% being over 60 years in 2005, compared with only 73% in 2009. By 2009, therefore, 27% of the persons receiving pacemakers and other rhythm devices were under 60 years old (Fig. 1). The gender distribution of recipients also changed substantially with a male:female ratio of 2:3 in 2005 compared to 1:1 in 2009.
Fig. 1. Age distribution of patients in 2005 and 2009.
Implanting physicians included interventional cardiologists, cardiac electrophysiologists and thoracic surgeons, with the majority of implantations being performed by nonsurgeons. Training of local implanters was also commenced in the interval between the two samples.
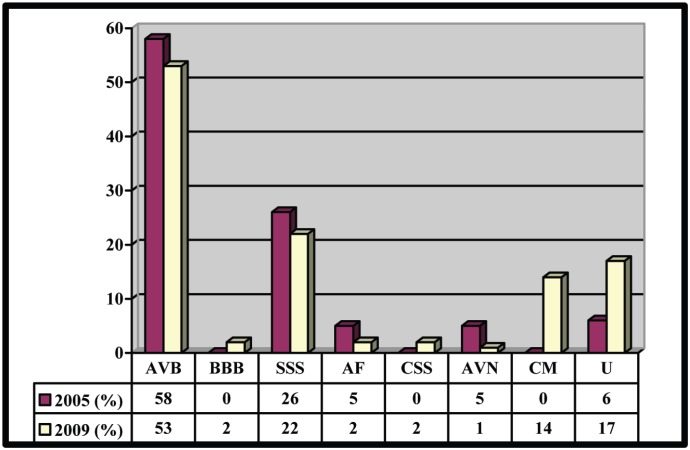
The most common indications for new device implants in 2009 were high-degree atrioventricular (AV) block (53%) followed by sick sinus syndrome (22%). This trend was quite similar to that in 2005 with the exception that there was a larger number of patients having pacemakers implanted for cardiomyopathy (14% in 2009 vs 0% in 2005) [Fig. 2].
Fig. 2. Indications for pacing in 2005 and 2009. AVB–high grade atrioventricular block, BBB–bundle branch block, SSS– sick sinus syndrome, AF–atrrial fibrillation, CSS–carotid sinus syncope, AVN–atrioventricular nodal ablation, CM–cardiomyopathy, U–unspecified.
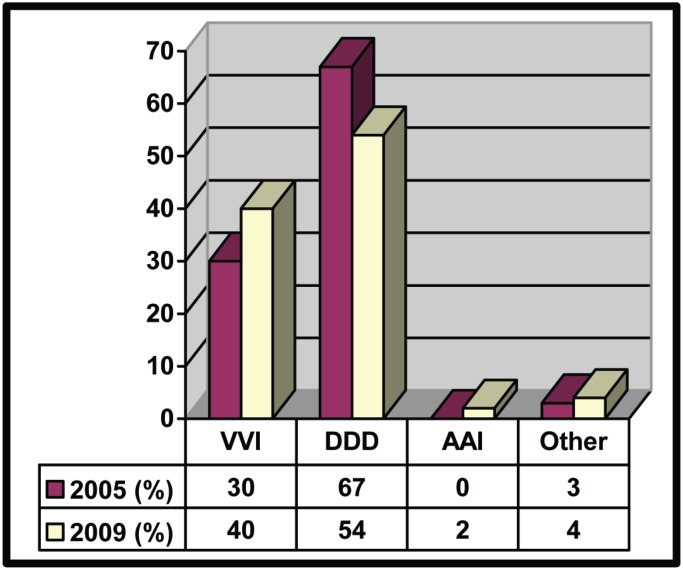
There were more pulse generators replaced in 2009 as compared to 2005 (20 in 2009 versus 7 in 2005). The pacing mode at initial implant during the interval period was as follows: dual chamber = 54% in 2009 versus 67% in 2005, single chamber = 40% in 2009 vs 30% in 2005 (Fig. 3). Pacing lead insertion for bradycardia indications was done exclusively by the transvenous route (100%). Two cases using combined transvenous and epicardial leads were performed in 2009, both for insertion of a left ventricular lead as part of cardiac resynchronization therapy. The electrode configuration was predominantly bipolar for both the atrium and ventricle.
Fig. 3. Modes of pacing in 2005 and 2009. VVI–ventricular based single chamber pacemaker, DDD–ventricular demand with atrial tracking dual chamber pacemaker, AAI–atrial based single chamber pacemaker.
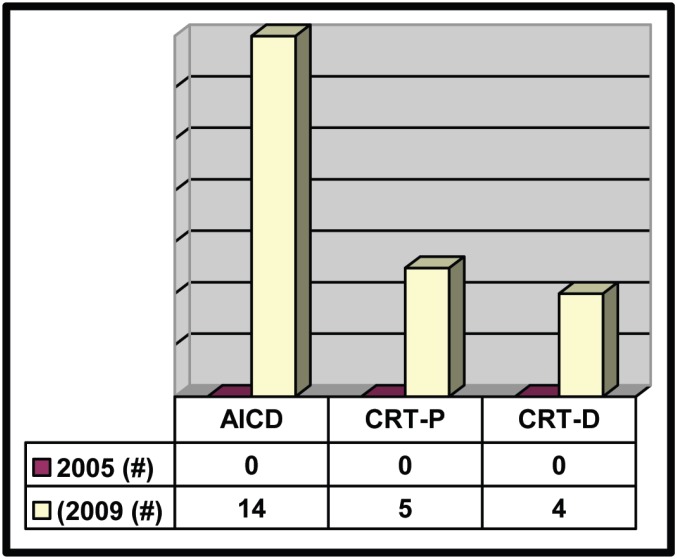
Of particular note, more complex devices were implanted in 2009, namely: five cardiac-resynchronization therapy (CRT-P) devices, 14 automatic implantable cardio-defibrillator (AICD) devices and four combined cardiac-resynchronization therapy with defibrillator (CRT-D) devices versus none in 2005 (Fig. 4).
Fig. 4. Use of complex pacing devices in 2005 and 2009. AICD–automatic implantable cardio-defibrillator, CRT-P–cardiac resynchonization therapy (pacing only), CRT-D–cardiac resynchronization therapy with defibrillator.
DISCUSSION
Within the last two decades, there has been a dramatic change in the understanding of bradycardia pacing from the simple concept of mortality/morbidity reduction in treating complete heart block with a single chamber pacemaker to understanding the need for both atrio-ventricular and ventricular-ventricular synchrony in an attempt to imitate the normal cardiac cycle as much as possible. The aim is to reduce heart failure, atrial fibrillation and a potential side effect of the single chamber device, the “pacemaker syndrome” (3, 4). We have also seen the increased use of complex devices to aid in the treatment of advanced heart failure (via CRT-P and CRT-D devices) as well as for the primary and secondary prevention of sudden cardiac death [via AICD devices] (5). On the other hand, these devices come at a substantial cost (6).
Insertion of implantable devices has been performed for several years in Trinidad. This has been historically successfully performed by varied categories of implanting doctors. Initially, implantations were done by thoracic or cardiothoracic surgeons, especially since sometimes lead implantation required an open thoracotomy for the implantation of epicardial leads. Later, as device and lead size decreased, and as the requirement for epicardial lead positioning became less frequent, cardiologists gradually implanted an increasingly large percentage of devices utilized in treating bradycardias worldwide. More recently, a new category of cardiologists devoted to heart rhythm disturbances has evolved. These electrophysiologists are in short supply worldwide but their importance in developing solutions for patients with tachyarrhythmias is well recognized.
A major improvement has been the increase in physician expertise and education. More internists and general cardiologists are comfortable referring patients for not only the traditional bradycardia devices but for cases where complex devices are indicated. There has also been greater dialogue between the referring physicians and the implanters, allowing appropriate device selection for the clinical needs of the patient. With the local presence of a dedicated full-time electrophysiologist since 2009, and the presence in the pacemaker clinics of the EWMSC of visiting consultants from the Johns Hopkins University under the Trinidad and Tobago Health Science Initiative project, greater cross-education has occurred and will surely continue to drive this process. There has also been a thrust to train the younger physicians in both device implantation and management. With more persons interested in pacing and this continued cross-education, greater skill in programming techniques has developed relevant to the patient's clinical needs eg use of rate response, AAI and DDI pacing modes. This skill has also translated into more frequent use of active lead fixation as well as the multi-disciplinary approach to device management. This includes echocardiography-guided optimization of CRT devices and thoracoscopic implantations of epicardial left ventricular pacing leads in those heart failure patients in whom technical difficulty was encountered during coronary sinus lead placement via the customary transvenous access.
One limitation of the database was the absence of response, by the time of publication, to data requests made to a new group at one implanting site in the 2009 cohort. However, the estimated data error as a consequence of this omission was equivalent to a 4% underestimation in the total number of devices. The inclusion of this data would not have substantially changed the conclusions of this analysis. There would in all probability have been a small increase in the number of devices to just over the 100% increase recorded and virtually no change in the gender distribution or absolute number of complex devices. The data presented therefore minimally underestimates the steady increase in device implantation in Trinidad and Tobago over the interval period. Industry support has also improved now, with on-site expertise for management of Medtronic™, St Jude Medical™ and Boston-Scientific™. Programming computers for devices from all major manufacturers are now available. The range of devices, both private and donated, has also expanded, making it possible to choose the best device for the patient's clinical needs in many instances.
Having said such, the implantation rate remains far below rates in developed countries. For example, the number of new implants per million population increased from 2005 to 2009 (n = 39 per million in 2005 vs 103 per million in 2009) but this was still far lower than developed nations eg United Kingdom (n = 447 per million in 2005 and 511 per million in 2008) or Puerto Rico (n = 448 per million in 2005). Notwithstanding better access of patients to health insurance and programmes like Heartbeat International, funding is still a major obstacle to procurement, especially for complex devices which can run in excess of TT$100 000 depending on the type of device, with significant variation amongst manufacturers.
Another challenge is the absence of a clearly articulated policy by the Government of Trinidad and Tobago via the Ministry of Health regarding direct funding of devices for the indigent population. At this time, patients and their relatives continue to rely on charitable organizations like Heartbeat International, Rotary International, local churches/ charities and self-raising of funds when health insurance is not readily available. In particular, the Heartbeat International charity has contributed substantially to the increment in device provision.
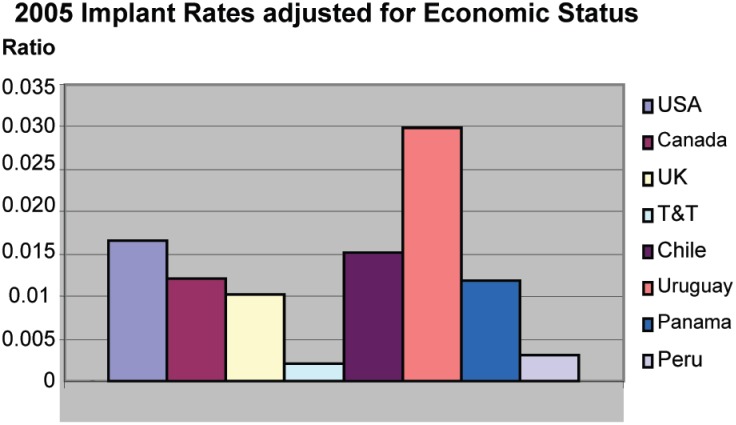
We therefore set about determining what should be an expected device implantation rate for a country with an economic and developmental status of Trinidad and Tobago. After excluding countries such as Brazil which would be expected to have a disproportionate device requirement because of the then prevalence of endemic Chagas disease, an infectious cause of heart block, we established a “Propensity Index”, obtained by dividing the device implantation rate per million by the per capita GDP for each country under study. Care was taken to sample countries both above and below the economic ranking of Trinidad and Tobago. The 2005 cohort was used since this represented the latest published complete data set for both new device implantation per million and per-capita GDP. Of the eight countries sampled, Trinidad and Tobago scored the lowest (Fig. 5), confirming an unexplained gap between the economic fortunes of Trinidad and Tobago and its provision of devices when compared with prevailing national efforts globally. For the other seven countries sampled, the Propensity Score for device provision ranged between 1.4 and 13.9 times that of Trinidad and Tobago. Put differently, therefore, when adjusted for economic status and hence presumably the ability to provide, other countries sampled were on average seven times more likely to provide pacemakers and other devices for its citizens than Trinidad and Tobago. A resource-based and rational strategic national philosophy must therefore be developed to address this discrepancy. Perhaps only bradycardia and secondary prevention AICDs should be paid for by the state. We may well need to look at other health systems similar to ours to assess what priorities have been successfully used to determine resource allocation (7). In addition, local physician consensus should be included to help define policy whenever health economics significantly affect clinical decision making.
Fig. 5. Ratio of pacemaker implantation rate: per capita gross domestic product (GDP) by country. UK–United Kingdom, T&T–Trinidad and Tobago.
In summary, Trinidad and Tobago has been improving with respect to the technical complexity and numbers of rhythm devices implanted in the population, but implantation rates remain far below rates in developed countries even when adjusted for economic status, suggesting that the need remains under-served.
ACKNOWLEDGMENTS
We wish to express our thanks to the staff of the Catheterization Laboratories of the Eric Williams Medical Sciences Complex and the Advanced Cardiovascular Institute for their assistance in the collection of data for this research project. Thank you also to the research assistants of the Doctors Inn Research Group for their invaluable help in compiling the data.
REFERENCES
- 1.Mond HG, Irwin M, Morillo C, Ector H. The world survey of cardiac pacing and cardioverter defibrillators: calendar year 2001. Pacing Clin Electrophysiol. 2004;27:955–964. doi: 10.1111/j.1540-8159.2004.00565.x. [DOI] [PubMed] [Google Scholar]
- 2.Mond HG, Irwin M, Ector H, Proclemer A. The world survey of cardiac pacing and cardioverter-defibrillators: calendar year 2005: an International Cardiac Pacing and Electrophysiology Society (ICPES) project. Pacing Clin Electrophysiol. 2008;31:1202–1212. doi: 10.1111/j.1540-8159.2008.01164.x. [DOI] [PubMed] [Google Scholar]
- 3.Al-Khatib SM, Anstrom KJ, Eisenstein EL, Peterson ED, Jollis JG, Mark DB, et al. Clinical and economic implications of the Multicenter Automatic Defibrillator Implantation Trial-II. Ann Intern Med. 2005;19:593–600. doi: 10.7326/0003-4819-142-8-200504190-00007. [DOI] [PubMed] [Google Scholar]
- 4.Piccini JP, Al-Khatib SM, Myers ER, Anstrom KJ, Buxton AE, Peterson ED, et al. Optimal timing of implantable cardioverter-defibrillator implantation after myocardial infarction: a decision analysis. J Cardiovasc Electrophysiol. 2010;21:791–798. doi: 10.1111/j.1540-8167.2009.01696.x. [DOI] [PubMed] [Google Scholar]
- 5.Zareba W, Zareba KM. Which patients with chronic heart failure should be referred for CRT-D implantation? Practical implications of current clinical research. Pol Arch Med Wewn. 2010;120:95–102. [PubMed] [Google Scholar]
- 6.Ribeiro RA, Stella SF, Camey SA, Zimerman LI, Pimentel M, Rohde LE, et al. Cost-effectiveness of implantable cardioverter-defibrillators in Brazil: primary prevention analysis in the public sector. Value Health. 2010;13:160–168. doi: 10.1111/j.1524-4733.2009.00608.x. [DOI] [PubMed] [Google Scholar]
- 7.Bradfield J, Warner A, Bersohn MM. Low referral rate for prophylactic implantation of cardioverter-defibrillators in a tertiary care medical center. Pacing Clin Electrophysiol. 2009;32(Suppl 1):S194–S197. doi: 10.1111/j.1540-8159.2008.02281.x. [DOI] [PubMed] [Google Scholar]