Abstract
Background
A minority of overweight or obese children are identified as such by a healthcare provider (HCP). The aim of this study was to examine characteristics of caregiver-reported HCP identification of overweight or obesity and whether it is associated with children’s waist circumference (WC).
Methods
This was an observational study using a nationally representative sample of 14,694 children (2–15 years of age) from the 2001–2010 National Health and Nutrition Examination Survey. Proxy respondents (i.e., caregivers) for 4906 overweight or obese (BMI ≥ 85th percentile) children reported whether an HCP had ever told them that their child was overweight. Multi-variable logistic regression analyses were used to examine associations between reported HCP identification of overweight and child sociodemographic and anthropometric characteristics.
Results
Over 75% of caregivers of overweight or obese children did not recall being notified of their child’s weight status by an HCP, though this proportion has decreased over the past decade. A significant WC by weight status interaction indicated abdominal adiposity was positively associated with reported HCP identification for obese children, but not for overweight children.
Conclusions
Lower levels of reported HCP identification were observed for overweight children, compared to obese children; among obese children, those with lower levels of abdominal adiposity were less likely to be identified as overweight by an HCP, according to caregivers. Reasons for this finding remain unclear. Providers may be relying on a child’s appearance, rather than universally screening all patients for overweight. Additionally, a variety of parent and provider characteristics may influence weight-related communications and caregiver recall of such information.
Introduction
Recent estimates indicate that nearly one third (31.8%) of US youth are overweight or obese (BMI ≥ 85th percentile for age and gender),1,2 placing them at risk for high cholesterol, hypertension, depression, decreased quality of life, type 2 diabetes, and asthma.3,4 Many obese children go on to become obese adults.5 Appropriate and timely recognition of pediatric overweight and obesity is a critical first step for weight-related interventions to prevent or treat overweight and obesity in children. Such efforts may be greatly facilitated if parents and children have an accurate perception of a child’s weight status and if overweight children are recognized as such by a healthcare provider (HCP).6,7 Unfortunately, parental recognition of childhood overweight and obesity is low. Given that more than half of parents do not recognize when their child is overweight,8–11 physicians have a critical role to play in identifying overweight and obese children and adolescents.12 As such, routine screening for obesity in pediatric and primary care offices and communication of findings to parents has been recommended by the American Medical Association’s expert panel,13,14 the American Academy of Pediatrics,15 the American Academy of Family Physicians,16 and the US Preventive Services Task Force.17
Despite existing recommendations, pediatric overweight and obesity are often under-recognized in clinical settings.13,18–23 A few studies have examined a limited set of sociodemographic correlates of provider identification of overweight, such as age, race or ethnicity, and insurance status. A recent study using data from the National Health and Nutrition Examination Survey (NHANES) assessed national trends in HCP identification of youth overweight based on parental recall, and suggested that though parental report of HCP notification increased between 1999 through 2008, fewer than one quarter of parents of overweight or obese youth report being told that their child is overweight. Recall of HCP notification was more likely among nonwhite children, insured children, and children with a higher number of provider visits in the previous year.22
Both BMI and waist circumference (WC) are independently associated with numerous health risks in children.24–27 Though some research suggests that WC may be associated with parent perceptions of their children’s weight,28,29 we found no published studies examining abdominal adiposity in relation to HCP identification of pediatric overweight. Abdominal adiposity may increase identification of childhood overweight by an HCP for several reasons. First, children with greater WCs may appear more obviously overweight than children with lower levels of abdominal adiposity, but high BMI percentiles. Relying on this visual cue may decrease the likelihood of HCP identification of overweight for children with high BMIs but lower WCs. Previous studies have reported that children with lower BMI percentiles are less likely to be identified as overweight by an HCP, and that this may be a result of those children appearing less obviously obese.30 Second, children with a greater degree of abdominal adiposity may be more likely to suffer from weight-related health comorbidities, which may also increase the likelihood of HCP identification of overweight. The aim of this research was to extend previous research by examining characteristics of caregiver-reported HCP identification of overweight or obesity and whether it is associated with children’s abdominal adiposity, independent of BMI and potential confounders, such as health status or healthcare utilization.
Methods
Data Source and Study Population
Data from five two-year cycles of the NHANES, conducted between 2001 and 2010, were used in this analysis. NHANES is a cross-sectional survey of the civilian, non-institutionalized US population.31 NHANES uses a complex, multi-stage probability sampling design, with some subgroups oversampled. The unweighted response rates for the total NHANES examined sample ranged from 75 to 80% for the five survey cycles. This study used data from 15,620 children (2–15 years of age) who completed the mobile examination component (MEC) of NHANES. Because the study utilized publicly available secondary data, no institutional review board approval or consent/assent information were required.
Proxy respondents (typically a parent or guardian, hereinafter “caregivers”) reported whether an HCP had ever told them that their child was overweight. Children 16 years and older responded for themselves whether they had ever been told by an HCP that they were overweight; thus, we decided to exclude this group because they may respond differently than a caregiver. Of the examined sample, 14,694 (94%) had anthropometric data (e.g., weight, height, or WC). Standardized weight and height measures collected in the MEC were used to calculate age- and sex-specific BMI percentiles, according to the 2000 CDC growth charts.32,33 Children were classified as overweight (excluding obese) if they had a sex- and age-specific BMI percentile 85–94.9 and obese if they had a BMI percentile ≥ 95. Only overweight or obese children were included in multi-variable logistic regression analyses (n = 4906). Age-and sex-specific WC percentiles were calculated based on NHANES anthropometric reference data.34 Categories of WC percentiles were defined similarly to the BMI cutoffs: < 85th percentile; 85–94.9th percentile, and ≥ 95th percentile.
We controlled for child sociodemographic characteristics that have been previously associated with HCP identification,22 including: age (2–5, 6–11, and 12–15 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other), and poverty-income ratio (PIR; 0–100% of federal poverty threshold [FPT], 101–200% FPT, 201–400% FPT, and > 400% FPT). We included an indicator variable for each survey cycle to control for time trends in HCP identification.22 Finally, general health status (excellent, very good, good, fair, or poor), insurance status (currently insured or not), and number of physician visits in the prior year (0, 1–3, and 4 + ) were included in models to control for potential confounders of the relationships between WC and likelihood of HCP identification of overweight (i.e., poor health, healthcare access, and utilization). Sample sizes of racial and ethnic subgroups other than non-Hispanic white, non-Hispanic black, and Mexican American are small; thus, results are not presented separately for participants identifying as other races or ethnicities, though they were included in the analytic sample.
Statistical Analysis
Univariate logistic regression models were used to examine crude or unadjusted associations between covariates of interest and reported HCP identification of overweight. Subsequently, multivariable logistic regression models were used to examine caregiver report of identification by an HCP in relation to child anthropometry, controlling for potential confounders. An interaction term between WC category (i.e., < 85th percentile, 85–94.9th percentile, and ≥ 95th percentile) and weight status (i.e., overweight or obese) was included in the models to examine whether associations between WC and HCP identification differed by child weight status. Sensitivity analyses examined WC percentile and BMI percentile as continuous variables; however, for ease of interpretation, results are shown for WC and BMI percentile categories. Marginal or predicted probabilities of HCP identification were calculated across survey cycles and child characteristics, including the WC by BMI percentile interaction, to aid in the interpretation of the associations and interaction. MEC sample weights and survey procedures in STATA/SE statistical software (Version 12.0; StataCorp LP, College Station, TX) were used to account for the complex sampling design of NHANES.35 Significant differences were assessed at the p < 0.05 level.
Results
Characteristics of the 14,694 children (including non-overweight) can be seen in Table 1. Approximately 59% of the sample were non-Hispanic White, 15% non-Hispanic Black, 14% Mexican American, and 12% were identified as “other.” Overall, approximately 31% of all US children [mean age, 9.3 years; standard error (SE), 0.08] were overweight or obese. Approximately 15.0% of children were overweight and 16.3% were obese. According to criteria established by the International Task Force on Obesity,36 17.7% of the sample were overweight and 11.2% were obese. Mean WC percentile for normal-weight children was 38.4 (SE, 0.3); overweight children had a mean WC percentile of 65.2 (SE, 0.4), whereas obese children had a mean WC percentile of 86.4 (SE, 0.3).
Table 1.
Sociodemographic Characteristics of US Childrena
| Normal weight (68.7%) | Overweight (15.0%) | Obese (16.3%) | |
|---|---|---|---|
| Age | 8.4 (0.1) | 9.2 (0.1) | 9.4 (1.0) |
| Female | 49.35 (0.6) | 51.1 (1.1) | 46.2 (1.0) |
| Race or ethnicity | |||
| Non-Hispanic white | 61.0 (1.5) | 55.6 (2.2) | 52.0 (2.7) |
| Non-Hispanic black | 13.9 (1.0) | 14.4 (1.1) | 18.3 (1.3) |
| Mexican American | 12.6 (1.0) | 15.8 (1.3) | 18.3 (1.7) |
| Income-to-poverty ratio | |||
| < 100% FPT | 22.1 (0.9) | 23.5 (1.3) | 28.1 (1.5) |
| 101–200% FPT | 23.2 (0.8) | 23.3 (1.4) | 26.4 (1.2) |
| 201–400% FPT | 28.8 (0.8) | 31.3 (1.7) | 28.6 (1.4) |
| > 400% FPT | 25.9 (1.2) | 21.7 (1.6) | 16.9 (1.3) |
| No. of healthcare visits | |||
| 0 | 10.8 (0.6) | 11.5 (0.8) | 10.8 (0.8) |
| 1–3 | 62.6 (0.6) | 61.2 (1.3) | 63.1 (1.3) |
| 4 + | 26.6 (0.7) | 27.3 (1.1) | 26.0 (1.2) |
| Insured | 90.3 (0.6) | 88.5 (1.0) | 87.0 (1.1) |
| General health condition | |||
| Excellent | 55.9 (0.8) | 50.4 (1.4) | 40.8 (1.4) |
| Very good | 24.6 (0.6) | 28.8 (1.2) | 25.2 (1.3) |
| Good | 15.9 (0.5) | 17.5 (1.0) | 28.0 (1.2) |
| Fair or poor | 3.6 (0.2) | 3.2 (0.4) | 6.1 (0.4) |
| Waist circumference | |||
| < 85th percentile | 96.4 (0.3) | 89.0 (1.0) | 38.6 (1.2) |
| 85–94.9th percentile | 0.4 (0.1) | 6.6 (0.8) | 29.6 (1.3) |
| ≥ 95th percentile | 3.2 (0.3) | 4.3 (0.7) | 31.8 (1.2) |
Values indicate weighted means/proportions (standard error).
n = 14,694, 2–15 years of age, National Health and Nutrition Examination Survey 2001–2010.
FPT, federal poverty threshold.
Overall, only 10.2% of overweight and 36.2% of obese children were reported by a caregiver as having been identified as overweight by an HCP. Table 2 illustrates the adjusted probabilities of reported HCP identification across child characteristics, by weight status, and overall.
Table 2.
Marginal Probabilities (95% CI) of Reported HCP Identification of Overweight by Child Characteristics Predicted from Multivariable Logistic Regression Models
| Overweight | Obese | Overweight or obese | |
|---|---|---|---|
| 2001–2002 | 7.2 (5.2–9.3) | 31.2 (25.9–36.5) | 20.0 (16.5–23.5) |
| 2003–2004 | 9.9 (7.6–12.1) | 38.1 (34.2–41.9) | 25.0 (22.2–27.7) |
| 2005–2006 | 6.8 (5.1–8.5) | 30.0 (25.5–34.5) | 19.1 (16.1–22.2) |
| 2007–2008 | 11.8 (9.3–14.4) | 41.8 (37.4–46.1) | 27.8 (24.6–31.0) |
| 2009–2010 | 9.6 (7.7–11.4) | 37.8 (34.3–41.4) | 24.8 (22.1–27.4) |
| Age (years) | |||
| 2–5 | 4.5 (3.2–5.8) | 23.0 (19.3–26.8) | 14.4 (11.9–16.8) |
| 6–11 | 8.4 (6.9–9.9) | 33.4 (30.6–36.2) | 21.5 (19.7–23.3) |
| 12–15 | 13.1 (10.7–15.5) | 47.0 (43.2–50.8) | 31.7 (29.0–34.5) |
| Race or ethnicity | |||
| Non-Hispanic white | 7.8 (6.5–9.2) | 31.7 (28.3–35.1) | 20.5 (18.4–22.6) |
| Non-Hispanic black | 10.4 (8.1–12.6) | 40.2 (37.3–43.0) | 26.7 (24.5–28.9) |
| Mexican American | 11.2 (8.8–13.7) | 40.1 (36.4–43.8) | 26.7 (23.9–29.5) |
| No. of healthcare visits | |||
| 0 | 5.8 (4.0–7.0) | 27.2 (21.6–32.8) | 17.3 (13.6–21.0) |
| 1–3 | 9.2 (7.7–10.7) | 36.5 (33.6–39.4) | 23.9 (22.0–25.7) |
| 4 + | 10.3 (7.9–12.6) | 38.1 (34.2–42.0) | 25.1 (22.1–28.1) |
| Uninsured | 7.5 (5.5–9.5) | 31.6 (26.5–36.7) | 20.2 (16.9–23.4) |
| Insured | 9.3 (7.8–10.8) | 36.5 (34.1–38.9) | 24.3 (22.6–26.1) |
| General health status | |||
| Excellent | 7.5 (5.8–9.3) | 30.2 (26.6–33.7) | 19.5 (17.0–22.0) |
| Very good | 9.6 (7.6–11.7) | 36.2 (31.9–40.4) | 23.9 (20.9–26.8) |
| Good | 11.7 (9.4–13.9) | 42.0 (37.7–46.3) | 28.3 (25.3–31.3) |
| Fair or poor | 13.2 (8.9–17.6) | 44.5 (36.4–52.7) | 30.3 (23.9–36.6) |
| Waist circumference | |||
| < 85th percentile | 10.2 (8.4–12.0) | 20.5 (17.0–24.0) | a |
| 85–94.9th percentile | 12.4 (5.1–19.7) | 34.0 (30.2–37.8) | a |
| ≥ 95th percentile | 15.1 (2.9–27.3) | 53.9 (48.7–59.1) | a |
Because of the presence of a significant interaction between weight status and waist circumference (WC), the main effect of WC is not shown for the total sample.
HCP, healthcare provider; CI, confidence interval.
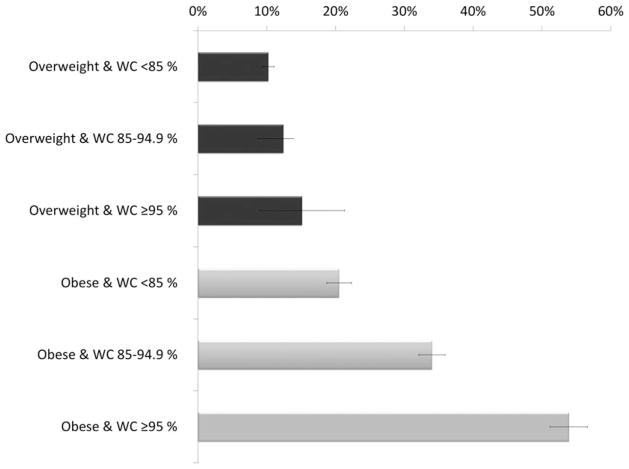
In unadjusted models, 14.2% [95% confidence interval (CI): 12.5–15.9] of children with a WC percentile < 85th were reported as identified as overweight by an HCP, compared to 32.3% of children in the middle WC category (95% CI: 28.3–36.3) and 47.6% of children in the highest WC percentile ( ≥ 95th) category (95% CI: 42.8–52.4). In fully adjusted models controlling for child sociodemographic, health characteristics, and child weight status, the adjusted probabilities of caregiver report of HCP identification by WC category were largely similar (16.6%, 95% CI: 14.6–18.6 for WC < 85th; 25.0%, 95% CI: 21.7–28.3 for WC 85–94.9th percentile; 40.6%, 95% CI: 35.9–45.4 for WC ≥ 95th percentile). Adding the WC by weight status interaction, the effect of increasing WC percentile was apparent only for obese children. Figure 1 depicts the WC by weight status interaction by displaying the adjusted probabilities of reported HCP identification of overweight across weight status and WC categories. Obese children had higher adjusted probabilities of reported HCP identification across all WC categories, as compared to overweight children. Sensitivity analyses using continuous BMI and WC percentiles indicated that the positive association between abdominal adiposity levels and reported HCP identification among obese children did not appear to be the result of increasing BMI percentiles within the obese category. Interaction between continuous WC percentile and BMI percentile was also significant; across all of the BMI percentiles within the obese category, higher WC percentiles were positively associated with reported HCP identification.
Figure 1.
Marginal probabilities of reported HCP identification illustrating weight status by waist circumference (WC) interaction. Note: Estimated marginal probabilities are adjusted for age, survey cycle, race/ethnicity, sex, income-to-poverty ratio, insurance status, general health status, and number of healthcare provider (HCP) visits in the previous year.
Several child sociodemographic characteristics were significantly associated with reported HCP identification of overweight, including age and race/ethnicity (see Table 2). In adjusted models, the probability of reported identification was higher for 6- to 11-year-old youth (21.5%; 95% CI: 19.7–23.3) and 12- to 15-year-old youth (31.7; 95% CI: 29.0–34.5), compared to 2- to 5-year-old children (14.4; 95% CI: 11.9–16.8). Non-Hispanic white children had the lowest probabilities of HCP identification (20.5%; 95% CI: 18.4–22.6), compared to 26.7% of non-Hispanic black children (95% CI: 24.5–28.9) and 26.7% of Mexican-American children (95% CI: 23.9–29.5). Additionally, several child health-related characteristics were also significantly associated with reported HCP identification of overweight. The probability of reported identification was lowest among children not visiting a physician in the previous year (17.3%; 95% CI: 13.6–21.0), compared to children reporting 1–3 or 4 + physician visits in the previous year (23.9%; 95% CI: 22.0–25.7 and 25.1%; 95% CI: 22.1–28.1, respectively). Compared to children reporting excellent general health (19.5%; 95% CI: 17.0–22.0), the likelihood of caregivers reporting that the child had been identified as overweight were significantly greater for children reporting good health (28.3%; 95% CI: 25.3–31.3) and children reporting fair or poor health (30.3; 95% CI: 23.9–36.6).
Finally, the adjusted probability of reported HCP identification was significantly higher in 2007–2008 (27.8; 95% CI: 24.6–31.0) and in 2009–2010 (24.8; 95% CI: 22.1–27.4), compared to 2001–2002 (20.0%; 95% CI: 16.5–23.5). We also examined whether there was an overall trend toward increasing reported HCP identification of overweight, and results suggest that there was a 1.2% increase in the adjusted probability of reported HCP identification for each 2-year survey cycle (95% CI: 0.3–2.2). A complete description of uni- and multivariable logistic regression models can be seen in Table 3.
Table 3.
Results of Uni- and Multivariable Logistic Regression Models Describing the Odds of HCP Identification of Overweight by Child Characteristics
| Unadjusted ORs (95% CI) | Adjusted ORs (95% CI) | |
|---|---|---|
| 2001–2002 | Ref | Ref |
| 2003–2004 | 1.19 (0.85–1.67) | 1.43 (1.02–1.99)* |
| 2005–2006 | 0.97 (0.67–1.40) | 0.93 (0.65–1.35) |
| 2007–2008 | 1.65 (1.20–2.27)* | 1.72 (1.22–2.41)* |
| 2009–2010 | 1.39 (0.99–1.95) | 1.41 (1.02–1.95)* |
| 2–5 years | Ref | Ref |
| 6–11 years | 1.91 (1.50–2.43)* | 1.81 (1.34–2.45)* |
| 12–18 years | 2.59 (1.97–3.41)* | 3.53 (2.60–4.80)* |
| Female | 1.03 (0.90–1.18) | 1.19 (0.99–1.44) |
| Race or ethnicitya | ||
| Non-Hispanic white | Ref | Ref |
| Non-Hispanic black | 1.54 (1.28–1.86)* | 1.54 (1.23–1.93)* |
| Mexican American | 1.57 (1.32–1.88)* | 1.54 (1.19–1.98)* |
| PIR | ||
| < 100% FPT | Ref | Ref |
| 101–200% FPT | 0.91 (0.73–1.14) | 1.02 (0.79–1.33) |
| 201–400% FPT | 0.62 (0.49–0.79)* | 0.73 (0.53–1.00)* |
| > 400% FPT | 0.77 (0.56–1.08) | 1.18 (0.81–1.73) |
| No. of healthcare visits | ||
| 0 | Ref | Ref |
| 1–3 | 1.60 (1.19–2.14)* | 1.65 (1.16–2.35)* |
| 4 + | 1.85 (1.38–2.47)* | 1.79 (1.28–2.51)* |
| Insured | 1.27 (1.03–1.57)* | 1.30 (0.96–1.75) |
| General health condition | ||
| Excellent | Ref | Ref |
| Very good | 1.66 (1.26–2.20)* | 1.37 (1.00–1.87) |
| Good | 2.51 (2.00–3.15)* | 1.82 (1.36–2.44)* |
| Fair or poor | 3.47 (2.39–5.03)* | 2.05 (1.32–3.17)* |
| Overweight and WC < 85% | Ref | Ref |
| Overweight and WC 85–94.9% | 0.84 (0.42–1.68) | 1.26 (0.59–2.71) |
| Overweight and WC ≥ 95% | 1.05 (0.33–3.30) | 1.60 (0.58–4.46) |
| Obese and WC < 85% | 2.50 (1.87–3.35)* | 2.39 (1.70–3.35)* |
| Obese and WC 85–94.9% | 5.13 (4.09–6.44)* | 5.08 (3.94–6.55)* |
| Obese and WC ≥ 95% | 9.52 (7.15–12.69)* | 12.63 (8.98–17.76)* |
Because of small sample sizes of children identifying as races and ethnicities other than non-Hispanic white, non-Hispanic black, and Mexican American, results are not presented for these children, though they were included in the analytic sample.
Significant at p < 0.05.
HCP, healthcare provider; OR, odds ratio; CI, confidence interval; PIR, income-to-poverty ratio; FPT, federal poverty threshold; WC, waist circumference.
Discussion
Although rates of reported HCP identification of child overweight have improved significantly over the past decade, more than 3 in 4 overweight or obese children (76%) are not reported by a caregiver as being identified as overweight by an HCP. These results are consistent with previous studies reporting that only a minority of overweight or obese children are identified as such by physicians.13,18,19,21–23,37–39 Brief, relatively simple interventions have been shown to improve weight screening and communication practices among physicians,40–42 which have, in turn, been associated with more accurate parent perception of child weight status and positive health behaviors related to diet and activity.23 Future studies might investigate the feasibility and utility of implementing these interventions on a wider scale.
Caregiver report of HCP identification was positively associated with abdominal adiposity and weight status (i.e., overweight or obesity) in unadjusted models. There was a significant weight status by WC interaction, whereby the positive association between abdominal adiposity and reported HCP identification of overweight were observed for obese children, but not overweight children. Although there was no significant association between WC and reported HCP identification among overweight children, the proportion of overweight children identified was small and perhaps limited the capacity to detect a pattern by WC in this group. With respect to the obese children, it is possible that abdominal adiposity may serve as a visual cue to providers,30 prompting them to screen children or communicate weight status to parents. Alternatively, parents of abdominally adipose children may be more likely to perceive their children as overweight and therefore more likely to recall being notified by an HCP, because this information was consistent with their own conceptions of their child’s weight status. Importantly, this also suggests that parents of obese children with lower levels of abdominal adiposity may not perceive their child to be overweight and may therefore be less likely to remember being alerted by an HCP, because this information may be discordant with their earlier beliefs. An important corollary of this finding is that despite the existence of universal BMI screening guidelines, providers and parents may be influenced by subjective perceptions of child weight status, instead of relying on objective measures. Existing clinical recommendations describe the inadequacies of relying on perceptions, stating that “although clinicians visually recognize obesity in many children without seeing the plotted BMI values, they may overlook excess body fat in children (p. S174),”13 and subsequently miss “opportunities to guide the family toward healthier behaviors (p. S174).”13
Finally, it is possible that children with higher BMI and WC percentiles are more likely to suffer from weight-related health conditions that lead to more frequent HCP identification of overweight or better parental recall of such notification. However, WC remained significant even after we controlled for general health status and number of HCP visits in the previous year. Because no studies to date have examined WC in relation to HCP identification of pediatric overweight, these mechanisms remain unclear. Future studies might examine whether WC may be a useful indicator of obesity-related health risks among children.
Consistent with earlier research documenting increases in HCP identification over time,22 the odds of overweight or obese children being identified by an HCP increased significantly from 2001–2002 to 2007–2008 and remained higher in 2009–2010. In 2007, recommendations were issued to change the terminology used to describe pediatric obesity from “at-risk of overweight” and “overweight” to “overweight” and “obese,” respectively.40 This change may have resulted in clearer communication regarding weight status of children, or increased comprehension and recall by parents. The uptick of HCP identification in 2007–2008 may also reflect adherence to screening recommendations that were issued around that time.13 Future studies may examine these potential time trends further when subsequent NHANES data become available.
In this analysis, non-Hispanic white children were less likely to be identified as overweight by an HCP, compared to non-Hispanic black or Hispanic children. Previous studies have reported that black and Hispanic patients may be more likely to receive a diagnosis of overweight or obesity or be counseled for weight, compared to non-Hispanic white patients.18,19,39 One recent study suggested that this pattern may be a consequence of provider awareness of weight-related disparities, where non-Hispanic black and Hispanic individuals are at greater risk of obesity.39 More research is needed to examine provider characteristics in association with weight screening patterns and communication to patients.
Although more than half of pediatricians report routine BMI screening,38,43–45 less than 24% of parents report being told that their child is overweight. There are several possible explanations for this discrepancy. First, because the question about identification is based on parental recall, it is possible that physicians are communicating weight status to parents, but that parents are unable or unwilling to comprehend the information provided, or they do not remember that this information was provided when asked. For example, if providers are using the older terminology of “at-risk for overweight” to describe children with BMI percentiles ≥ 85, parents may not report being told by an HCP that their child is overweight. Second, physicians may be screening and documenting children’s weight status, but failing to communicate this adequately to parents. There are several barriers to weight-related communication between HCPs and parents, including the belief that parents do not want to discuss children’s weight and the stigma that overweight and obese children often endure.46 Additionally, providers may not feel equipped to address pediatric obesity in clinical practice.30,38,45 Third, physicians may be over-reporting screening practices. Studies of medical records have found that actual documentation of child weight status by pediatricians is much lower than reported screening rates.18,44
Our findings are limited by the reliance on cross-sectional and observational data as well as reliance on proxy report. The caregiver responding in NHANES may not be the one who typically accompanies children to HCP visits and therefore might be unaware of conversations related to child weight status. Additionally, it is possible that some children became overweight or obese between the time when the child last visited an HCP and the time point at which the child participated in NHANES. Our estimates may therefore underestimate the proportion of overweight or obese children who are identified by an HCP. Finally, we did not have any information about provider characteristics that may be related to weight-screening practices.
There are several strengths to be noted. First, data are based on a large, nationally representative sample of children in the United States, allowing us to look at rates of reported HCP identification across several different sociodemographic characteristics. Second, this is the first study that we are aware of to examine health-related variables such as abdominal adiposity in relation to the likelihood that caregivers recall being notified by an HCP that their child is overweight or obese. The findings of the present study indicate that among obese children, caregivers are more likely to report being notified of their child’s weight status by an HCP if the child has a higher waist circumference. More research is needed to explore the relationships between child characteristics, parent weight perceptions, and HCP identification of overweight.
Conclusions
Though the proportion of overweight or obese children identified by an HCP has increased over the past decade, 75% of caregivers of overweight or obese children do not report being told about their child’s weight status by an HCP. Reported identification of overweight by an HCP is higher among obese children, and lower levels of abdominal adiposity were also associated with lower probabilities of reported HCP identification of overweight among this group. Despite existing clinical guidelines supporting “a shift from simple identification of obesity, which often occurs when the condition is obvious and intractable, to universal assessment, universal preventive health messages, early intervention…[and] assessment of obesity risk for all patients, with anticipatory guidance on healthy behaviors to minimize that risk (p. S169),”13 our findings suggest that visual cues of adiposity, such as waist circumference, may be influencing caregiver recall of HCP notification of overweight or obesity. Additionally, a variety of parent and provider characteristics may affect weight-related communications and caregiver recall of such information; these issues should be explored in future research.
Acknowledgments
The findings and conclusions in this article are those of the author(s) and do not necessarily represent the official position of the National Center for Health Statistics, Centers for Disease Control and Prevention.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 4.Lobstein T, Baur L, Uauy R, et al. Obesity in children and young people: A crisis in public health. Obes Rev. 2004;5:S4–S104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 5.Singh AS, Mulder C, Twisk JW, et al. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev. 2008;9:474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 6.Kant AK, Miner P. Physician advice about being overweight: Association with self-reported weight loss, dietary, and physical activity behaviors of US adolescents in the National Health and Nutrition Examination Survey, 1999–2002. Pediatrics. 2007;119:E142–E147. doi: 10.1542/peds.2006-1116. [DOI] [PubMed] [Google Scholar]
- 7.Loureiro ML, Nayga RM. Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62:2458–2468. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Chaimovitz R, Issenman R, Moffat T, et al. Body perception: Do parents, their children, and their children’s physicians perceive body image differently? J Pediatr Gastr Nutr. 2008;47:76–80. doi: 10.1097/MPG.0b013e31815a34. [DOI] [PubMed] [Google Scholar]
- 9.Doolen J, Alpert PT, Miller SK. Parental disconnect between perceived and actual weight status of children: A metasynthesis of the current research. J Am Acad Nurse Prac. 2009;21:160–166. doi: 10.1111/j.1745-7599.2008.00382.x. [DOI] [PubMed] [Google Scholar]
- 10.Huang JS, Becerra K, Oda T, et al. Parental ability to discriminate the weight status of children: Results of a survey. Pediatrics. 2007;120:E112–E119. doi: 10.1542/peds.2006-2143. [DOI] [PubMed] [Google Scholar]
- 11.Parry LL, Netuveli G, Parry J, et al. A systematic review of parental perception of overweight status in children. J Ambul Care Manage. 2008;31:253–268. doi: 10.1097/01.JAC.0000324671.29272.04. [DOI] [PubMed] [Google Scholar]
- 12.Hernandez RG, Cheng TL, Serwint JR. Parents’ healthy weight perceptions and preferences regarding obesity counseling in pre-schoolers: Pediatricians matter. Clin Pediatr. 2010;49:790–798. doi: 10.1177/0009922810368288. [DOI] [PubMed] [Google Scholar]
- 13.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 14.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert committee recommendations. Pediatrics. 1998;102:E29. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 15.Krebs NF, Baker RD, Greer FR, et al. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Family Physicians. Practical Advice for Family Physicians to Help Overweight Patients. AAFP; Leawood, KS: 2003. [Last accessed June 14, 2013]. Available at http://eatbettermovemore.org/SA/enact/healthcare/documents/healthcare.rolemodels.tools.obesitymonograph.pdf. [Google Scholar]
- 17.Barton M US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125:361–367. doi: 10.1542/peds.2009-2037. [DOI] [PubMed] [Google Scholar]
- 18.Benson L, Baer HJ, Kaelber DC. Trends in the diagnosis of overweight and obesity in children and adolescents: 1999–2007. Pediatrics. 2009;123:E153–E158. doi: 10.1542/peds.2008-1408. [DOI] [PubMed] [Google Scholar]
- 19.Dorsey KB, Wells C, Krumholz HM, et al. Diagnosis, evaluation, and treatment of childhood obesity in pediatric practice. Arch Ped Adolesc Med. 2005;159:632–638. doi: 10.1001/archpedi.159.7.632. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton JL, James FW, Bazargan M. Provider practice, overweight and associated risk variables among children from a multi-ethnic underserved community. J Natl Med Assoc. 2003;95:441–448. [PMC free article] [PubMed] [Google Scholar]
- 21.Louthan MV, Lafferty-Oza MJ, Smith ER, et al. Diagnosis and treatment frequency for overweight children and adolescents at well child visits. Clin Pediatr. 2005;44:57–61. doi: 10.1177/000992280504400107. [DOI] [PubMed] [Google Scholar]
- 22.Perrin EM, Skinner AC, Steiner MJ. Parental recall of doctor communication of weight status: National trends from 1999 through 2008. Arch Ped Adolesc Med. 2012;166:317–322. doi: 10.1001/archpediatrics.2011.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perrin EM, Vann JCJ, Benjamin JT, et al. Use of a pediatrician toolkit to address parental perception of children’s weight status, nutrition, and activity behaviors. Acad Pediatr. 2010;10:274–281. doi: 10.1016/j.acap.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernandez JR, Redden DT, Pietrobelli A, et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145:439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 25.Pietrobelli A, Fernandez J, Redden DT, et al. Waist circumference percentiles in nationally representative samples of black, white, and Hispanic children. [Conference abstract presented at the 13th European Congress on Obesity, Prague, Czech Republic, May 2004.] Int J Obes. 2004;28:S201. [Google Scholar]
- 26.Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord. 2000;24:1453–1458. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]
- 27.Taylor RW, Jones IE, Williams SM, et al. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 y. Am J Clin Nutr. 2000;72:490–495. doi: 10.1093/ajcn/72.2.490. [DOI] [PubMed] [Google Scholar]
- 28.Juliusson PB, Roelants M, Markestad T, et al. Parental perception of overweight and underweight in children and adolescents. Acta Paediatr. 2011;100:260–265. doi: 10.1111/j.1651-2227.2010.02039.x. [DOI] [PubMed] [Google Scholar]
- 29.Parkinson KN, Drewett RF, Jones AR, et al. When do mothers think their child is overweight? Int J Obes. 2011;35:510–516. doi: 10.1038/ijo.2010.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Voelker R. Improved use of BMI needed to screen children for overweight. JAMA. 2007;297:2684–2685. doi: 10.1001/jama.297.24.2684. [DOI] [PubMed] [Google Scholar]
- 31.National Center for Health Statistics. [Last accessed June 14, 2013];National Health and Nutrition Examination Survey: Questionnaires, datasets, and related documentation. Available at www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 32.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;8:1–27. [PubMed] [Google Scholar]
- 33.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 34.McDowell MA, Fryar CD, Hirsch R, et al. Anthropometric reference data for children and adults: US population, 1999–2002. Adv Data. 2005;7:1–5. [PubMed] [Google Scholar]
- 35.StataCorp. Stata Statistical Software. StataCorp LP; College Station, TX: 2011. Release 12 ed. [Google Scholar]
- 36.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hillman JB, Corathers SD, Wilson SE. Pediatricians and screening for obesity with body mass index: Does level of training matter? Public Health Rep. 2009;124:561–567. doi: 10.1177/003335490912400413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klein JD, Sesselberg TS, Johnson MS. Adoption of body mass index guidelines for screening and counseling in pediatric practice. Pediatrics. 2010;125:265–272. doi: 10.1542/peds.2008-2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liang L, Meyerhoefer C, Wang J. Obesity counseling by pediatric health professionals: An assessment using nationally representative data. Pediatrics. 2012;130:67–77. doi: 10.1542/peds.2011-0596. [DOI] [PubMed] [Google Scholar]
- 40.Krebs NF, Himes JH, Jacobson D, et al. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 41.Nicholas J, Dennison BA, de Long R, et al. Randomized controlled trial of a mailed toolkit to increase use of body mass index percentiles to screen for childhood obesity. Prev Chron Dis. 2009;6:A122. [PMC free article] [PubMed] [Google Scholar]
- 42.Oettinger MD, Finkle JP, Esserman D, et al. Color-coding improves parental understanding of body mass index charting. Acad Pediatr. 2009;9:330–338. doi: 10.1016/j.acap.2009.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barlow SE, Dietz WH, Klish WJ, et al. Medical evaluation of overweight children and adolescents: Reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110:222–228. [PubMed] [Google Scholar]
- 44.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:154–159. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 45.Sesselberg TS, Klein JD, O’Connor KG, et al. Screening and counseling for childhood obesity: Results from a national survey. J Am Board Fam Med. 2010;23:334–342. doi: 10.3122/jabfm.2010.03.090070. [DOI] [PubMed] [Google Scholar]
- 46.Latner JD, Stunkard AJ. Getting worse: The stigmatization of obese children. Obes Res. 2003;11:452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]