Abstract
Both single-bundle (SB) and double-bundle (DB) procedures have been widely used in the treatment of anterior cruciate ligament (ACL) rupture; however, the optimal repair strategy remains considerably controversial. In this meta-analysis of published studies, we compared the results of these two techniques. After systematic review of electronic databases and websites, a total of 8 RCTs reporting data on 941 subjects were included. The objective and subjective functional recovery outcomes were meta-analyzed. The methodological quality was evaluated using the CBRG scale. The overall pooled data showed superiority in rotational stability, the degree of osteoarthritis (OA) changes, and subjective function score postoperatively in patients managed with DB compared with the SB procedure (pivot shift test, P = 0.02; degree of OA, P = 0.02; Lysholm score, P = 0.04; and Tegner scale, P = 0.002, respectively). However, subgroup analysis suggested no difference between the treatment procedures at long-term follow-up. This meta-analysis demonstrated that the DB technique could result in better rotational stability and higher subjective function score and was effective in preventing OA compared to SB in the mid-term treatment of the injured ACL. Further studies with better design involving larger sample sizes and longer-term follow-up are required.
Keywords: Single-bundle, double-bundle, anterior cruciate ligament, mid- to long-term, meta-analysis
Introduction
Anterior cruciate ligament (ACL) injury is the most common type of sports injury to the knee and may result in recurrent knee instability, meniscal tears, and articular cartilage degeneration [1-3]. Currently, the most common treatment strategy for the injured ACL is either single-bundle (SB) or double-bundle (DB) ACL reconstruction [4,5]. Both surgical management approaches are relatively effective in restoring the native anatomy and kinematics of the joint [2].
The arthroscopic SB technique has been widely performed by creating one single femoral tunnel and one single tibial tunnel for decades [6-8]. Whereas this technique may provide good clinical outcomes and restore anterior stability following an ACL injury [9], it may be suboptimal with regard to rotational function and may even cause osteoarthritis (OA) postoperatively [10,11]. Previous studies have revealed that the ACL is a double-bundled ligament containing the anteromedial (AM) bundle and the posterolateral (PL) bundle, which possess different functions [12,13]. The arthroscopic DB strategy, first described by Mott in 1983 [14], technically reconstructs the 2 functional bundles of the ACL, thereby more closely approximating the native anatomy. Moreover, it improves pivot shift resistance and increases rotational knee control [15-18] in comparison to SB ACL reconstruction.
An increasing number of studies have been performed comparing the two surgical techniques, that is, SB versus DB procedures. Many biomechanical studies comparing the two procedures on human cadavers have demonstrated better results for DB ACL reconstruction [10,12]. Several clinical studies have reported that anatomic DB ACL reconstruction might improve pivot-shift resistance, increase rotational knee control, decrease the rate of meniscal tears, and postpone progression toward arthritis [1,19-21]. However, other studies found no significant differences between clinical outcomes in the patient groups [22-24]. Moreover, different results were reported among several previously published meta-analyses [2,6,7]. The optimal treatment for ACL rupture therefore remains controversial.
Although there have been several meta-analysis reviews comparing the two procedures, it remains unclear which one is superior and moreover, few randomized controlled trials (RCTs) with a minimum of 3-year follow-up were included in those studies. Hence, the purpose of this meta-analysis is to evaluate the mid- to long-term results of SB versus DB ACL reconstruction by pooling the results of RCTs.
Materials and methods
Eligibility criteria
Only the RCTs comparing SB versus DB arthroscopic ACL reconstruction were included in this review. Quasi-randomized studies (nonrandom treatment allocation) were excluded. Studies were considered to be eligible if they met the following criteria: 1) all-arthroscopic ACL reconstruction using either the SB or the DB repair, or both, 2) only therapeutic studies, 3) a minimum of 3-year follow-up, 4) one or more outcomes of interest postoperatively, and 5) only prospective RCT study design. The exclusion criteria were the following: 1) non-English-language articles, 2) technique papers, 3) studies that compared the two techniques on patients using an open technique and on cadavers, 4) articles that did not describe the surgical techniques used, and 5) all studies that were not RCTs. When more than one study by the same author was included in this review, the reported data were carefully assessed by comparing the demographic data. When the necessary data provided in the included study were incomplete, the data were obtained by contacting the author. All studies considered eligible were finally included based on the full article.
Search strategies
We searched for the results of relevant trials published from January 1991 to October 2014 in the Cochrane Library, EMBASE, and PubMed. The following search terms were used: “anterior cruciate ligament”, “ACL”, “single-bundle”, “double-bundle”, “SB”, and “DB”, with various combinations of the operators “AND” and “OR”. The study language was restricted to English. Reduplication was eliminated during the search process. The study was analyzed in full text if the potential data provided in the titles and abstracts did not establish whether the studies contained relevant information. References cited in the articles and relevant review articles were assessed to search for additional studies. Two authors independently reviewed the articles to identify articles that potentially met the eligibility criteria. Any disagreement between the reviewers was resolved by discussion with another reviewer.
Outcome measures
A variety of outcome scores were acknowledged in this review. The objective results used as the primary outcomes were the pivot shift test, anteroposterior laxity, the objective International Knee
Documentation Committee (IKDC) score, and arthritic changes. According to the IKDC criteria [25], the pivot-shift test, objective IKDC score, and the degree of arthritic changes were classified as normal, nearly normal, abnormal and severely abnormal. We only recorded the number of subjects with a normal pivot-shift test for the meta-analysis. The anteroposterior laxity was assessed with an arthrometer. The secondary outcomes included subjective data, such as the subjective IKDC scale, the Lysholm score, and the Tegner scale.
Data extraction and management
The data were extracted by two independent reviewers and further discussed with another independent senior author. The extracted information included the following: 1) the characteristics of the included studies, including the authors, study design, year of publication, sample size, age, gender, duration of follow-up, and time from injury to surgery; 2) the surgical details, such as the type of graft, drilling technique, and patterns of fixation; and 3) the outcomes details. In cases of discrepancies, the two reviewers reached a consensus by discussion and the senior author eventually determined the conclusion. This formed the basis of the results for the data analysis.
Risk of bias assessment
The methodological quality of each included study was assessed by the two reviewers using the Cochrane Back Review Group (CBRG) scale [26]. For each criterion, “yes” or “no” was recorded. Studies with a quality score of > 6 points were considered to have a low risk of bias and studies scoring > 9 on the CBRG scale were designated as high-quality randomized controlled trials. To minimize the selection bias, two investigators evaluated the studies independently and subsequently determined a score based on the scale.
Statistical analysis
All statistical analyses were performed using Review Manager 5.2. Statistical heterogeneity was assessed using the chi-squared and I 2 tests. For each study, we calculated risk ratios (RRs) with 95% confidence intervals (CIs) for dichotomous data and standard mean differences (SMDs) with 95% CIs for continuous data. A fixed-effects model was initially employed in the analysis and alternatively, a random-effects model was used if significant heterogeneity was observed across the studies (I 2 > 50%). A P value lower than 0.05 was considered statistically significant. The lack of publication bias in this review was due to the small number of studies (< 10) included in each analysis.
Results
Search results
The primary search generated 12 031 potentially relevant articles of which 8 studies [1,3,27-32] with a total of 941 subjects met the selection criteria. The flow diagram of the study search process is presented in Figure 1. The characteristics of the included studies are listed in Table 1. Surgery-related information in the 8 publications included in this review is provided in Table 2. The detailed results regarding the methodological quality of each included study are summarized in Table 3. Ultimately, all of the included RCTs scored at least 8 points on the CBRG scale.
Figure 1.
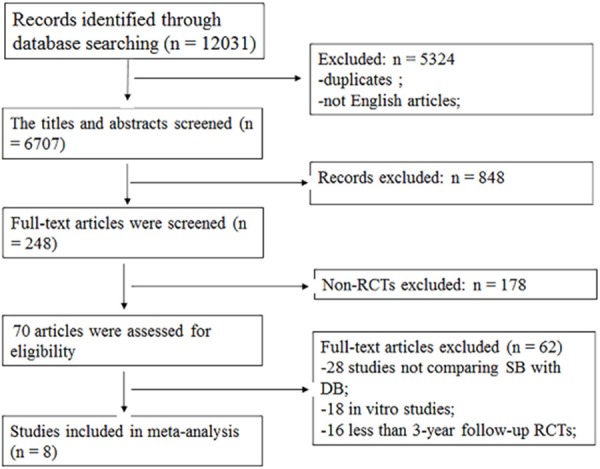
Flow diagram of study selection.
Table 1.
Demographic characteristics of included studies
| Author | Year | Country | Design | Sample size | Age (mean, y) | Gender (M/F) | FITST (mean, mo) | Side involved (L/R) | Follow-up (mean, mo) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||
| SB | DB | SB | DB | SB | DB | SB | DB | SB | DB | |||||
| Zaffagnini; [27] | 2007 | Italy | L-1 RCT | 35 | 37 | 26 | 27 | 20/15 | 20/17 | 8.2 | 6.9 | N/A | N/A | 36 |
| Zaffagnini; [28] | 2010 | Italy | L-2 RCT | 39 | 40 | 26 | 27 | 20/19 | 22/18 | 8.6 | 8.9 | N/A | N/A | 103 |
| Gobbi; [29] | 2011 | Italy | L-1 RCT | 30 | 30 | 31.9 | 28.9 | 15/15 | 18/12 | N/A | N/A | 18/12 | 12/18 | 46.2 |
| Hussein; [1] | 2011 | Slovenia | L-1 RCT | 78 | 131 | 34.2 | 32.3 | 46/32 | 80/51 | N/A | N/A | 46/32 | 68/63 | 51.15 |
| Suomalainen; [30] | 2012 | Finland | L-1 RCT | 30 | 30 | 30 | 34 | 21/9 | 21/9 | 12 | 13 | N/A | N/A | 60 |
| Song; [31] | 2013 | Korea | L-2 RCT | 60 | 52 | 35.5 | 30.3 | 38/22 | 44/8 | 7.6 | 8.3 | N/A | N/A | 48 |
| Sun; [3] | 2014 | China | L-1 RCT | 142 | 154 | 28.2 | 27.5 | 101/41 | 106/48 | N/A | N/A | N/A | N/A | 36 |
| Koga; [32] | 2014 | Japan | L-2 RCT | 25 | 28 | 24 | 25 | 7/18 | 16/12 | 16 | 18 | N/A | N/A | 69 |
Abbreviations: L, Level; RCT, Randomized controlled trial; SB, Single bundle; DB, Double bundle; FITST, from injury to surgery time; N/A, not applicable.
Table 2.
Surgery-Related Information and Evaluation Data from the Studies Involved
| Author | Graft | Drilling | Fixation | Evaluation Index | |
|---|---|---|---|---|---|
|
|
|||||
| SB | DB | ||||
| Zaffagnini; [27] | STG | TMP | Staple/with a TSK/looped around BB | IKDC scores, Tegner scale, KT-2000 measurements, Activity Rating Scale, Thigh girth, Psychovitality Questionnaire, Ahlback radiographic score | |
| Zaffagnini; [28] | BPTB | STG | TAMP/TMP | IS/TSK/ looped around BB | IKDC scores, Tegner scale, KT-2000 measurements, pivot shift test |
| Gobbi; [29] | ST | TAMP+OIT | EndoButton+bioabsorbable IS | Rolimeter, pivot shift test, IKDC scores, Noyes score, Lysholm scores, Marx scores, Tegner scale, ROM, Psychological profile | |
| Hussein; [1] | STG | TMP/TT | SF+bioabsorbable IS | Pivot shift test, KT-1000 measurements, IKDC scores, Lysholm scores | |
| Suomalainen; [30] | STG | ST | TAMP+OIT | bioabsorbable IS | Pivot-shift test, KT-1000, IKDC, Lysholm, Degree of OA |
| Song; [31] | TA | TAMP | bioabsorbable IS | Degree of OA, Lysholm, Tegner score, IKDC, Lachman test, Pivot-shift test | |
| Sun; [3] | TA | STG/TA | TAMP/TT | bioabsorbable IS+Retro Button | KT-1000, Pivot shift test, IKDC, Lysholm scores, Degree of OA |
| Koga; [32] | ST | TAMP | EndoButton+nonabsorbable anchor | KT-1000, Pivot-shift test, Lachman test, Anterior drawer test, Lysholm score, patient satisfaction, Tegner score, Sports performance level | |
Abbreviations: SB, single bundle; DB, double bundle; STG, semitendinosus and gracilis graft; ST, semitendinosus tendon graft; BPTB, bone patellar tendon bone graft; TA, tibialis anterior; TMP, through medial portal; TAMP, through anteromedial portal; OIT, outside-in technique; TT, transtibial tunnel; TSK, transtibial tunnel; BB, bony bridge; IS, interference screws; SF, suspensory fixation; IKDC, International Knee Documentation Committee; ROM, range of motion; OA, osteoarthritis.
Table 3.
Risk of bias assessment of the RCTs
| Zaffagnini [27] | Zaffagnini [28] | Gobbi [29] | Hussein [1] | Suomalainen [30] | Song [31] | Sun [3] | Koga [32] | |
|---|---|---|---|---|---|---|---|---|
| Adequate randomization | Y | Y | Y | Y | Y | Y | Y | Y |
| Allocation concealment | Y | Y | Y | Y | Y | Y | Y | Y |
| Blinding of patients | N | N | Y | N | N | N | N | Y |
| Blinding of care providers | N | N | N | N | N | N | N | N |
| Blinding of outcome assessors | Y | Y | Y | Y | Y | Y | Y | Y |
| Baseline comparability | Y | Y | Y | Y | Y | Y | Y | Y |
| Drop-out rate is described | Y | Y | Y | Y | N | N | Y | Y |
| Free of selective outcome reporting | Y | Y | Y | Y | Y | Y | Y | Y |
| Co-interventions were similar | Y | Y | Y | Y | Y | Y | Y | Y |
| Acceptable compliance between groups | Y | Y | Y | Y | Y | Y | Y | Y |
| Intention-to treatment analysis | N | N | N | N | N | N | N | N |
| Similar timing of outcome assessment | Y | Y | Y | Y | Y | Y | Y | Y |
| Overall quality (max 12) | 9 | 9 | 10 | 9 | 8 | 8 | 9 | 10 |
Abbreviations: Y, yes; N, no.
Primary outcomes
With a minimum of 3-year follow-up, all 8 studies used the pivot shift test to assess knee laxity. More patients with normal test results were observed in the DB group (RR = 0.84, 95% CI = 0.73 to 0.97; P = 0.02), compared to the SB group with moderate heterogeneity (I 2 = 73%; Figure 2A). All of the included studies reported anteroposterior laxity, representing another assessment of knee laxity. However, because one study [3] did not provide the standard deviation, the meta-analysis could only be performed with seven studies. There was no significant difference in anteroposterior laxity between the SB and the DB groups (SMD = 0.16, 95% CI = 0.00 to 0.32; P = 0.05) with moderate heterogeneity (I 2 = 72%; Figure 2B). Data on the objective IKDC score were available in five RCTs and after meta-analysis, no significant difference was observed (P = 0.12; Figure 2C), without significant heterogeneity. With respect to the incidence of OA, the analyzed results suggested a significant difference between the two procedures (RR = 0.85, 95% CI = 0.75 to 0.97; P = 0.02) without significant heterogeneity across the studies (I 2 = 0; Figure 2D).
Figure 2.
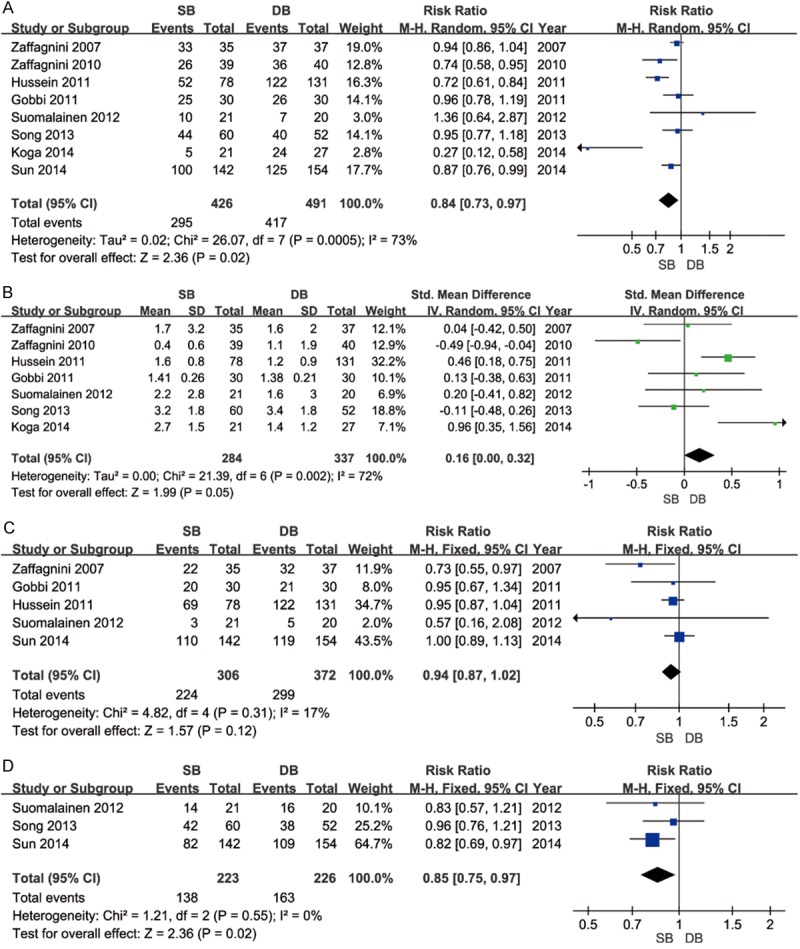
Primary outcomes after meta-analysis. A. Forest plot to assess pivot shift test between two treatment strategies; B. Forest plot to assess anteroposterior laxity between two treatment strategies; C. Forest plot to assess obective IKDC scores between two treatment strategies; D. Forest plot to assess arthritic changes between two treatment strategies.
Secondary outcomes
The secondary outcomes were evaluated using 3 indices: the subjective IKDC score, the Lysholm score, and the Tegner scale. Figure 3 shows the detailed results of the pooled analysis. With respect to the subjective IKDC score, the analysis using a random effects model did not reveal a significant difference between the two strategies (P = 0.09; Figure 3A). Six studies reported final follow-up Lysholm scores and one report was excluded for lacking standard deviation. With a fixed effects model, there was a significant difference between the two groups (SMD = -0.17, 95% CI = -0.32 to -0.01; P = 0.04). Heterogeneity across the studies was not considered significant (I 2 = 16%; Figure 3B). After combining the data from three RCTs, a significantly higher Tegner score was observed in the DB group compared to patients who received SB ACL reconstruction (SMD = -0.76, 95% CI = -1.25 to -0.27; P = 0.002; Figure 3C).
Figure 3.
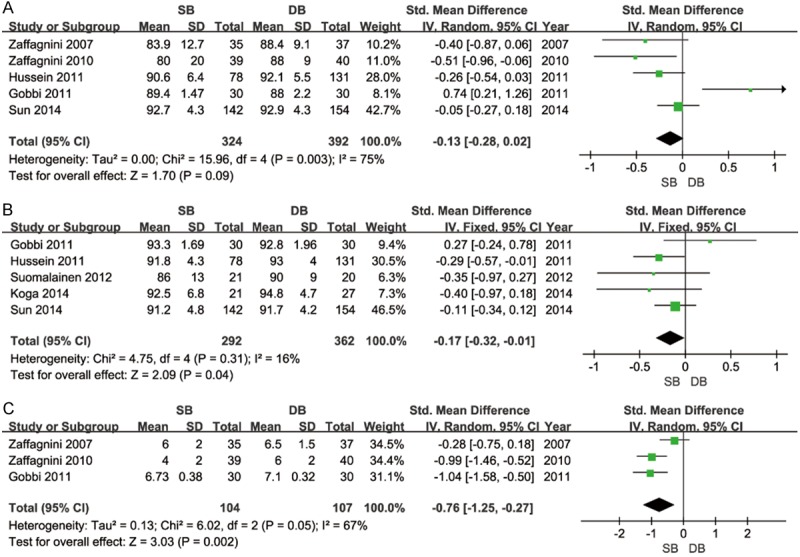
Secondary outcomes after meta-analysis. A. Forest plot to assess subjective IKDC scores between two treatment strategies; B. Forest plot to assess Lysholm Score between two treatment strategies; C. Forest plot to assess Tegner Scale between two treatment strategies.
Subgroup and sensitivity analysis
Subgroup analysis according to the period of follow-up was available for knee stability (pivot shift test). The period of follow-up was divided into two groups (less than 5 years and more than 5 years). More stable knees were observed in patients who underwent double-bundle procedures at less than 5 years of follow-up (Figure 4A) but no significant difference was found between the two groups at longer-term follow-up (≥ 5 years) (Figure 4B). A series of sensitivity analyses (Table 4) was conducted by omitting one of the eligible studies at a time. The results revealed that there was not a particularly influential study among all of the selected studies, except for the impact of the trial of Suomalainen et al. [30] on the Lysholm scores. No significant difference was observed in the Lysholm scores between the two treatment groups after the exclusion of the Suomalainen et al. trial.
Figure 4.
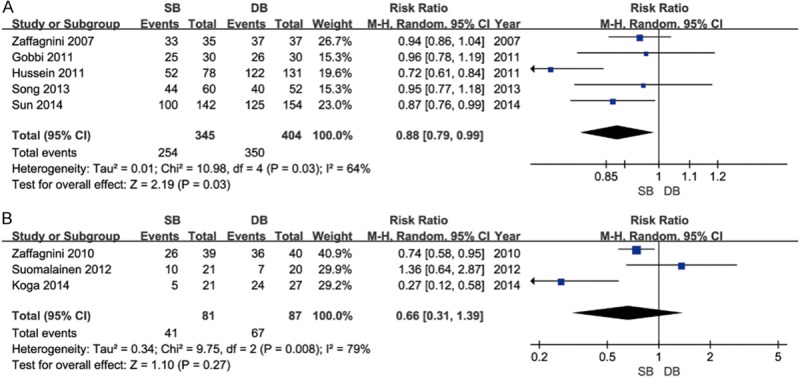
Subgroup analysis according to the period of follow-up. A. Difference in the pivot shift test at mid-term follow-up (< 5 years). B. Difference in the pivot shift test at long-term follow-up (≥ 5 years).
Table 4.
Sensitivity analysis was conducted by only pooling data from the studies that score > 9 points on the CBRG scale
| Outcomes | RRE/SMD (95% CI) | I 2 | P value |
|---|---|---|---|
| Pivot shift test | 0.80 [0.68, 0.96] | 82% | 0.01* |
| Anteroposterior laxity | 0.20 [-0.23, 0.63] | 79% | 0.35 |
| Objective IKDC scores | 0.95 [0.88, 1.02] | 28% | 0.16 |
| Arthritic changes | 0.82 [0.69, 0.97] | N/A | 0.02* |
| Subjective IKDC scores | -0.12 [-0.44, 0.21] | 75% | 0.48 |
| Lysholm Scores | -0.15 [-0.31, 0.01] | 32% | 0.06* |
| Tegner Scale | -0.76 [-1.25, -0.27] | 67% | 0.002* |
Abbreviations: RRE, risk ratio effect; SMD, standard mean difference; N/A, not applicable.
sigificant difference.
Discussion
Currently, ACL reconstruction is frequently used to recreate native anatomy, to better replicate natural ACL function, and to prevent future degenerative changes [2,7] because the ACL plays an important role in the motion of the knee and in restricting anterior tibial dislocation [7]. The SB procedure is widely accepted as the standard surgical option to treat ACL-deficient knees [33]. The SB ACL reconstruction is successful in restoring anterior stability and provides good clinical outcomes postoperatively [31]. However, many studies have reported frequent complications of rotational instability and an increased incidence of OA with the SB technique [34-37]. With surgical technologic development, advances in ACL reconstructive techniques have concentrated on reducing these complications [38-40]. Therefore, many surgeons have considered DB ACL reconstruction an attractive option.
Several biomechanical studies have concluded that DB ACL reconstruction is superior to the SB technique in anterior and rotational stability of the knee and that it more closely restores the knee anatomy [38,41,42]. Furthermore, previous studies comparing the clinical results of SB versus DB techniques have reported on the superiority of the latter [28,39,43]. Conversely, some studies have reported no difference between the two procedures [44,45]. Additionally, the follow-ups in most of the published trials were less than 3 years, a period that is too brief to observe the natural history of the injured ACL repair and the propensity for developing OA changes in the knees postoperatively [30]. This may be a reason for the debate above. Consequently, we conducted the present meta-analysis to investigate the mid- to long-term clinical outcomes of the two techniques.
The most important findings of this study was that a significant difference was observed between the two techniques with regard to the pivot shift test, although no significant difference was observed among patients treated with single- or double-bundle ACL reconstruction at longer-term follow-up. However, according to the final results, a tendency persisted for patients who underwent the DB procedure to acquire better rotational stability of the knee postoperatively compared to those patients who underwent SB ACL reconstruction. Similar results was presented in a recent meta-analysis by Desai et al. [2]. However, their study reported DB as superior to SB in terms of anteroposterior laxity. In another meta-analysis by Xu et al. [6], better anterior stability and higher objective IKDC scores were shown in the DB group. Inconsistent results appeared in our review, that is, we found no significant difference between the two groups with regard to the objective IKDC score and anteroposterior laxity.
Injury of the ACL often results in the subsequent progression of knee OA changes [46-48]. Nevertheless, whether an increasing incidence of OA occurred after arthroscopic SB surgery was not analyzed in many previous meta-analyses. After a meta-analysis of the degree of OA, we found that the arthroscopic DB procedure could postpone the development of OA changes in the ACL-deficient knees. This suggested a relatively higher risk of OA in long-term follow-up after SB ACL reconstruction surgery. However, these findings should be interpreted with caution because only three included studies with a total of 449 patients reported this index.
With respect to the subjective IKDC score, no significant difference was shown between the two groups, although this meta-analysis demonstrated significant differences regarding the Lysholm score and the Tegner scale, (P = 0.04 and P = 0.002, respectively). The results of Muneta et al. [9] also suggested that a higher Lysholm knee scale was obtained in the DB group, whereas Sastre et al. [49] reported no significant difference in the Lysholm score between the two techniques. Although we did detect superior knee stability after DB ACL reconstruction compared to the SB procedure, the enduring controversy regarding the subjective scores suggested that patient satisfaction is not exclusively dependent on postoperative knee stability [50].
There were several limitations in this review. First, the English-language restriction of the included studies may have contributed to a publication bias factor. Second, all of the RCTs were performed at a single center. Multicenter studies with more patients will be required in the future. Finally, a significant need remains for a gold standard outcome to evaluate the postoperative clinical effects following arthroscopic SB and DB ACL surgery.
Conclusions
Based on this first meta-analysis of mid- to long-term results, the following conclusions may be drawn: the DB ACL reconstruction effectively enhances rotational stability of the knee joint and achieves higher subjective functional scores at the mid-term follow-up compared with the SB procedure. However, at long-term follow-up, the results regarding knee joint stability must be interpreted with caution. In the future, better-designed RCTs with improved evaluation methods involving multiple centers, longer-term follow-up and larger sample sizes are desirable.
Disclosure of conflict of interest
None.
References
- 1.Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic doublebundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40:512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 2.Desai N, Bjornsson H, Musahl V, Bhandari M, Petzold M, Fu FH, Samuelsson K. Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:1009–1023. doi: 10.1007/s00167-013-2811-6. [DOI] [PubMed] [Google Scholar]
- 3.Sun R, Chen BC, Wang F, Wang XF, Chen JQ. Prospective randomized comparison of knee stability and joint degeneration for double-and single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23:1171–8. doi: 10.1007/s00167-014-2934-4. [DOI] [PubMed] [Google Scholar]
- 4.Zelle BA, Brucker PU, Feng MT, Fu FH. Anatomical double-bundle anterior cruciate ligament reconstruction. Sports Med. 2006;36:99–108. doi: 10.2165/00007256-200636020-00001. [DOI] [PubMed] [Google Scholar]
- 5.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35:223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 6.Xu M, Gao S, Zeng C, Han R, Sun J, Li H, Xiong Y, Lei G. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29:357–365. doi: 10.1016/j.arthro.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 7.Li X, Xu CP, Song JQ, Jiang N, Yu B. Singlebundle versus double-bundle anterior cruciate ligament reconstruction: an up-to-date metaanalysis. Int Orthop. 2013;37:213–226. doi: 10.1007/s00264-012-1651-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 9.Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and doublebundle techniques. Arthroscopy. 2007;23:618–628. doi: 10.1016/j.arthro.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 11.Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon . A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84-A:907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Mae T, Shino K, Miyama T, Shinjo H, Ochi T, Yoshikawa H, Fujie H. Single- versus twofemoral socket anterior cruciate ligament reconstruction technique: Biomechanical analysis using a robotic simulator. Arthroscopy. 2001;17:708–716. doi: 10.1053/jars.2001.25250. [DOI] [PubMed] [Google Scholar]
- 13.Radford WJ, Amis AA. Biomechanics of a double prosthetic ligament in the anterior cruciate deficient knee. J Bone Joint Surg Br. 1990;72:1038–1043. doi: 10.1302/0301-620X.72B6.2147184. [DOI] [PubMed] [Google Scholar]
- 14.Mott HW. Semitendinosus anatomic reconstruction for cruciate ligament insufficiency. Clin Orthop Relat Res. 1983:90–92. [PubMed] [Google Scholar]
- 15.Fu FH, Karlsson J. A long journey to be anatomic. Knee Surg Sports Traumatol Arthrosc. 2010;18:1151–1153. doi: 10.1007/s00167-010-1222-1. [DOI] [PubMed] [Google Scholar]
- 16.Shen W, Jordan S, Fu F. Review article: anatomic double bundle anterior cruciate ligament reconstruction. J Orthop Surg (Hong Kong) 2007;15:216–221. doi: 10.1177/230949900701500219. [DOI] [PubMed] [Google Scholar]
- 17.van Eck CF, Lesniak BP, Schreiber VM, Fu FH. Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy. 2010;26:258–268. doi: 10.1016/j.arthro.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 18.van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy. 2010;26:S2–12. doi: 10.1016/j.arthro.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Lee S, Kim H, Jang J, Seong SC, Lee MC. Comparison of anterior and rotatory laxity using navigation between single- and doublebundle ACL reconstruction: prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2012;20:752–761. doi: 10.1007/s00167-012-1880-2. [DOI] [PubMed] [Google Scholar]
- 20.van Eck CF, Kopf S, Irrgang JJ, Blankevoort L, Bhandari M, Fu FH, Poolman RW. Singlebundle versus double-bundle reconstruction for anterior cruciate ligament rupture: a metaanalysis--does anatomy matter? Arthroscopy. 2012;28:405–424. doi: 10.1016/j.arthro.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 21.Xu Y, Ao YF, Wang JQ, Cui GQ. Prospective randomized comparison of anatomic singleand double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:308–316. doi: 10.1007/s00167-013-2398-y. [DOI] [PubMed] [Google Scholar]
- 22.Park SJ, Jung YB, Jung HJ, Jung HJ, Shin HK, Kim E, Song KS, Kim GS, Cheon HY, Kim S. Outcome of arthroscopic single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a preliminary 2-year prospective study. Arthroscopy. 2010;26:630–636. doi: 10.1016/j.arthro.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Kanaya A, Ochi M, Deie M, Adachi N, Nishimori M, Nakamae A. Intraoperative evaluation of anteroposterior and rotational stabilities in anterior cruciate ligament reconstruction: lower femoral tunnel placed single-bundle versus double-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:907–913. doi: 10.1007/s00167-009-0757-5. [DOI] [PubMed] [Google Scholar]
- 24.Wang JQ, Ao YF, Yu CL, Liu P, Xu Y, Chen LX. Clinical evaluation of double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: a prospective, randomized and controlled study. Chin Med J (Engl) 2009;122:706–711. [PubMed] [Google Scholar]
- 25.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 26.Furlan AD, Pennick V, Bombardier C, van Tulder M Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 27.Zaffagnini S, Bruni D, Russo A, Takazawa Y, Lo Presti M, Giordano G, Marcacci M. ST/G ACL reconstruction: double strand plus extraarticular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports. 2008;18:573–581. doi: 10.1111/j.1600-0838.2007.00697.x. [DOI] [PubMed] [Google Scholar]
- 28.Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19:390–397. doi: 10.1007/s00167-010-1225-y. [DOI] [PubMed] [Google Scholar]
- 29.Gobbi A, Mahajan V, Karnatzikos G, Nakamura N. Single- versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clin Orthop Relat Res. 2012;470:824–834. doi: 10.1007/s11999-011-1940-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suomalainen P, Jarvela T, Paakkala A, Kannus P, Jarvinen M. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med. 2012;40:1511–1518. doi: 10.1177/0363546512448177. [DOI] [PubMed] [Google Scholar]
- 31.Song EK, Seon JK, Yim JH, Woo SH, Seo HY, Lee KB. Progression of osteoarthritis after double- and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:2340–2346. doi: 10.1177/0363546513498998. [DOI] [PubMed] [Google Scholar]
- 32.Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M, Nakamura T, Otabe K, Sekiya I. Mid- to Long-term Results of Single-Bundle Versus Double-Bundle Anterior Cruciate Ligament Reconstruction: Randomized Controlled Trial. Arthroscopy. 2015;31:69–76. doi: 10.1016/j.arthro.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 33.Harner CD, Fu FH, Irrgang JJ, Vogrin TM. Anterior and posterior cruciate ligament reconstruction in the new millennium: a global perspective. Knee Surg Sports Traumatol Arthrosc. 2001;9:330–336. doi: 10.1007/s001670100230. [DOI] [PubMed] [Google Scholar]
- 34.Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC. Long-term results of anterior cruciate ligament reconstruction using bone-patellar tendonbone: an analysis of the factors affecting the development of osteoarthritis. Arthroscopy. 2012;28:1114–1123. doi: 10.1016/j.arthro.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 35.Lee MC, Seong SC, Lee S, Chang CB, Park YK, Jo H, Kim CH. Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy. 2007;23:771–778. doi: 10.1016/j.arthro.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 36.Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 37.Oiestad BE, Holm I, Engebretsen L, Aune AK, Gunderson R, Risberg MA. The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:942–949. doi: 10.1007/s00167-012-2161-9. [DOI] [PubMed] [Google Scholar]
- 38.Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 39.Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, Hoshino Y, Matsushita T, Matsumoto T, Nagamune K, Kurosaka M. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. 2011;35:439–446. doi: 10.1007/s00264-010-1110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kato Y, Ingham SJ, Linde-Rosen M, Smolinski P, Horaguchi T, Fu FH. Biomechanics of the porcine triple bundle anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:20–25. doi: 10.1007/s00167-009-0893-y. [DOI] [PubMed] [Google Scholar]
- 41.Sasaki SU, Mota e Albuquerque RF, Pereira CA, Gouveia GS, Vilela JC, Alcaras Fde L. An in vitro biomechanical comparison of anterior cruciate ligament reconstruction: single bundle versus anatomical double bundle techniques. Clinics (Sao Paulo) 2008;63:71–76. doi: 10.1590/s1807-59322008000100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seon JK, Gadikota HR, Wu JL, Sutton K, Gill TJ, Li G. Comparison of single- and doublebundle anterior cruciate ligament reconstructions in restoration of knee kinematics and anterior cruciate ligament forces. Am J Sports Med. 2010;38:1359–1367. doi: 10.1177/0363546510361494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N. Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med. 2010;38:25–34. doi: 10.1177/0363546509347096. [DOI] [PubMed] [Google Scholar]
- 44.Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y. Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br. 2004;86:515–520. [PubMed] [Google Scholar]
- 45.Streich NA, Friedrich K, Gotterbarm T, Schmitt H. Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc. 2008;16:232–238. doi: 10.1007/s00167-007-0480-z. [DOI] [PubMed] [Google Scholar]
- 46.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 47.Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16:239–244. doi: 10.1016/j.knee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 48.Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M. Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury--a prospective cohort study. Osteoarthritis Cartilage. 2009;17:284–290. doi: 10.1016/j.joca.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 49.Sastre S, Popescu D, Nunez M, Pomes J, Tomas X, Peidro L. Double-bundle versus single-bundle ACL reconstruction using the horizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2010;18:32–36. doi: 10.1007/s00167-009-0844-7. [DOI] [PubMed] [Google Scholar]
- 50.Muneta T, Sekiya I, Ogiuchi T, Yagishita K, Yamamoto H, Shinomiya K. Objective factors affecting overall subjective evaluation of recovery after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 1998;8:283–289. doi: 10.1111/j.1600-0838.1998.tb00484.x. [DOI] [PubMed] [Google Scholar]


