Abstract
AIM: To investigate the role of TGFβ1 in invasion and metastasis in colorectal cancer by analysing TGFβ1 correlated with depth of tumor invasion, stage and metastasis.
METHODS: Serum TGFβ1 levels were determined in 50 patients with colorectal cancer and 30 healthy volunteers using a TGFβ1 enzyme-linked immunosorbent assay. TGFβ1 expression in primary and lymph node metastatic lesions were detected in 98 cases of colorectal cancer by immunohistochemical staining and in situ hybridization.
RESULTS: Serum levels of TGFβ1 in patients with colorectal cancer (40 ± 18 μg·L-1) were significantly higher than those in the healthy control group (19 ± 8 μg·L-1), P < 0.05. Elevated levels of serum TGFβ1 were found in 60% of patients with colorectal cancer when the mean +2 s was used as the upper limit of the normal range (35.1 μg·L-1). Increases in serum TGFβ1 levels were significantly associated with Duke's stage (P < 0.05), but there was no significant difference between Duke's stage B patients and Duke's stage C patients. In the cytoplasm of cancer cells, TGFβ1 was immunostained in 37.8% (37/98) of colorectal cancer, and this expression was confirmed by in situ hybridization. Among 35 cases of colorectal cancer with lymph node metastatic lesions, TGFβ1 positive staining was found in 18 (51.4%) cases of primary tumor, and 25 (71.4%) cases with lymph node metastatic lesions, respectively. Of 17 cases w ith no staining in the primary lesion, 7 (41.2%) casesshowed TGFβ1 staining in the metastatic lesion. Serum TGFβ1 levels and TGFβ1 expression in colorectal cancer tissues were correlated significantly with depth of tumor invasion, stage and metastasis. Patients in stage C-D, T3-T4 and with metastasis had significantly higher TGFβ1 levels than patients in stage A-B, T1-T2 and without metastasis (P < 0.05).
CONCLUSION: These results suggest that transforming growth factor-β1 is closely related to the invasion and metastasis of colorectal cancer. It increased the invasive and metastatic potential of tumor by altering a tumor microenvironment. TGFβ1 may be used as a possible biomarker.
INTRODUCTION
The incience of colorectal cancer has become high in China and its biology is a hot topic of research[1-44]. Tumor invasion and metastasis are complex processes in which cancer cells detach from the original tumor mass to establish metastatic foci at distant sites. Metastatic cells characteristically lose growth inhibitory responses, undergo alteration in adhesiveness and demonstrate enhanced production of enzymes that can degrade extracellular matrix components. Since it is the development of metastatic disease that is primarily responsible for cancer mortality, an understanding of the mechanisms that facilitate metastatic tumor progression is of great importance[1]. Transforming growth factor (TGF)-β1 is a 25-kd polypeptides. This growth factor regulates cell growth and differentiation in both normal and transformed cells. TGF-β1 was found to inhibit the growth of normal and neoplastic cells. Resistance to the negative growth-regulating properties of TGF-β1 has been observed in epithelial and mesenchymal tumors. Tumor cell lines that lack TGF-β receptors lose responsiveness to TGF-β1, and the escape of cells from TGF-β1 mediated negative regulation is linked to tumor progression[45]. Colorectal cancer is one of the most malignant neoplasms. TGF-β1 plays a crucial role in tumor extension. We examined the expression of TGF-β1 in primary and lymph node metastatic lesions in colorectal cancer, as well as serum TGF-β1 levels in the peripheral veins. Our objective is to determine the clinical significance of TGF-β1 in advance of colorectal cancer.
MATERIALS AND METHODS
Patients
Serum TGF-β1 assays were performed in 50 patients treated from July 1999 to June 2000. There were 32 men and 18 women, and their age ranged from 23 to 74 years (means, 53 ± 11 years). According to Duke's staging criteria, 9 cases were stage I, 18 stage II, 18 stage III and 5 stage IV. Thirty healthy volunteers were selected as control group among whom there were 17 men and 13 women. Their age ranged from 20 to 56 years (means, 45 ± 8 years).
A total of 98 colorectal adenocarcinoma patients (including the 50 patients above) who had undergone surgical resection in the Affiliated Zhongnan Hospital of Wuhan University (Wuhan, China) from July 1998 to December 2000, TGFβ1 and TGFβRII immunohistochemical staining and in situ hybridization were performed. There were 53 men and 45 women, and their age ranged from 23 to 74 years (means, 56 ± 11 years). Among 98 patients, 17 were well differentiated adenocarcinoma, 47 moderately differentiated adenocarcinoma and 34 poorly differentiated adenocarcinoma. According to Duke's staging criteria, 34 cases were stage I, 29 stage II, 30 stage III and 5 stage IV.
Methods
Preparation of serum sample and TGFβ1 assay Two mL of blood sample, collected from the peripheral vein before surgery, were stored for approximately 3 h at 4 °C until the samples were centrifuged. Blood samples were centrifuged at 3000 g for 20 min. The serum was separated and stored frozen at -70 °C until the time of analysis. TGFβ1 was assayed using human TGFβ1 enzyme-linked immunoabsorbent assay kits. The ELISA kits were obtained from Quantikine Co. of USA. The TGFβ1 assay was performed according to the methods outlined in the package insert. Standard samples of 200 μg were added to each well, and incubated for 3 h at room temperature. After complete wash of each well, 200 μL TGFβ1 conjugate was added to each well and these were incubated for 1.5 h at room temperature. We repeated the aspiration/wash and added 200 μL of substrate solution to each well and incubated for 20 min. Finally, we added 50 μL of stop solution and absorbances in each well were measured using a spectrophotometric plate reader at a wavelength of 490 nm. To determine the TGF-β1 concentration in each sample, we first calculated the average absorbance value in each set of duplicates. Serum levels of TGF-β1 were calculated from linear regression equation.
Immunohistochemistry All the tissue specimens were fixed in 100 mL•L-1 neutral formalin and embedded in paraffin. Five-um thick sections were xylene dehydrated in ethanol. Tissue sections were washed three times in 0.05 mol·L-1 PBS, and incubated in endogenous peroxidase blocking solution. Non-specific antibody binding was blocked by pretreatment with PBS containing 5 g•L-1 bovin serum albumin. Sections were then rinsed in PBS and incubated overnight at 4 °C with diluted anti-TGFβ1 and anti-TGFβRII protein polyclonal antibody. The steps were performed using Immunostain kit according to the manufacturer’s instructions. PBS was used as substitutes of protein antibody for negative control groups. The sections were examined under light microscopy. Anti-TGFβ1 and anti-TGFβRII protein polyclonal antibody were purchased from Bosden Comp. (Wuhan, China). S-P detection kit was purchased from Fuzhou Maixin Comp. (Fuzhou, China). Anti-TGFβ1 and anti-TGFβRII protein polyclonal antibody were diluted to 1:100.
In situ hybridization All the tissue specimens were fixed in 100 mL•L-1 neutral formalin and embedded in paraffin. Six-um thick sections were xylene dehydrated in ethanol, and digested with 10 mg•L-1 proteinase for 10 min. Sections were washed in 0.5 mol·L-1 PBS for 15 min. They were incubated overnight at 37 °C with the 500 μg•L-1 digoxigenin-labeled RNA probe in hybridization buffer. After hybridization, sections were washed in 2 × SSC for 10 min at 37 °C and finally in 0.2 × SSC for 15 min at 37 °C. Sections were incubated with alkaline phosphatase-conjugated anti-digoxigenin antibody for 60 min at 37 °C. The steps were performed using in situ hybridization kit according to the manufacturer's instructions. The kits were purchased from Bosden Comp. (Wuhan, China).
TGFβ1 in situ hybridization probe sequences were:
(1)5-CGTTTCACCAGCTCCATGTCGATGGTCTTGCAAT-3'
(2)5-CTTGATTTTAATCTCTGCAAGCGCAGCTCTGCACG-3'
(3)5-TTGGTATCCAGGGCTCTCCGGTGCCGTGAGCTGTG-3'
Statistical analysis
The difference between each group was analyzed by Chi-square test and correlativity.
The limit of significant difference was P < 0.05.
RESULTS
Serum TGFβ1 levels in patients with colorectal cancer
Serum TGFβ1 levels in patients with colorectal cancer (40.4 ± 17.6 μg•L-1) were significantly higher than in normal controls (19.2 ± 8.0 μg•L-1), P < 0.01. Elevated levels of serum TGFβ1 were found in 60% of patients with colorectal cancer when the mean +2 s was used as the upper limit of the normal range (35.1 μg•L-1, Figure 1). Increased in serum TGFβ1 levels were significantly associated with Duke's stage (P < 0.05), but there was no significant difference between Duke's stage B patients and Duke's stage C patients. Serum levels of TGFβ1 were 29.2 ± 7.3 μg•L-1 in Duke's stage A patients, 39.5 ± 11.9 μg•L-1 in Duke's stage B patients, 43.1 ± 15.8 μg•L-1 in Duke's stage C patients, and 57.8 ± 16.2 μg•L-1 in Duke's tage D patients. Serum levels of TGFβ1 in each stage were significantly higher than those in the control group (Figure 2). Serum levels of TGFβ1 were not correlated with age, gender, tumor size and differentiation degree of tumor.
Figure 1.
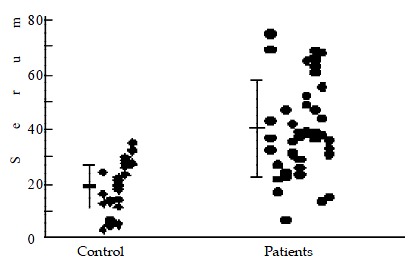
Serum TGFβ1 in patients with colorectal cancer. Bars represent mean ± standard deviation.
Figure 2.
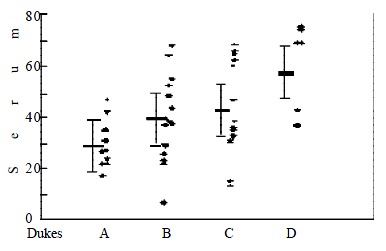
Serum TGFβ1 in patients with colorectal cancer according to Duke's stage. Bars represent mean ± standard deviation.
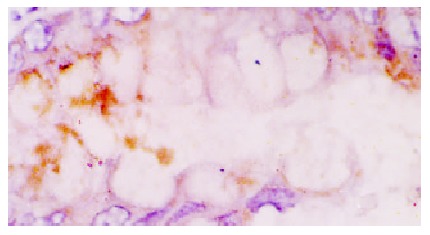
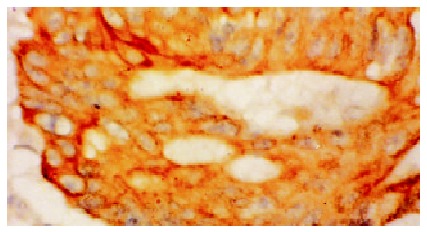
TGFβ1 and TGFβRII Expression in colorectal cancer tissue The TGFβ1 and TGFβRII protein were stained mainly in the cytoplasm and cell membrane of cancer cells, as shown in Figure 3 and Figure 4. Staining was classified as negative if less than 10% of the cells were positive and as positive if more than 10% were positive[2]. Thirty-seven (37.8%) of 98 tissues from colorectal cancer patients were positive for TGFβ1 staining and forty-six (46.9%) were positive for TGFβRII staining. The expression of TGFβ1 and TGFβRII was correlated significantly with the depth of invasion, stage of disease and metastasis (lymph node and distant metastasis). Patients in T3-T4, stage C-D and with metastasis had significantly higher expression of TGFβ1 than patients in T1-T2, stage A-B and without metastasis (P < 0.05). Patients in T3-T4, stage C-D and with metastasis had significantly lower expression of TGFβRII than patients in T1-T2, stage A-B and without metastasis (P < 0.05). The expression of TGFβ1 and TGβRII was not correlated with age, gender, tumor size and differentiation degree of tumor (Table 1).
Figure 3.
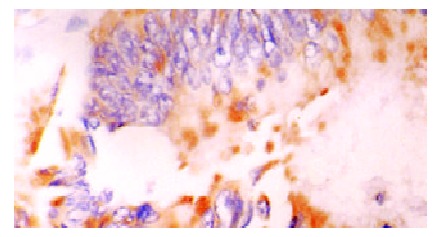
TGFβ1 staining in cytoplasm of cancer cells. × 400
Figure 4.
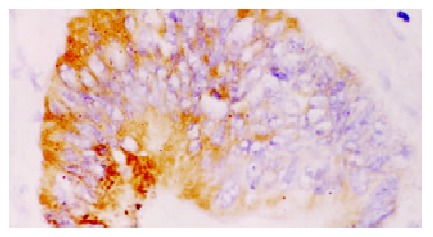
TGFβRII staining in cytoplasm of cancer cells. × 400
Table 1.
Clinicopathologic characteristics of colorectal cancer with expression of TGFβ1 and TGFβRII
| Variables | n | TGFβ1-positive n (%) | TGFβRII-positive n (%) | |
| Age (yrs) | ≥ 50 | 60 | 24 (40.0) | 30 (50.0) |
| < 50 | 38 | 13 (34.2) | 16 (42.1) | |
| Sex | Male | 53 | 20 (41.5) | 25 (53.7) |
| Female | 45 | 17 (31.0) | 21 (37.9) | |
| Tumor size | < 5 cm | 56 | 21 (37.5) | 24 (42.9) |
| ≥ 5 cm | 42 | 16 (38.1) | 22 (52.4) | |
| Histology | ||||
| Well-diff. ade | 17 | 9 (52.9) | 11 (64.7) | |
| Mode-diff. ade | 47 | 15 (31.9) | 19 (40.4) | |
| Poor-diff. ade | 34 | 13 (38.2) | 16 (47.1) | |
| Depth of invasion | ||||
| T1-T2 | 60 | 17 (28.3) | 33 (55.0) | |
| T3-T4 | 38 | 20 (52.6)a | 13 (34.2)a | |
| Metastasis | Present | 35 | 18 (51.4) | 11 (31.4) |
| Absent | 63 | 19 (30.2)a | 35 (55.6)a | |
| Stage | A | 34 | 8 (23.5) | 23 (67.7) |
| B | 29 | 9 (31.1) | 13 (44.8) | |
| C+D | 35 | 20 (57.1)a | 10 (28.6)a | |
aP < 0.05, T1-T2 vs T3-T4, Present vs Absent, A, B vs C+D
TGFβ mRNA expression in colorectal cancer tissue
The expression of TGFβ1 mRNA in 50 colorectal cancer tissues was examined. The degree of staining was prominent in cases of TGFβ1 positive immunohistochemical staining, but it was rare for negative cases of immunohistochemical staining. The pattern of distribution of TGFβ1 mRNA is the same as immunohistochemical staining (Figure 5).
Figure 5.
TGFβ1 mRNA expression in colorectal cancer in situ hybridization. × 400
Relationship of TGFβ1 expression between primary and lymph node metastic lesions Among 35 cases of colorectal cancer with lymph node metastatic lesions, the TGFβ1 positive rate was 51.4% (18/35) for primary lesions and 71.4% (25/35) for metastatic lesions in the lymph nodes. Of 17 cases with no staining in the primary lesion, 7 cases (41.2%) showed TGFβ1 staining in the metastatic lesion (Figure 6).
Figure 6.
TGFβ1 Expression in lymph node metastatic lesions. × 400
DISCUSSION
TGFβ1 has been found to be overexpressed locally in many tumors, and is believed to play a role in tumor transformation and progression, as well as in tumor regression[46-48]. Although TGFβ1 acts as a potent inhibitor of cell growth and tumor progression, loss of this negative regulation can lead to tumor development. TGFβ1 switches to a growth stimulator with tumor progression. Growth inhibition is replaced in many tumors by the opposite response, growth stimulation. This paradoxical switch in the responsiveness of tumor cell to TGFβ1 during neoplastic progression may be due to the inactivation of the TGFβ1 signaling pathway such as mutations in the type 2 TGFβ receptor gene or through reduced expression and increase of blood supply to a tumor mass and inhibition of immunologic mechanisms involved in tumor identification and cytolysis. In cases of breast cancer, expression of TGFβ1 was positively associated with invasion and matastasis. Maehara et al[45] reported that the expression of TGFβ1 in gastric cancer cells was closely related to infiltrative growth of the cancer and to the higher rate of lymph node metastasis.
We found that TGFβ1 levels in the serum of patients with colorectal cancer were significantly elevated compared with normal controls. TGFβ1 was overexpressed in colorectal cancer tissue compared with normal colorectal mucosa. Elevated serum levels of TGFβ1 and over-expression of TGFβ1 in colorectal cancer tissue were correlated significantly with invasion and metastasis of colorectal cancer. Patients in T3-T4, stage C-D and with metastasis had significantly higher expression of TGFβ1 in tumor tissue and TGFβ1 levels in the serum than patients in T1-T2, stage A-B and without metastasis (P < 0.05). The expression of TGFβ1 in tumor tissue and TGFβ1 levels in the serum were not correlated with age, gender and differentiation degree of tumor. Shim et al[49] reported that patients of colorectal cancer in stage C-D had significantly higher expression of TGFβ1 in tumor tissues and TGFβ1 levels in the serum than patients in stage A-B (P < 0.05). TGFβ1 in colorectal cancer patients may be associated with disease progression. Among 35 cases of colorectal cancer with lymph node metastasis lesions, the TGFβ1 positive rate was 51.4% (18/35) for primary lesions and 71.4% (25/35) for metastatic lesions in the lymph nodes. Of 17 cases with no staining in the primary lesion, 7 cases (41.2%) showed TGFβ1 staining in the metastatic lesion. The preferential expression of TGFβ1 in lymph node metastases suggests a clonal selection of tumor cells with TGFβ1 expression, specific for the higher potential of lymph node metastasis in tumor advance, and TGFβ1 plays a role related to the malignant progression of colorectal cancer. We also found that TGFβRII expression was significantly lower in colorectal cancer tissues than in normal mucosa. The expression of TGFTGFβRII in tumor tissues of Patients in T3-T4, stage C-D and with metastasis was significantly lower than that in patients in T1-T2, stage A-B and without metastasis (P < 0.05). The expression of TGFβRII in tumor tissues was not correlated with age, gender and differentiation degree of tumor. The lower expression of TGFβRII in colorectal cancer may be associated with disease progression. In our previous study[50,51], we found that TGFβ1 expression was correlated significantly with angiogenesis in colorectal cancer tissues and inhibition of immunologic mechanisms involved in tumor identification and cytolysis. TGFβ1 is closely related to the invasion and matastasis of colorectal cancer, and it may be used as a possible biomarker.
Footnotes
Edited by Ma JY
Supported by Hubei Province Natural Science Foundation, No.2000J054
References
- 1.McEarchern JA, Kobie JJ, Mack V, Wu RS, Meade-Tollin L, Arteaga CL, Dumont N, Besselsen D, Seftor E, Hendrix MJ, et al. Invasion and metastasis of a mammary tumor involves TGF-beta signaling. Int J Cancer. 2001;91:76–82. doi: 10.1002/1097-0215(20010101)91:1<76::aid-ijc1012>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 2.Xiao B, Jing B, Zhang YL, Zhou DY, Zhang WD. Tumor growth inhibition effect of hIL-6 on colon cancer cells transfected with the target gene by retroviral vector. World J Gastroenterol. 2000;6:89–92. doi: 10.3748/wjg.v6.i1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang PL, Zhu SN, Lu SL, Dai ZS, Jin YL. Inhibitor of fatty acid synthase induced apoptosis in human colonic cancer cells. World J Gastroenterol. 2000;6:295–297. doi: 10.3748/wjg.v6.i2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie B, He SW, Wang XD. Effect of gastrin on protein kinase C and its subtype in human colon cancer cell line SW480. World J Gastroenterol. 2000;6:304–306. doi: 10.3748/wjg.v6.i2.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo WJ, Zhou GD, Wu HJ, Liu YQ, Wu RG, Zhang WD. Ultrastructural localization of glutathione S-transferase-pi in human colorectal cancer cells. World J Gastroenterol. 2000;6:454–455. doi: 10.3748/wjg.v6.i3.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuan P, Sun MH, Zhang JS, Zhu XZ, Shi DR. APC and K-ras gene mutation in aberrant crypt foci of human colon. World J Gastroenterol. 2001;7:352–356. doi: 10.3748/wjg.v7.i3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng CX, Zhan WH, Zhao JZ, Zheng D, Wang DP, He YL, Zheng ZQ. The prognostic value of preoperative serum levels of CEA, CA19-9 and CA72-4 in patients with colorectal cancer. World J Gastroenterol. 2001;7:431–434. doi: 10.3748/wjg.v7.i3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peng ZH, Xing TH, Qiu GQ, Tang HM. Relationship between Fas/FasL expression and apoptosis of colon adenocarcinoma cell lines. World J Gastroenterol. 2001;7:88–92. doi: 10.3748/wjg.v7.i1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li XG, Song JD, Wang YQ. Differential expression of a novel colorectal cancer differentiation-related gene in colorectal cancer. World J Gastroenterol. 2001;7:551–554. doi: 10.3748/wjg.v7.i4.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang W, Luo HS, Yu BP. Telomerase and colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:800–802. [Google Scholar]
- 11.Ying YQ, Zhou G, Wu P. Huang WB. Significance of TGF-a and TGF-β1 expressions in the tissue of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:223–225. [Google Scholar]
- 12.Xie B, He SW, Wang DK. Inhibition of neomycin on gastrin-stimulating cell proliferation of human colon cell line SW480. Shijie Huaren Xiaohua Zazhi. 1999;7:249–251. [Google Scholar]
- 13.Qiao Q, Wu JS, Zhang J, Ma QJ, Lai DN. Expression and significance of apoptosis related gene bcl-2, bax in human large intestine adenocarcinoma. Shijie Huaren Xiaohua Zazhi. 1999;7:936–938. [Google Scholar]
- 14.Jiang HY, Qing SH. Research on related factors with lymph node metastasis of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 1999;7:982–984. [Google Scholar]
- 15.Wang Q, Wu JS, Lai DN, Ma QJ, Pan BR. Expression and significance of p16 protein in colorectal carcinoma. Shijie Huaren Xiaohua Zazhi. 1999;7:1047–1048. [Google Scholar]
- 16.Cao JB, Li SR. Relation between human papilloma virus and colorectal cancer. Shijie Huaren Xiaohua Zazhi. 1999;7:1070–1071. [Google Scholar]
- 17.Zhang LL, Zheng ZS, Zhang YL, Wu BP, Guo W, Liu XX, Zhou DY. Microsatellite instability in multiple primary colorectal cancers. Shijie Huaren Xiaohua Zazhi. 1999;7:397–399. [Google Scholar]
- 18.Li M, Wang H, Yu BM, Zheng MH. Effect of p53 gene mutation and tumor markers on the prognosis of patients with colorectal cancer. Shijie Huaren Xiaohua Zazhi. 1999;7:425–426. [Google Scholar]
- 19.Wang SM, Wu JS, Yao X, He ZS, Pan BR. Effect of TGFa, EGFR anti-sense oligodeoxynucleotides on colon cancer cell line. Shijie Huaren Xiaohua Zazhi. 1999;7:522–524. [Google Scholar]
- 20.Li WS, Li JS. Surgical treatment of left colon carcinoma obstruction. Shijie Huaren Xiaohua Zazhi. 1999;7:533–534. [Google Scholar]
- 21.Yao XQ, Qing SH. Detection of multidrug resistance gene in progressive colon cancer and its significance. Shijie Huaren Xiaohua Zazhi. 1999;7:535–536. [Google Scholar]
- 22.Fan YF, Huang ZH. Progress in the studies of gene therapy for colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:427–430. [Google Scholar]
- 23.Wang CH, Zhang XM, Zhan M, Tang FX, Li L. TGF-β and its receptor expression in human colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:462–3. [Google Scholar]
- 24.Fan RY, Li SR, Wu ZT, Wu X. Detection of p53 protein, k-ras and APC gene mutation in sporadic colorectal cancer tissue and exfoliative epithelial cell in stool. Shijie Huaren Xiaohua Zazhi. 2001;9:771–775. [Google Scholar]
- 25.Sheng ZX, Chao G, Sun J. Clinical significance of Cox-2 mRNA expression in colorectal cancer tissue. Shijie Huaren Xiaohua Zazhi. 2001;9:1082–1083. [Google Scholar]
- 26.Yu BM, Zhao R. Molecular biology of colorectal carcinoma. Shijie Huaren Xiaohua Zazhi. 1999;7:173–175. [Google Scholar]
- 27.Deng YC, Zhen YS, Zheng S, Xue YC. Activity of boanmycin against colorectal cancer. World J Gastroenterol. 2001;7:93–97. doi: 10.3748/wjg.v7.i1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bai DJ, Yang GL, Yuan HY, Li Y, Wang K. Effect of cimetidine on T-lymplocyte subsets in periopenative gastrointestinal cancer patients. Shijie Huaren Xiaohua Zazhi. 2000;8:147–149. [Google Scholar]
- 29.Yang JH, Rao BQ, Wang Y, Tu XH, Zhang LY, Chen SH, Ou-Yong XN, Dai XH. Clinical significance of defecting the circulating cancer cells in peripheral blood from colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:187–189. [Google Scholar]
- 30.Li SR. Early diagnosis of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:780–782. [Google Scholar]
- 31.Sheng JQ, Chen ZM. Colorectal cancer related gene in the screen of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:783–785. [Google Scholar]
- 32.Gu F, Lu YM. Treatment of colorectal adenoma. Shijie Huaren Xiaohua Zazhi. 2001;9:785–786. [Google Scholar]
- 33.Han RY. Early endoscopic diagnosis of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:789–790. [Google Scholar]
- 34.Han YY. Endoscopic treatment of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:790–792. [Google Scholar]
- 35.Wang YB, Yang ZX. Routine diagnosis of colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:792–793. [Google Scholar]
- 36.Ma Q, Zhang ZS, Wang QY. Reverse of multidrug resistance to colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:822–825. [Google Scholar]
- 37.Gu HP, Ni CR, Zhan RZ. Relationship of expression of CD15, CD44V6 and nm23H1 mRNA with metastasis and prognosis of colon carcinoma. Shijie Huaren Xiaohua Zazhi. 2000;8:887–891. [Google Scholar]
- 38.Zha R, Yu BM, Zhang GC, Zheng MH, Li DH, Huang L, Zhou HZ. Effect of selenium on immunity and anti-oxidative functions in patients with colorectal carcinoma. Shijie Huaren Xiaohua Zazhi. 2000;8:1013–1016. [Google Scholar]
- 39.Jia L, Chen TX, Sun JW, Na ZM, Zhang HH. Relationship between microvessel density and proliferating cell nuclear antigen and prognosis in colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:74–76. [Google Scholar]
- 40.Ji DJ, Cao Y, Zhang YL, Jiang B, Yu N, Feng FC, Zhou DY. Synchronous studies on variation of p53 gene transcriptions and expression in HT-29, Lovo cells. Shijie Huaren Xiaohua Zazhi. 2000;8:77–79. [Google Scholar]
- 41.Zhao R, Zhang GC, Yu BM, Zheng MH, Li DH, Zhu YM, Hu BY. Effect of selemicm on T lymphocytc against colonic cancer cells. Shijie Huaren Xiaohua Zazhi. 2000;8:80–83. [Google Scholar]
- 42.Cao JB, Li SR, Zhu QP, Gu SY, Li YJ, Chen ZM, Zhang HG. The study of relationship between human papillomaviras and colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:111–112. [Google Scholar]
- 43.Chen J, Gu GG, Ling WH, Luo YH. Microsatellite instability in 46 cases with non-hereditary colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2000;8:350–352. [Google Scholar]
- 44.Wang ZW, Cheng RX, Zhou GJ, Shen HD, Chon YQ. CK20 mRNA expression in the peripheral blood of colorectal cancer patients. Shijie Huaren Xiaohua Zazhi. 2000;8:818–820. [Google Scholar]
- 45.Maehara Y, Kakeji Y, Kabashima A, Emi Y, Watanabe A, Akazawa K, Baba H, Kohnoe S, Sugimachi K. Role of transforming growth factor-beta 1 in invasion and metastasis in gastric carcinoma. J Clin Oncol. 1999;17:607–614. doi: 10.1200/JCO.1999.17.2.607. [DOI] [PubMed] [Google Scholar]
- 46.Rodeck U, Nishiyama T, Mauviel A. Independent regulation of growth and SMAD-mediated transcription by transforming growth factor beta in human melanoma cells. Cancer Res. 1999;59:547–550. [PubMed] [Google Scholar]
- 47.Sheen-Chen SM, Chen HS, Sheen CW, Eng HL, Chen WJ. Serum levels of transforming growth factor beta1 in patients with breast cancer. Arch Surg. 2001;136:937–940. doi: 10.1001/archsurg.136.8.937. [DOI] [PubMed] [Google Scholar]
- 48.Farina AR, Coppa A, Tiberio A, Tacconelli A, Turco A, Colletta G, Gulino A, Mackay AR. Transforming growth factor-beta1 enhances the invasiveness of human MDA-MB-231 breast cancer cells by up-regulating urokinase activity. Int J Cancer. 1998;75:721–730. doi: 10.1002/(sici)1097-0215(19980302)75:5<721::aid-ijc10>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 49.Shim KS, Kim KH, Han WS, Park EB. Elevated serum levels of transforming growth factor-beta1 in patients with colorectal carcinoma: its association with tumor progression and its significant decrease after curative surgical resection. Cancer. 1999;85:554–561. doi: 10.1002/(sici)1097-0142(19990201)85:3<554::aid-cncr6>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 50.Xiong B, Gong LL, Zhang F, Hu MB, Yuan HY. TGF beta1 expression and angiogenesis in colorectal cancer tissue. World J Gastroenterol. 2002;8:496–498. doi: 10.3748/wjg.v8.i3.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xiong B, Yuan HY, Hu WB, Ydan T, Yang GD. Serum levels of transforming growth factor-β1 correlating with T cell subsets and natural killer cell activity in colorectal cancer. Shijie Huaren Xiaohua Zazhi. 2001;9:1194–1195. [Google Scholar]


