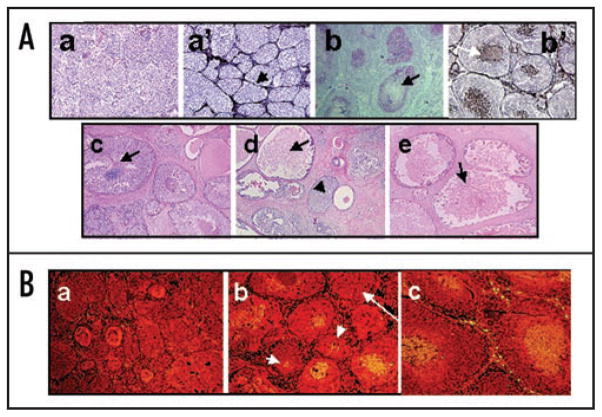
Figure 1.
(A) Comparative morphologies of clinical comedo-DCIS (c–e) and MCF10DCIS.com xenografts (a, a′, b, b′). Panels (a and b), H&E of MCF10DCIS.com xenografts at days 20 and 44, respectively. Panels (a′ and b′), silver staining of MCF10DCIS.com xenografts at days 20 and 44, respectively. Panels (c–e), H&E of clinical comedo-DCIS breast tumors. Note that MCF10DCIS.com xenografts initially organize into solid DCIS lesions surrounded by basement membrane (arrow in a′) before conversion to comedo-DCIS. Arrows in (b, b′ and c–e), indicate necrotic cores and the arrowhead in (d), solid DCIS. Original magnification x10. (B) MCF10DCIS.com xenografts undergo spontaneous apoptosis. Panels (a–c), TUNEL staining for xenografts harvested at days 20, 30 and 44 days, respectively. Note the presence of central TUNEL-positive cells in (b and c) and its absence in (a). Also, note that TUNEL positivity is not related to the size of the ducts as some small ducts are TUNEL positive (short arrows in b), whereas some larger ducts (long arrow in b) are TUNEL-negative. Original magnification x10.